Classification and causes of hyperparathyroidism
There are four types of hyperparathyroidism:
- pseudohyperparathyroidism;
- tertiary;
- secondary;
- primary.
Clinical manifestations in all types are similar - calcium is washed out of the inert system, hypercalcemia develops.
In primary hyperparathyroidism, the disease can have various forms. Primary hyperparathyroidism is caused by a primary pathology of the parathyroid gland. Typically, the cause of primary hyperparathyroidism is an organ tumor. Less common are multiple adenomas, and even less common is a malignant tumor. These processes are typical mainly for older people and women before menopause. Rarely they will be characteristic of young people, usually then combined with other diseases.
Primary hyperparathyroidism is divided into 3 types:
- Primary subclinical hyperparathyroidism.
There are two types of this disease:
- asymptomatic;
- biochemical.
- Primary hyperparathyroidism is clinical.
- bone. Limbs become deformed, and if the disease occurs, a person may remain disabled. Fractures occur without injury, they recover slowly, bone tissue density decreases, and osteoporosis develops.
- visceropathic form;
- renal: severe urolithiasis, prolonged colic and kidney failure are observed;
- mixed;
- gastrointestinal, diseases such as pancreatitis, duodenal ulcer and stomach ulcers, cholecystitis may occur.
The following types can be distinguished, depending on the symptoms:
This disease develops in the parathyroid glands in the presence of:
- tumors (adenomas);
- enlarged gland (hyperplasia);
- cancer (tumor), is hormonal in nature, occurs in one percent of diseases.
In ten percent of situations in patients, hyperparathyroidism occurs in combination with tumors that are hormonal in nature. These diseases include: thyroid cancer, pheochromocytoma.
Hyperparathyroidism (primary) is often hereditary.
Affected Populations
Estimates of the incidence and prevalence of primary hyperparathyroidism around the world vary. Most people with this disease, more than 80% of the world, have no symptoms. Individuals with symptoms, especially severe ones, are less common in developed countries. Primary hyperthyroidism can occur at any age, but most often affects people over 50 years of age. The incidence is highest among African-Americans, followed by Caucasians. Women are affected approximately three times more often than men.
The incidence of PHPT is 20-200 new observations per 100,000 population. In the United States, there are about 100,000 cases annually, a rate of 15.4 per 100,000, and among older adults the rate is 150 per 100,000. In Europe the rate is higher, with an average of 300 cases per 100,000 people.
Secondary hyperparathyroidism
Hyperparathyroidism (secondary) can be caused by a reduced composition of Ca in the blood, when the cause of this is other diseases, and the parathyroid glands themselves remain healthy.
In this case, the following are distinguished:
- intestinal;
- renal form.
An increase in parathyroid hormone synthesis occurs:
- with renal failure;
- with a lack of vitamin D;
- during malabsorption disease.
In 50-70% of cases, patients who are on hemodialysis suffer from secondary hyperparathyroidism. The likelihood of developing the syndrome increases for patients who have undergone gastrectomy. In addition, hypocalcemia also occurs in patients with severe liver diseases, vitamin D metabolism disorders, rickets-like diseases and rickets.
Nervous system
The higher the concentration of calcium in the blood plasma, the more pronounced disorders of the nervous system and psyche. Patients complain of the following pathological manifestations:
- apathy;
- lethargy;
- headache;
- sad mood;
- anxiety;
- drowsiness;
- decreased memory and thinking abilities.
In severe cases, patients experience psychotic disorders with clouding of consciousness, delusions and hallucinations.
Ectopic hyperparathyroidism
Ectopic hyperparathyroidism or pseudohyperparathyroidism occurs in tumors of a malignant type (breast cancer and bronchogenic), which have the ability to create parathyroid hormones, in the presence of adenomatosis of the second and first types.
The appearance of the disease hyperparathyroidism occurs due to an excess amount of parathyroid hormone, as a result of which it removes calcium and phosphorus from bone tissue. At the same time, the bones lose their structure, they become soft, curvature is observed, and fractures can occur more often than would be the case under normal conditions.
Hypercalcemia (calcium content in the blood is too high) provokes muscle weakness and excess calcium is excreted in the urine. Constant urination is accompanied by severe thirst, nephrolithiasis (kidney disease) appears, calcium salts are formed in the kidneys.
During the disease hyperparathyroidism, arterial hypertension may occur as a result of the effects of excess calcium on the blood vessels.
Symptoms of hyperparathyroidism
Hyperparathyroidism can only be determined through diagnosis, as it may not have symptoms. Clinical manifestations will depend on what is most affected - kidneys, bones, gastrointestinal tract, neurological, mental spheres.
During hyperparathyroidism, a patient may immediately develop several symptoms that are associated with damage to various organs. Diseases such as stomach ulcers, urolithiasis, osteoporosis and others may appear.
The initial symptoms of the disease include:
- fatigue;
- muscles become weaker;
- headache;
- Difficulties may arise when moving (during long distances and when climbing);
- gait becomes waddling;
- patients have poor memory;
- depression is often observed;
- imbalance;
- general lethargy;
- there is constant anxiety;
- elderly patients experience severe disorders of a psychological nature;
- During prolonged hyperparathyroidism, the skin becomes gray;
- foot pain;
- loosening and loss of healthy teeth;
- thirst;
- excessive urination;
- significant weight loss.
During the disease, in the later stages, the arms and legs, as well as the spine, often hurt. With osteoporosis, jaws can become loose and you can lose teeth that are completely healthy. The human skeleton becomes deformed and becomes shorter. Fractures due to the disease do not heal quickly, even with the appearance of false joints. Periarticular calcifications occur during illness. They are formed in the upper and lower extremities. An adenoma forms in the cervical area where the parathyroid glands are located.
There are no characteristic symptoms during visceropathic hyperparathyroidism, but they may be:
- vomit;
- pain in the stomach;
- flatulence;
- nausea;
- poor appetite and weight loss.
Patients often suffer from peptic ulcers. They are accompanied by bleeding, and serious exacerbations of diseases appear. Symptoms of gallbladder and pancreas disease occur. The disease polyuria is accompanied by symptoms of severe thirst, and the density of urine becomes less. In the later stages of the disease, renal failure and nephrocalcinosis are observed, and uremia subsequently develops.
During hypercalcemia and hypercalciuria, sclerosis of vascular calcification is observed, which subsequently leads to disruption of organ nutrition. In the blood, Ca will be in an increased composition, the condition of the cardiovascular system worsens, the pressure rises and angina pectoris appears. A syndrome called “red eye” can occur with calcification.
Patients suffer from impaired mental activity, drowsiness, fatigue, decreased mental abilities are observed, auditory or visual hallucinations may appear, and the reproduction of voluntary movements is completely lost.
Initial symptoms
At an early stage, the disease may occur without severe symptoms. At the beginning of the pathology, PTH secretion is slightly increased. As a result, dysfunction of the parathyroid glands is detected late, when the patient has already suffered serious damage to the bones and internal organs. The disease can be diagnosed at an early stage only with a blood test for hormones.
The first signs of an endocrine disorder appear with a significant increase in the secretion of parathyroid hormone. Symptoms and treatment of primary hyperparathyroidism in women and men depend on the form of the disease. However, it is possible to identify common initial signs of pathology:
- Fatigue and muscle weakness. Increased calcium concentration leads to muscle weakness. Patients get tired quickly and have difficulty walking for a long time. It often becomes difficult for patients to get up from a chair without support or enter the door of public transport.
- Musculoskeletal pain. This is the initial sign of calcium being washed out of the tissues. Most often pain occurs in the feet. Characterized by a “duck” gait. Due to pain, patients walk, swaying from one foot to the other.
- Frequent urination and thirst. With primary hyperparathyroidism, patients have increased urinary calcium excretion. This leads to damage to the kidney tubules. The tissues of the excretory organ lose sensitivity to the pituitary hormone vasopressin, which regulates diuresis.
- Deterioration of dental condition. This early manifestation of pathology is associated with calcium deficiency. Often the first sign of the disease is loosening and loss of teeth, as well as rapidly progressing caries.
- Weight loss, change in skin color. The weight of patients in the first months of the disease can decrease by 10 - 15 kg. Increased diuresis leads to severe dehydration, which causes weight loss. Patients' skin becomes excessively dry and takes on a grayish or sallow tone.
- Neuropsychic disorders. Hypercalcemia leads to deterioration of brain tissue. Patients experience frequent headaches, mood swings, increased anxiety and depression.
Patients do not always associate such symptoms with endocrine disorders. Therefore, visiting a doctor is often postponed.
At the advanced stage of pathology, the clinic of primary hyperparathyroidism is characterized by severe damage to bone tissue, blood vessels and internal organs. An increase in parathyroid hormone secretion leads to a sharp deterioration in the patient's condition. Next, we will consider in detail the pathological manifestations of various organs and systems.
Diagnosis of hyperparathyroidism
At the stage of primary hyperparathyroidism, specific symptoms may not appear and it will be difficult to establish a diagnosis, but a comprehensive diagnosis can cope with this task.
The results are based on the following surveys:
- power analysis (general).
- examination for biochemistry (pathogen hormone, P, Ca).
- Ultrasound examination.
- MRI and CT, X-ray examination.
- scintigraphy.
It is determined how much calcium is excreted from the urine and the composition of P in it.
The composition of Ca in the blood increases, the composition of P is less than necessary, and increased phosphatase activity. The most significant indicator for the disease will be the composition of parathyroid hormone (from 5 to 8 ng/ml and more if the composition is from 0.15 to 1 ng/ml) in the blood.
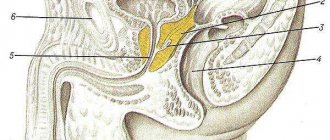
Using ultrasound, the parathyroid gland is examined for the location of parathyroid adenomas.
The study helps determine changes in the bones, as well as fractures and osteoporosis. Densitometry is necessary to determine bone density. X-ray examination allows you to diagnose the appearance of peptic ulcers in the stomach and intestines. A CT scan of the kidneys and bladder can help identify stones. It is also possible to identify the location of parathyroid adenoma in the retrosternal space. MRI is much better than ultrasound and CT scan as it can detect various changes that occur in the thyroid glands.
Detects changes in the parathyroid glands. The examination is carried out for secondary hyperparathyroidism.
Complications of hyperparathyroidism
Hypercalcemic crisis is one of the most severe complications that can threaten the patient. Risk factors include: taking vitamins D and calcium, as well as thiazide diuretics (reduce calcium in the urine) in excess amounts, prolonged bed rest. With hypercalcemia, a crisis can occur instantly (Ca in the blood is from 3.5 to 5 mmol/l, with a composition from 2.15 to 2.50 mmol/l), and acute symptoms occur.
In this condition, an increased body temperature of 39-40 ° C, vomiting, pain in the epigastrium, drowsiness, and coma may be observed. The feeling of weakness in the body quickly increases and dehydration appears. Serious complications may occur: muscle atrophy and intercostal muscle diaphragms develop. Peptic ulcers (blood), thrombosis, perforation, and pulmonary edema appear.
When this complication occurs, the mortality rate is 60% or higher.
It can be provoked by: pregnancy, infections, dehydration, intoxication, massive release of calcium into the blood, advanced state of primary hyperparathyroidism.
Forecast
In the absence of treatment and severe course of the disease, disability occurs. Life-threatening is hypercalcemic crisis , the mortality rate of which reaches 60%. Detection of the disease at an early stage and timely surgical treatment prevent the occurrence of osteovisceral complications.
After surgery, the symptoms of the disease disappear, recovery occurs in 90% of cases. During the first year after surgery, bone mineral density increases by 15-25%.
Treatment of hyperparathyroidism
Hyperparathyroidism will require urgent treatment. The main treatment will be surgical intervention; in case of a hypercalcemic crisis, intervention is carried out on an emergency basis. Most of the time is spent finding tumors during surgery. If a visceropathic form of the disease is detected, which is confirmed by examination (high concentration of parathyroid hormone), then in this case the operation is performed even without topical diagnostics.
Surgery is one of the main methods to save the patient if the diagnosis is hyperparathyroidism or its primary form.
If patients are over fifty years of age, the operation is performed:
- upon detection of progressive osteoporosis;
- if the creatinine norm of the age norm is less than thirty percent;
- if the Ca composition is above 3 mmol/l, if there are acute symptoms of hypercalcemia;
- if there are complications caused by primary hyperparathyroidism.
When deciding not to undergo surgery, patients should drink the amount of fluid they need and move more so that physical inactivity does not occur. Cardiac glycosides and thiazide diuretics are contraindicated during treatment. You also need to monitor blood pressure; if patients are postmenopausal, estrogens are prescribed. After six months you need to undergo an examination. It is this that will allow us to determine the composition of plasma creatinine, calcium, and creatinine clearance. Every year, conduct an examination of the abdominal part using an ultrasound method.
With hyperplasia of the parathyroid glands, gland replantation is necessary. They are removed and fiber is added to the forearm.
Prognosis of hyperparathyroidism
It is possible to make predictions about the disease only if the disease was diagnosed at the initial stage and treatment was carried out on time.
Restoration of working capacity after treatment in a patient with bone hyperparathyroidism is associated with how much bone tissue was damaged. If the disease was mild, the patient can recover after four months after treatment; in severe cases, recovery occurs within two years. If the disease is advanced, the ability to work will be limited.
Renal hyperparathyroidism is a more severe disease. Recovery primarily depends on how damaged the kidneys were before surgery. If the operation is not performed, patients may remain disabled or die from kidney failure.
Prognosis of hyperparathyroidism
It is possible to make predictions about the disease only if the disease was diagnosed at the initial stage and treatment was carried out on time.
Restoration of working capacity after treatment in a patient with bone hyperparathyroidism is associated with how much bone tissue was damaged. If the disease was mild, the patient can recover after four months after treatment; in severe cases, recovery occurs within two years. If the disease is advanced, the ability to work will be limited.
Renal hyperparathyroidism is a more severe disease. Recovery primarily depends on how damaged the kidneys were before surgery. If the operation is not performed, patients may remain disabled or die from kidney failure.
Excretory organs
With increased production of the hormone PTH, the kidneys become the second target organ after the skeletal system. Increased urinary calcium excretion causes tubular damage. In the early stages, this manifests itself in increased urination and thirst. Over time, stones form in the organ, which is accompanied by attacks of renal colic.
The more pronounced the signs of kidney damage, the more unfavorable the prognosis of the disease. In severe cases, patients develop edema and develop renal failure, which is irreversible.