Feces, like urine, are the end product of human life. It is formed in the large intestine as a result of a number of biochemical processes. Feces include water, undigested food debris, metabolic byproducts, bacteria, and so on.
Do not underestimate stool testing. Sometimes it is this analysis that makes it possible to identify pathologies of the digestive tract, liver disease, and pancreas in adults and children. This examination is prescribed not only for the purpose of diagnosing diseases, but also to monitor the treatment being carried out.
What a coprogram (stool analysis) shows:
- study of the physical and chemical properties of feces (color, consistency);
- microscopy of material;
- bacteriological examination (detection of pathogenic microbes and analysis of intestinal microflora);
- detection of helminth eggs;
- detection of occult blood in the stool.
general description
Feces are formed in the large intestine. It consists of water, remnants of food taken and secretions of the gastrointestinal tract, products of the transformation of bile pigments, bacteria, etc. For the diagnosis of diseases associated with the digestive organs, stool examination in some cases can be crucial. A general stool analysis (coprogram) includes macroscopic, chemical and microscopic examination.
How to donate feces: preparation and collection rules
It is very important to carefully consider the doctor’s recommendations regarding preparation for the study; the accuracy of decoding the results of the coprogram depends on this, and hence the correct diagnosis.
So, let's look at how to submit feces for analysis correctly:
- Even at the stage of receiving a referral, you must inform your doctor about all the medications that you have used in recent weeks or are currently taking, as well as about all diagnostic procedures completed the day before. The fact is that radiopaque agents affect the composition of stool, and invasive procedures, such as colonoscopy, can lead to internal damage and bleeding from the intestines. Unwanted medications include antibiotics, anthelmintic and laxatives, activated carbon, iron and bismuth preparations, rectal suppositories and many other medications, so it is better to warn the doctor about all of them in advance;
- 3-5 days before the scatological examination, it is necessary to adjust your diet - remove from it dishes and foods that color the stool in uncharacteristic colors (beets, red and black berries, carrots, spinach). It is quite possible that the doctor will ask you to switch to a special diet, which will clarify the existing problems with the functioning of certain digestive organs. For example, a doctor may recommend that for several days you eat mainly cereals, dairy products, raw vegetables and fruits, protein foods, and so on;
- Immediately before collecting stool for coprogram, you need to urinate, because otherwise, during defecation, urine will likely be released from the bladder and get into the sample for research, and this should not be allowed. Then you need to perform an intimate toilet - thoroughly wash the perineum with soap, paying special attention to the perianal area, rinse and wipe dry;
- It is not recommended to collect feces for analysis directly from the toilet - there will either be large quantities of pathogenic bacteria or traces of aggressive detergents. It is better to prepare a convenient container (an old saucepan, bowl), wash it thoroughly, pour boiling water over it and defecate there. The coprogram for children is taken from a clean potty, for infants - from a diaper or oilcloth; you should not collect a sample from a diaper, since the filler may contain chemical impurities that distort the interpretation of the research results;
- Defecation should occur spontaneously and naturally - you cannot stimulate the intestines with drugs or give an enema. Stool obtained in this way is not suitable for analysis. When the process is complete, immediately collect samples from different parts of the feces, especially those areas that are different in color or consistency or have suspicious inclusions. A special plastic container with a spoon, which can be purchased at a pharmacy, is best suited for collecting stool. To conduct a scatological study, approximately 20 g of material is needed;
- The stool sample must be delivered to the laboratory within a maximum of 2 hours after collection, with the lid of the container immediately tightly closed to prevent open air from influencing the composition of the stool. Preliminary storage of the material in the refrigerator at a temperature not exceeding -5 °C Celsius and no longer than 12 hours is allowed. However, the sooner you bring feces for examination, the more objective the results will be.
Macroscopic examination
Quantity
In pathology, the amount of feces decreases with prolonged constipation caused by chronic colitis, peptic ulcers and other conditions associated with increased absorption of fluid in the intestines. With inflammatory processes in the intestines, colitis with diarrhea, and accelerated evacuation from the intestines, the amount of feces increases.
Consistency
Thick consistency - with constant constipation due to excessive absorption of water. Liquid or mushy consistency of stool - with increased peristalsis (due to insufficient absorption of water) or with abundant secretion of inflammatory exudate and mucus by the intestinal wall. Ointment-like consistency - in chronic pancreatitis with exocrine insufficiency. Foamy consistency - with enhanced fermentation processes in the large intestine and the formation of a large amount of carbon dioxide.
Form
The form of feces in the form of “large lumps” - when feces remain in the colon for a long time (hypomotor dysfunction of the colon in people with a sedentary lifestyle or who do not eat rough food, as well as in cases of colon cancer, diverticular disease). The form in the form of small lumps - “sheep feces” indicates a spastic state of the intestines, during fasting, stomach and duodenal ulcers, a reflex nature after appendectomy, with hemorrhoids, anal fissure. Ribbon or “pencil” shape - for diseases accompanied by stenosis or severe and prolonged spasm of the rectum, for rectal tumors. Unformed feces are a sign of maldigestion and malabsorption syndrome.
Color
If staining of stool by food or drugs is excluded, then color changes are most likely due to pathological changes. Grayish-white, clayey (acholic feces) occurs with obstruction of the biliary tract (stone, tumor, spasm or stenosis of the sphincter of Oddi) or with liver failure (acute hepatitis, cirrhosis of the liver). Black feces (tarry) - bleeding from the stomach, esophagus and small intestine. Pronounced red color - with bleeding from the distal parts of the colon and rectum (tumor, ulcers, hemorrhoids). Gray inflammatory exudate with fibrin flakes and pieces of the colon mucosa (“rice water”) - with cholera. The jelly-like character is deep pink or red in amoebiasis. In typhoid fever, the stool looks like “pea soup.” With putrefactive processes in the intestines, the feces are dark in color, with fermentative dyspepsia - light yellow.
Slime
When the distal colon (especially the rectum) is affected, the mucus occurs in the form of lumps, strands, ribbons, or a glassy mass. With enteritis, the mucus is soft, viscous, mixing with feces, giving it a jelly-like appearance. Mucus, covering the outside of formed feces in the form of thin lumps, occurs with constipation and inflammation of the large intestine (colitis).
Blood
When bleeding from the distal parts of the colon, the blood is located in the form of streaks, shreds and clots on formed stool. Scarlet blood occurs when bleeding from the lower parts of the sigmoid and rectum (hemorrhoids, fissures, ulcers, tumors). Black feces (melena) occur when there is bleeding from the upper digestive system (esophagus, stomach, duodenum). Blood in the stool can be found in infectious diseases (dysentery), ulcerative colitis, Crohn's disease, disintegrating colon tumors.
Pus
Pus on the surface of the stool occurs with severe inflammation and ulceration of the mucous membrane of the colon (ulcerative colitis, dysentery, disintegration of an intestinal tumor, intestinal tuberculosis), often together with blood and mucus. Large amounts of pus without mucus are observed when opening paraintestinal abscesses.
Leftover undigested food (lientorrhea)
The release of undigested food residues occurs with severe insufficiency of gastric and pancreatic digestion.
Answers to frequently asked questions about coprogram
- How much does a stool test for coprogram cost? The price depends on the region and the policies of private clinics; on average, a scatological examination in a good medical center will cost you 350-1000 rubles. In a public clinic, you can donate feces free of charge if you have relevant complaints and after presenting your compulsory health insurance policy;
- How long to wait for the result? Medical institutions that provide services to the population on a commercial basis, as a rule, do this very quickly - they provide a transcript of the coprogram the very next day. After 1-3 days, laboratories at clinics transfer the finished analysis form directly to the doctor to whom the patient turned - usually a local therapist or pediatrician. Therefore, you will be able to find out the results of the study as soon as you attend your next appointment;
- Is it possible to freeze and test yesterday's stool? Yes, this is completely acceptable. Everyone has their own biorhythms - there are people who habitually empty their bowels in the evenings, but in the morning they don’t really feel like going to the toilet at all. With young children, especially infants, coprogram sometimes becomes an impossible task if you try to collect fresh morning feces and immediately deliver it to the laboratory;
- Is it necessary to donate stool in a special container? No, but it meets all hygienic requirements, is easy to use and inexpensive. Private clinics usually issue such containers along with a referral for coprogram; their price is included in the total cost of the service. And in a state laboratory they will take your stool in any suitable container - a small sealed jar made of plastic or glass, but they will ask if you washed it well;
- How much feces should be submitted for coprogram? A volume approximately equal to one teaspoon is sufficient, but it is better to collect a sample from different parts of the stool, so that it becomes possible to evaluate the composition and properties of feces as objectively as possible. If you use a special container with a spoon, then scoop 3-5 servings from the top, side and middle of the feces;
- Is it possible to do a coprogram during menstruation? It is not advisable, it is better to wait until the end of menstrual bleeding to be sure that blood will not get into the sample being studied and will not distort the decoding of the coprogram. If there are urgent indications or a threatening health condition, then a stool test can be taken, but during defecation it is necessary to securely close the entrance to the vagina with a hygienic tampon or sterile cotton wool;
- Is it true that you can’t have anal sex before coprogram? Yes, this is true, and not all doctors, due to the sensitivity of this topic, warn patients about the need to temporarily refrain from such pleasures. During anal sex, bleeding injuries to the rectum may occur, and even if they are microscopic, deciphering the coprogram will give a false positive test result for occult blood;
- Is what a coprogram shows always enough to make a correct diagnosis? No, this is a basic test that allows you to suspect a problem and outline a further examination strategy. Very often, based on the results of scatology, the patient is referred for bacteriological analysis of stool, ultrasound of the abdominal organs, X-ray contrast tomography, colonoscopy, sigmoidoscopy and other diagnostic procedures.
Chemical research
Fecal reaction
An acidic reaction (pH 5.0-6.5) is observed when iodophilic flora is activated, producing carbon dioxide and organic acids (fermentative dyspepsia). An alkaline reaction (pH 8.0-10.0) occurs with insufficient digestion of food, with colitis with constipation, sharply alkaline with putrefactive and fermentative dyspepsia.
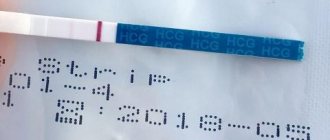
Reaction to blood (Gregersen reaction)
A positive reaction to blood indicates bleeding in any part of the gastrointestinal tract (bleeding from the gums, rupture of varicose veins of the esophagus, erosive and ulcerative lesions of the gastrointestinal tract, tumors of any part of the gastrointestinal tract in the stage of decay).
Reaction to stercobilin
The absence or sharp decrease in the amount of stercobilin in the feces (the reaction to stercobilin is negative) indicates obstruction of the common bile duct with a stone, compression by a tumor, stricture, stenosis of the common bile duct, or a sharp decrease in liver function (for example, in acute viral hepatitis). An increase in the amount of stercobilin in feces occurs with massive hemolysis of red blood cells (hemolytic jaundice) or increased bile secretion.
Reaction to bilirubin
The detection of unchanged bilirubin in the stool of an adult indicates a disruption in the process of bilirubin recovery in the intestine under the influence of microbial flora. Bilirubin can appear during rapid evacuation of food (sharp increase in intestinal motility), severe dysbiosis (syndrome of bacterial overgrowth in the colon) after taking antibacterial drugs.
Vishnyakov-Triboulet reaction (for soluble protein)
The Vishnyakov-Triboulet reaction is used to identify a hidden inflammatory process. The detection of soluble protein in stool indicates inflammation of the intestinal mucosa (ulcerative colitis, Crohn's disease).
Features of decoding coprograms in children
The main indicators of coprogram in children are similar to those in adults. But there are some peculiarities.
Most children have a normal coprogram with a neutral or slightly alkaline reaction (in the pH range 6-7.6.
Please note: in infants, the reaction is most often sour in nature, as a result of the nutritional characteristics characteristic of this age category.
An alkaline reaction in children is determined when the absorption process is disrupted, with increased putrefactive processes in the intestines, and prolonged presence of undigested food in the stomach and intestines.
Until a child is three months old when breastfeeding, the presence of bilirubin in the stool is normal. After 3 months, only stercobilin should normally be determined in deciphering the coprogram in children.
Lotin Alexander, medical columnist
99, total, today
( 49 votes, average: 4.43 out of 5)
Pipelle biopsy of the endometrium with histological examination: what it is, how it is performed, indications, contraindications, complications
MRI during pregnancy: is it possible or not?
Related Posts
Microscopic examination
Muscle fibers - with striations (unchanged, undigested) and without striations (changed, digested). A large number of changed and unchanged muscle fibers in the feces (creatorrhoea) indicates a violation of proteolysis (protein digestion):
- in conditions accompanied by achlorhydria (lack of free HCl in gastric juice) and achylia (complete absence of secretion of HCl, pepsin and other components of gastric juice): atrophic pangastritis, a condition after gastric resection;
- with accelerated evacuation of food chyme from the intestines;
- in case of violation of the exocrine function of the pancreas;
- with putrefactive dyspepsia.
Connective tissue (remnants of undigested vessels, ligaments, fascia, cartilage). The presence of connective tissue in the feces indicates a deficiency of proteolytic enzymes of the stomach and is observed with hypo- and achlorhydria, achylia.
Fat is neutral. Fatty acid. Salts of fatty acids (soaps)
The appearance of large amounts of neutral fat, fatty acids and soaps in the stool is called steatorrhea. This happens:
- with exocrine pancreatic insufficiency, a mechanical obstruction to the outflow of pancreatic juice, when steatorrhea is represented by neutral fat;
- if the flow of bile into the duodenum is impaired and if the absorption of fatty acids in the small intestine is impaired, fatty acids or salts of fatty acids (soaps) are found in the feces.
Plant fiber
Digestible - found in the pulp of vegetables, fruits, legumes and grains. Indigestible fiber (the skin of fruits and vegetables, plant hairs, the epidermis of cereals) has no diagnostic value, since there are no enzymes in the human digestive system that break it down. It is found in large quantities during rapid evacuation of food from the stomach, achlorhydria, achylia, and the syndrome of bacterial overgrowth in the colon.
Starch
The presence of a large amount of starch in the feces is called amilorrhea and is observed more often with increased intestinal motility, fermentative dyspepsia, and less often with exocrine insufficiency of pancreatic digestion.
Iodophilic microflora (clostridia)
With a large amount of carbohydrates, clostridia multiply intensively. A large number of clostridia is regarded as fermentative dysbiosis.
Epithelium
A large amount of columnar epithelium in the feces is observed in acute and chronic colitis of various etiologies.
Leukocytes
A large number of leukocytes (usually neutrophils) are observed in acute and chronic enteritis and colitis of various etiologies, ulcerative necrotic lesions of the intestinal mucosa, intestinal tuberculosis, and dysentery.
Red blood cells
The appearance of slightly changed red blood cells in the stool indicates the presence of bleeding from the colon, mainly from its distal parts (ulceration of the mucous membrane, disintegrating tumor of the rectum and sigmoid colon, anal fissures, hemorrhoids). A large number of red blood cells in combination with leukocytes and columnar epithelium is characteristic of ulcerative colitis, Crohn's disease with damage to the colon, polyposis and malignant neoplasms of the colon.
Worm eggs
Eggs of roundworms, tapeworms, etc. indicate a corresponding helminthic infestation.
Pathogenic protozoa
Cysts of dysenteric amoeba, Giardia, etc. indicate a corresponding invasion by protozoa.
Yeast cells
Found in feces during treatment with antibiotics and corticosteroids. Identification of the fungus Candida albicans is carried out by culturing on special media (Sabouraud's medium, Microstix Candida) and indicates a fungal infection of the intestine.
Calcium oxalate (oxalic lime crystals)
Detection of crystals is a sign of achlorhydria.
Triple phosphate crystals (ammonium phosphate-magnesia)
Triple phosphate crystals found in feces (pH 8.5-10.0) immediately after defecation indicate increased protein putrefaction in the colon.
Classification of steatorrhea
Detection of shine in stool is a reason to immediately consult a doctor. The disease exists in several varieties:
- nutritional (food) steatorrhea,
- pancreatic steatorrhea,
- intestinal steatorrhea.
The classification of steatorrhea depends on the nature of the fatty acids.
- Nutritional diarrhea is caused by the quality of food consumed. When more fat enters the body than it can process, the excess is excreted in the feces. This natural elimination of excessively consumed fatty foods is diagnosed most often among other forms of steatorrhea (fatty stool). Food diarrhea is observed when poisoned by foods containing triglycerides.
- The pancreatic form is more difficult to tolerate. With such steatorrhea, it is not the intestines that suffer, but the pancreas. The body stops producing lipase, which performs the function of breaking down fats. The absence of the enzyme causes loose stools.
- With intestinal steatorrhea, disorders occur in the small intestine. In this section, fatty foods cease to be absorbed. Fat molecules are not absorbed and are released into the feces. A prerequisite may be unhealthy diet and gastrointestinal pathologies.
Norms
Macroscopic examination
| Parameter | Norm |
| Quantity | A healthy person produces an average of 100-200 g of feces per day. Normally, feces contain about 80% water and 20% dry matter. With a vegetarian diet, the amount of feces can reach 400-500 g per day; when using easily digestible food, the amount of feces decreases. |
| Consistency | Normally, formed feces have a dense consistency. Pasty feces can occur normally and are caused by the intake of predominantly plant foods. |
| Form | Normally cylindrical. |
| Smell | Normally, stool has a mild odor, which is called fecal (ordinary). It may intensify with the predominance of meat products in the diet, with putrefactive dyspepsia and weaken with a dairy-vegetable diet, constipation. |
| Color | Normally, stool is brown in color. When eating dairy foods, stool turns yellowish-brown, and meat stool turns dark brown. Ingestion of plant foods and some medications can change the color of stool (beets - reddish; blueberries, blackcurrants, blackberries, coffee, cocoa - dark brown; bismuth, iron color stool black). |
| Slime | Normally absent (or in scanty quantities). |
| Blood | Normally absent. |
| Pus | Normally absent. |
| Leftover undigested food (lientorrhea) | Normally none. |
Chemical research
| Parameter | Norm |
| Fecal reaction | Normally neutral, less often slightly alkaline or slightly acidic. Protein nutrition causes a shift in the reaction towards the alkaline side, while carbohydrate nutrition causes the reaction to shift towards the acidic side. |
| Reaction to blood (Gregersen reaction) | Normally negative |
| Reaction to stercobilin | Normally positive. |
| Reaction to bilirubin | Normally negative. |
| Vishnyakov-Triboulet reaction (for soluble protein) | Normally negative. |
Microscopic examination
| Parameter | Norm |
| Muscle fibers | Normally absent or single in the field of view. |
| Connective tissue (remnants of undigested vessels, ligaments, fascia, cartilage) | Normally absent. |
| Fat is neutral. Fatty acid. Salts of fatty acids (soaps). | Normally there are no or scanty amounts of fatty acid salts. |
| Plant fiber | Normally, there are single cells in the p/z. |
| Starch | Normally absent (or single starch cells). |
| Iodophilic microflora (clostridia) | Normally, single in rare areas (normally, iodophilic flora lives in the ileocecal region of the large intestine). |
| Epithelium | Normally, there are no or single columnar epithelial cells in the p/z. |
| Leukocytes | Normally, there are no or single neutrophils in the p/z. |
| Red blood cells | Normally none. |
| Worm eggs | Normally none. |
| Pathogenic protozoa | Normally none. |
| Yeast cells | Normally none. |
| Calcium oxalate (oxalic lime crystals) | Normally none. |
| Triple phosphate crystals (ammonium phosphate-magnesia) | Normally none. |
Preparatory activities
To obtain accurate results, experts recommend going on a diet a few days before taking a general stool test. This measure will help to avoid inaccurate decoding of the received data.
Preparing for coprogram involves following a therapeutic diet
Table 3. Diet options
| Diet | Daily norm |
| Schmidt. |
|
| Pevzner. |
|
Pevzner's principle of nutrition is to increase the food load on the human body. In the presence of acute inflammatory processes or dysfunction of the gastrointestinal tract, the use of this method is not recommended.
Types of diets according to Pevzner M.I.
Diseases for which a doctor may prescribe a general stool test (coprogram)
Anal fissure
With an anal fissure, feces may take the form of small lumps (“sheep feces” indicates a spastic condition of the intestines). Due to bleeding, scarlet blood and slightly changed red blood cells may be present in the stool.
Crohn's disease
With Crohn's disease, you may find blood in your stool. The Vishnyakov-Triboulet reaction reveals soluble protein in it. Crohn's disease affecting the colon is characterized by the presence in the feces of a large number of red blood cells in combination with leukocytes and columnar epithelium.
Colon diverticulosis
With diverticular disease, due to the long stay of stool in the colon, it takes the form of “large lumps”.
Duodenal ulcer
With a duodenal ulcer, the feces have the form of small lumps (“sheep feces” indicates a spastic condition of the intestines).
Stomach ulcer
With a stomach ulcer, the feces have the form of small lumps (“sheep feces” indicates a spastic condition of the intestines).
Chronic pancreatitis
In chronic pancreatitis with exocrine insufficiency, stool may have a pasty consistency.
Hemolytic anemia
With hemolytic jaundice (anemia), due to massive hemolysis of red blood cells, the amount of stercobilin in the feces increases.
Benign neoplasms of the colon
With a tumor accompanied by bleeding from the distal colon, the stool may have a pronounced red color. With disintegrating colon tumors, blood may be found in the stool. Pus on the surface of the stool occurs when there is severe inflammation and ulceration of the colon mucosa (disintegration of an intestinal tumor), often along with blood and mucus. When a colon tumor is in the stage of decay due to bleeding, the reaction to blood (Gregersen reaction) is positive.
Intestinal helminthiases
With helminthic infestation, the feces contain eggs of roundworms, tapeworms, etc.
Cirrhosis of the liver
In liver failure, including liver cirrhosis, the stool is grayish-white, clayey (acholic).
Ulcerative colitis
With colitis, there is mucus covering the outside of the stool in the form of thin lumps. With ulcerative colitis, blood may be found in the stool; pus on the surface of the stool, often along with blood and mucus; soluble protein in the Vishnyakov-Triboulet reaction; a large number of leukocytes (usually neutrophils); a large number of red blood cells in combination with leukocytes and columnar epithelium.
Constipation
With prolonged constipation caused by chronic colitis, peptic ulcers and other conditions associated with increased absorption of fluid in the intestine, the amount of feces decreases. With constant constipation due to excessive absorption of water, the consistency of stool is dense. With constipation, there may be mucus covering the outside of the stool in the form of thin lumps.
Malignant neoplasm of the colon
The form of feces in the form of “large lumps” - when feces remain in the colon for a long time - is noted in colon cancer. Pronounced red color of stool - with a tumor accompanied by bleeding from the distal parts of the colon and rectum. Blood in the stool can be found in disintegrating colon tumors. Pus on the surface of the stool occurs when there is severe inflammation and ulceration of the colon mucosa (disintegration of an intestinal tumor), often along with blood and mucus. A positive reaction to blood (Gregersen reaction) indicates bleeding with a tumor of the colon in the stage of decay. A large number of red blood cells in combination with leukocytes and columnar epithelium is characteristic of malignant neoplasms of the colon.
Irritable bowel syndrome, chronic colitis
With colitis with diarrhea, the amount of feces increases. The amount of feces decreases with prolonged constipation caused by chronic colitis. Mucus covering the outside of formed feces in the form of thin lumps is found in colitis. An alkaline reaction (pH 8.0-10.0) occurs in colitis with constipation. A large number of leukocytes (usually neutrophils) are observed in colitis of various etiologies.
Cholera
In cholera, stool looks like a gray inflammatory exudate with fibrin flakes and pieces of the colon mucosa (“rice water”).
Amoebiasis
With amebiasis, the stool is jelly-like, deep pink or red.
Typhoid fever
In typhoid fever, the stool looks like “pea soup.”
Complications of the disease
Complications of steatorrhea occur in case of improper treatment or its complete absence. The following may develop:
- Disturbances in the functioning of the vascular system, heart, genitourinary, endocrine, and nervous systems.
- Increased intestinal barrier permeability.
- Disturbance of protein metabolism, which leads to weight loss, ascites, and a decrease in the amount of total protein in the body.
- Hypovitaminosis. It, in turn, is accompanied by frequent dizziness, pain in the joints and spine, swelling, convulsions, dryness, pallor of the mucous membranes, itching, decreased visual acuity, splitting of the nails, fragility and dullness of the hair, stomatitis, glossitis, looseness of the gum surfaces.
Prevention
If the appearance of white streaks in the stool is due to the presence of a disease that was subsequently cured, then you should take care of your body to prevent this from happening again.
The following can be done as preventive measures:
- carefully monitor food, avoiding eating expired food;
- it is recommended to adhere to a healthy diet and refuse (or at least limit) the consumption of any foods that are “heavy” for the digestive system, that is, anything fatty, spicy or smoked;
- Maintain personal hygiene - wash your hands thoroughly, keep the room clean;
- prevent hypothermia and immediately begin treatment of any infectious diseases;
- try to prevent the occurrence of such unpleasant conditions as diarrhea or constipation, bloating or irritation of the mucous membranes;
- Periodically visit a doctor and undergo routine examinations. A timely diagnosed disease is much easier to cure than its advanced form.
The main thing to remember during treatment is that only under the guidance of a specialist can you completely get rid of the problem and minimize possible consequences.
What does mucus in stool mean?
Factors that can provoke active mucus secretion are quite diverse. Among the most common are:
- prolonged fasting;
- sudden change in food products;
- drinking raw drinking water from random sources;
- colds and infectious diseases of the respiratory tract, accompanied by copious sputum production;
- dietary nutrition, which involves daily consumption of decoctions of oats and flax seeds;
- uncontrolled use of medications;
- hypothermia, which causes inflammation of the pelvic organs and anal area.
Paying attention to your health helps eliminate or prevent negative manifestations.
Diagnostics
To draw up a detailed clinical picture, the doctor examines the patient and inquires about his diet and diet. After this, a number of events are planned:
- Analysis of stool to identify pathogenic microorganisms in it. To choose adequate treatment with antibiotics, you need to know exactly the type of causative agent of the disease.
- Studying mucus in laboratory conditions. A clinical and biochemical study is carried out to identify the level of leukocytes, indicating a progressive inflammatory process. The presence of red blood cells is also assessed.
- If damage to the stomach or duodenum is suspected, FGDS is prescribed. An ultrasound is performed to examine the abdominal organs. The list can be supplemented with an X-ray examination using contrast - a barium mixture.
- Study of the intestinal lumen through rectoscopy. This technique is indicated for suspected polyposis, neoplasms or hemorrhoids.