5 / 5 ( 1 voice )
Many of us have heard of such a diagnosis as cardiopulmonary failure (CPF), however, not everyone is familiar with its etiology, causes and consequences. This pathological process provokes disruptions in the respiratory rhythm and disorders in the cardiovascular system.
The main cause is hypertension, which develops in the pulmonary circulation. The disease is characterized by the release of blood into the pulmonary artery, which is a rather serious problem.
We will tell you about the symptoms of cardiopulmonary failure and treatment of the pathology in our dedicated editorial office.
Cardiopulmonary failure appears due to hypertension in the pulmonary circulation.
Features of the pathology
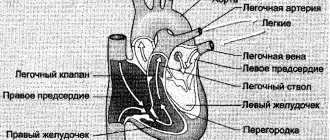
Cardiopulmonary failure is most often a malfunction of the left ventricle, which causes stagnation of blood in the lungs. This can be triggered by a change in the activity of the heart muscle after an infectious pathology or electrical discharge, blood clots in the coronary artery, or any other vascular accident.
Manifests itself in cardiogenic shock, suffocation, and pulmonary edema. The latter swell due to excess pressure in them, which leads to the filling of blood vessels in the intercellular space with liquid, disrupting the natural process of gas exchange. In acute cardiopulmonary failure, a person painfully tries to take a breath, and if he is not helped, death will occur. The attack develops suddenly at any age.
Pulmonary insufficiency: severity
Due to the fact that the chronic form of this disease is characterized by a slow and often almost imperceptible increase in pathological symptoms, four degrees of severity of the disease are determined:
- I degree – there are no signs of the disease, no manifestations of the disease are observed with habitual physical activity, and slight shortness of breath appears with increasing load.
- Stage II – symptoms do not appear at rest, but with habitual physical activity shortness of breath and rapid heartbeat appear.
- III degree – symptoms of deficiency appear with minimal physical activity, but are absent at rest.
- IV degree – a person cannot perform minimal physical activity, signs of the disease appear at rest.
An acute attack of pulmonary failure can develop in one of two ways - right and left ventricular failure. Left ventricular failure may manifest as pulmonary edema or cardiac asthma.
Reasons for development
Pulmonary heart failure does not occur out of nowhere. Usually this is a combination of pathologies that provoked such a condition. The causes of cardiopulmonary failure are divided into groups:
Vascular, including changes provoked by:
- atherosclerosis;
- compression of the heart by an aneurysm;
- blood clots in the arteries of the lungs.
Bronchopulmonary, consisting of:
- extensive pneumonia;
- tuberculosis;
- chronic bronchitis;
- bronchial asthma.
Thoradiaphragmatic, associated with obvious deformation of the chest, provoked by:
- kyphoscoliosis;
- polio;
- ankylosing spondylitis;
- abnormal structure of the diaphragm.
Classification
Pathology is classified according to the type of course:
- Acute, which is often decompensated. Often this is a consequence of massive thromboembolism of the pulmonary artery, valvular pneumothorax, mediastinal emphysema or status asthmaticus. It occurs suddenly due to an increase in pressure in the artery, which provokes an expansion of the cavity of the right ventricle, making its walls thin.
- Subacute, occurring with and without right ventricular failure. This is a consequence of any of the above reasons in combination. It develops from a month to several years, provoking pronounced myocardial hypertrophy.
- Chronic is similar to subacute, but has a less pronounced course and can develop over years.
Acute, subacute and chronic pulmonary heart failure can have the following clinical types:
- respiratory with a predominance of shortness of breath, episodic suffocation, cough, wheezing and cyanosis;
- cerebral, giving symptoms of encephalopathy from aggressiveness and psychosis to apathy;
- anginal provokes severe chest pain and suffocation;
- abdominal - nausea, vomiting, stomach ulcers and other signs of gastrointestinal hypoxia;
- collaptoid is accompanied by hypotension, pallor, weakness, tachycardia, and cold sweat.
Right ventricular failure
It can also occur as a complication of myocardial infarction or myocarditis. Its manifestations, in addition to shortness of breath and increasing suffocation, are:
- cyanosis of the face and fingers;
- the swollen neck veins are clearly visible, especially when inhaling;
- swelling of the legs, face, abdominal wall up to ascites;
- enlarged liver, pulsation in the epigastrium is observed.
Symptoms
Each form of cardiopulmonary failure has its own symptoms:
Acute, in which the patient must be immediately taken to the hospital. because the risk of death is quite high, especially in a child. It is provoked by painful shock and extensive swelling of the lungs. Symptoms:
- a sharp drop in blood pressure until collapse;
- the breathing process is difficult, superficial, it is difficult to take a breath;
- neck veins are swollen;
- the skin turns blue, especially the limbs;
- chest pain of varying severity;
- sticky sweat;
- suffocation due to lack of oxygen.
WE RECOMMEND: What are the consequences of incomplete blockade of the right bundle branch?
Chronic is easier than acute and subacute forms. Symptoms largely depend on the underlying cause. Usually this:
- arms, legs and nasolabial triangle with a bluish tint;
- severe vertigo;
- tachycardia;
- exercise causes shortness of breath;
- fatigue and weakness.
The more severe the stage of the pathology, the brighter the symptoms. Often, at a later stage, individual symptoms are added that provoke irreversible changes in orgasm, such as:
- shortness of breath at rest;
- heartache;
- when you inhale, the veins in the neck swell;
- tachycardia due to low blood pressure;
- swelling that does not go away even after taking special medications;
- pain in the liver area, etc.
Diagnostics
Diagnosis of this condition begins with examining the patient and asking about his well-being and complaints. For a more detailed assessment, an instrumental examination is carried out:
- X-ray of the lungs, which reveals both diseases of the respiratory system and changes in heart size;
- Breast CT is performed if necessary if the diagnosis remains doubtful after radiography;
- Ultrasound of the heart allows you to determine the degree of dysfunction of this organ;
- catheterization and invasive manometry accurately determines pressure in the pulmonary artery and heart cavities;
- The ECG reflects secondary changes in advanced cases.
First aid for pulmonary edema
Acute cardiopulmonary failure, which must be treated immediately, is dangerous. During an attack, the patient needs help because he cannot help himself. Therefore, emergency care should be based on the following manipulations:
- Call an ambulance.
- Place the person on a chair in the “horse” position with the elbows resting on the back.
- Place a Nitroglycerin tablet under your tongue.
- Open all windows to provide fresh air.
- If you have an oxygen mask, apply it to the patient.
- Make tight bandages on both legs to slightly relieve the load on the heart and the amount of fluid circulating through it. Make sure that decompression of the lower extremities does not occur.
If the patient gets worse, cardiopulmonary resuscitation methods should be used. To do this, it is advisable to adhere to the recommendations of the American Cardiology Association:
- If you do not have the skills for such actions, then perform only manual massage of the sternum, continuously pressing on the chest at least 2 presses per second until the doctors arrive.
- There is no need to perform mouth-to-mouth artificial respiration.
- If you have resuscitation skills, choose one of the options:
- alternately do 30 presses and 2 mouth-to-mouth exits, alternating them;
- press rhythmically on the chest.
Important! This resuscitation is only suitable for adult patients; for children, the measures are different.
Objectives of any resuscitation measures:
- clear and open the victim’s airways;
- do everything to restore the body’s respiratory function;
- normalize blood circulation.
For children over one year old, you need to carry out five cycles of pressure and mouth-to-mouth breaths in a couple of minutes. Compression of the sternum is carried out with one hand, and breaths should be weaker. If this does not bring results, you need to use a defibrillator in strict compliance with the instructions in the instructions for it.
Diagnosis
It is important to find the root cause that provoked cardiopulmonary failure. The most valuable laboratory tests are:
- checking blood for gas composition;
- chest x-ray;
- angiopulmonography;
- ventilation-perfusion lung scintigraphy;
- FVD study;
- ECG;
- EchoCG;
- transbronchial and/or transthoracic lung biopsy.
General clinical samples will be taken from the patient to determine the current state of health and confirm preliminary conclusions.
WE RECOMMEND: Treatment of rheumatic myocarditis in children
Diagnosis of the disease
The gold standard for research in case of insufficiency of heart and lung function is an ultrasound examination of the heart (EchoCG). Ultrasound reveals enlargement of the right chambers of the heart and a decrease in cardiac output. In addition, to confirm the diagnosis, an ECG, chest x-ray, bronchial and pulmonary function testing (BPF) and pulse oximetry are performed.
Treatment methods
The doctor will decide what kind of care and therapy should be based on the form of the pathology and the current condition of the patient. The acute form of the pathology is treated in intensive care. Therapy of acute cardiopulmonary failure is based on:
- the use of thrombolysis drugs, which are indispensable for thrombosis of the arteries of the pulmonary trunk;
- administration of a dose of Papaverine, which relaxes the walls of the vascular bed, which leads to improved blood flow in general;
- a course of anticoagulants, which remove blood stagnation by thinning it;
- an injection of Atropine, which makes breathing easier by relaxing the pulmonary muscles.
For the treatment of chronic forms of pathology, complex treatment methods are used, which are based on:
- eliminating the root cause of cardiopulmonary failure;
- use of anti-inflammatory drugs;
- drugs that make the blood in the body more fluid;
- means for relaxing muscles, which leads to dilation of the bronchi;
- hormonal therapy of various origins.
Pathogenesis
A decrease in the pumping function of the heart in CHF leads to secondary activation of the sympathoadrenal (SNS) and renin-angiotensin-aldosterone systems (RAAS) on the one hand and vasopressin (known as the antidiuretic hormone ADH) and atrial peptides on the other hand. The process mediates peripheral and renal vasoconstriction, causing a decrease in glomerular filtration rate, which, coupled with the already reduced blood filling pressure, leads to secondary activation of the RAAS. Activation of the RAAS results in an increase in aldosterone secretion, thereby ensuring proper perfusion pressure in the tissues due to increased reabsorption of sodium and water by the proximal nephron tubules.
Stimulation of the release of vasopressin from the posterior lobe of the pituitary gland occurs in response to the activation of baroreceptors that respond to a decrease in blood filling pressure. Increased ADH levels lead to myocardial fibrosis, hypertrophy and vasoconstriction, as well as increased water reabsorption in the nephron collecting ducts, despite the already existing overload of the heart with circulating blood volume in the form of stretched atrial tissue and low plasma osmolality.
Pathogenetically, water-electrolyte homeostasis is mainly under the control of renal regulation, which is the most vulnerable point of sodium-potassium homeostasis. The clinical effects of ADH release are thirst and increased water intake. Angiotensin II also contributes by stimulating the brain's "thirst center" and promoting the release of ADH. Under physiological conditions, hyperactivation of neurotransmitter systems is excluded by the multidirectionality of their action, and with CHF, conditions arise for the occurrence of edema, against the background of hypotension and hypoosmolality. It is true that it is worth noting that, according to experimental data, different mechanisms were noted underlying the activation of the RAAS and SNS on the one hand and the vasopressin and atrial peptide systems on the other hand
A transient decrease in renal function and direct renal damage inevitably contribute to an increase in potassium levels, which is leveled for the time being by taking loop and/or thiazide diuretics. However, it is worth noting that it would be preferable to choose the drug Torasemide, which, compared to Furosemide, promotes less activation of the RAAS and mediates less excretion of potassium from the body.
Acute heart failure
Acute heart failure (AHF), which is a consequence of impaired myocardial contractility and a decrease in systolic and minute blood volumes, is manifested by extremely severe clinical syndromes: cardiogenic shock, pulmonary edema, acute renal failure.
Acute heart failure is most often left ventricular and can manifest as cardiac asthma, cardiogenic pulmonary edema, or cardiogenic shock.
Complications and prognosis
No cardiologist will give a 100% prognosis about the further development of pathology and the consequences that cardiopulmonary failure can provoke. In each individual case, this will be individual and depend on how severe the disease is, whether there are concomitant pathologies, how old the patient is, how his body reacts to therapy, what kind of lifestyle he leads, and much more. Often with such a pathological process one should not count on a favorable prognosis.
Interesting! In a number of European countries and the United States, the leading position in hospitalization of older people is occupied by cardiopulmonary failure.
Those who have suffered a stroke or heart attack with cardiopulmonary failure syndrome have a negligible chance of survival. Any pathological changes in the functioning of the lungs and heart are always difficult, difficult to treat and have an unfavorable prognosis with frequent deaths. Therefore, those who suffer from angina pectoris, ischemic heart disease and hypertension should not trigger the pathology, so as not to provoke an attack of cardiopulmonary failure.
Prevention
Prevention of the primary type of cardiopulmonary failure includes timely recognition of pathology and accelerated treatment of the root cause of their occurrence. It is important to remove all provoking factors from life, such as:
- smoking;
- unhealthy and sedentary lifestyle;
- unbalanced diet;
- bad habits.
You should always monitor your health, and not only when the problem becomes acute. A person's harmonious weight puts little strain on the heart without wearing it out. The risk of thrombosis is reduced, and this all depends on nutrition and physical activity. The more it is, the stronger the body. But without fanaticism, excess training and excessive effort can lead to no less sad consequences than their absence.
If there is a hint of cardiac or pulmonary pathology, do not delay a visit to the doctor. If there are diagnosed pathologies in these systems, you need to regularly undergo all the necessary examinations and tests in order to monitor the trend of the disease and the effectiveness of the chosen therapy.