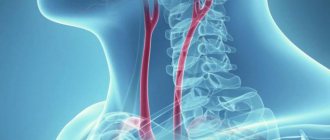
Structure of the pulmonary artery
The location of the pulmonary artery is the central part of the chest. This blood vessel consists of two large branches and several small ones, branching into a capillary network. The average diameter of large branches is 25 mm.
The PA is connected to the right ventricle. Branching from it, the artery is located next to other large vessels. Dividing, the branches of the pulmonary artery enter the lungs, one into the right, the other into the left. At the base of the PA there is a valve that ensures timely blood flow from the right ventricle.
Location of aircraft branches:
- The left branch is a continuation of the pulmonary trunk. It is located in front of the aorta and the descending part of the left bronchus.
- The right branch is longer than the left one. On one side of the vessel is the superior vena cava and the ascending aorta. On the other is the main right bronchus.
Classification
Clinically, PE is classified into the following types:
- massive - more than 50% of the volume of the vascular bed of the lungs is affected (embolism of the pulmonary trunk and/or main pulmonary arteries) and the disease manifests itself in shock and/or systemic hypotension;
- submassive - 30 - 50% of the volume of the vascular bed of the lungs is affected (embolism of several lobar or many segmental pulmonary arteries) and is manifested by symptoms of right ventricular failure;
- non-massive - less than 30% of the volume of the vascular bed of the lungs is affected (embolism of small distal pulmonary arteries), manifestations are absent or minimal (pulmonary infarction).
Functions of the pulmonary artery
The pulmonary artery of the heart is one of the most important vessels in the body. It is irreplaceable, and its failure is unacceptable. Aircraft functions:
- The main function is to supply venous blood to the lungs. At first glance, this sounds paradoxical. In theory, arterial blood should flow into the artery, not venous. But, thanks to this feature, the pulmonary artery has another important function.
- Enriches the blood entering it from the right side of the heart with oxygen. The effect is achieved due to gas exchange in the capillaries that entwine the alveoli - small respiratory “bubbles”. The blood, enriched with oxygen, is again sent into the systemic circulation and supplies oxygen to all tissues and organs.
Notes
- Geerts WH, Code KI, Jay RM, Chen E, Szalai JP (December 1994). "A prospective study of venous thromboembolism after major trauma." N.Engl. J. Med. 331
(24):1601–6. DOI:10.1056/NEJM199412153312401. PMID 7969340. Retrieved 2011-09-19. - A.I.Kirienko, A.A.Matyushenko, V.V.Andriyashkin, D.A.Churikov.
Thromboembolism of the pulmonary arteries: diagnosis, treatment and prevention (Russian) (14-06-2006). Archived March 19, 2012. - White RH (June 2003). "The epidemiology of venous thromboembolism". Circulation 107
(23 Suppl 1):I4–8. DOI:10.1161/01.CIR.0000078468.11849.66. PMID 12814979. Retrieved 2011-09-19. - Horlander KT, Mannino DM, Leeper KV (July 2003). "Pulmonary embolism mortality in the United States, 1979-1998: an analysis using multiple-cause mortality data." Arch. Intern. Med. 163
(14):1711–7. DOI:10.1001/archinte.163.14.1711. PMID 12885687. Retrieved 2011-09-19. - Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ (March 1998). "Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study." Arch. Intern. Med. 158
(6):585–93. PMID 9521222. Retrieved 2011-09-19. - ↑ 1 2 3 4
Torbicki A, Perrier A, Konstantinides S,
et al.
(September 2008).
"Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)". Eur. Heart J 29
(18):2276–315. DOI:10.1093/eurheartj/ehn310. PMID 18757870. Retrieved 2011-09-15. - Wells PS, Anderson DR, Rodger M, Stiell I, Dreyer JF, Barnes D, Forgie M, Kovacs G, Ward J, Kovacs MJ (2001). "Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer." Ann Intern Med 135
(2):98–107. PMID 11453709. - Le Gal G, Righini M, Roy PM, et al.
(February 2006).
“Prediction of pulmonary embolism in the emergency department: the revised Geneva score.” Annals of Internal Medicine 144
(3):165–71. PMID 16461960. - ↑ 1 2 3 A. Kartasheva.
Pulmonary embolism. New ESC recommendations (2008) // Medicine Review. - T. 4, issue. 04. - pp. 56-64. - Schrecengost JE, LeGallo RD, Boyd JC, et al.
(September 2003).
"Comparison of diagnostic accuracies in outpatients and hospitalized patients of D-dimer testing for the evaluation of suspected pulmonary embolism." Clin. Chem. 49
(9):1483–90. DOI:10.1373/49.9.1483. PMID 12928229. - ↑ 1 2 V.S.
Savelyev, E.I. Chazov, E.I. Gusev et al. Russian clinical guidelines for the diagnosis, treatment and prevention of venous thromboembolic complications (Russian). - Moscow: Media Sphere, 2010. - T. 4, issue. 2. - pp. 1-37. - ISSN 1997-697. - Rodger M, Makropoulos D, Turek M, et al.
(October 2000).
"Diagnostic value of the electrocardiogram in suspected pulmonary embolism." Am. J. Cardiol. 86
(7):807–9, A10. DOI:10.1016/S0002-9149(00)01090-0. PMID 11018210. - Scott RC (July 1971). "The S1Q3 (McGinn-White) pattern in acute cor pulmonale: a form of transient left posterior hemiblock?". Am. Heart J 82
(1):135–7. PMID 5581712. - McGinn S, White P D (1935). "Acute cor pulmonale resulting from pulmonary embolism." J Am Med Assoc 104
:1473–80. - A. V. Strutynsky.
Electrocardiogram. Analysis and interpretation. - M: MEDpress-inform, 2009. - P. 120-123. — 224 p. — 10,000 copies. — ISBN 5-98322-542-1. - Come PC (April 1992). "Echocardiographic evaluation of pulmonary embolism and its response to therapeutic interventions." Chest 101
(4 Suppl):151S–162S. PMID 1555480. - Schaefer-Prokop C, Prokop M (November 2005). "MDCT for the diagnosis of acute pulmonary embolism." Eur Radiol 15 Suppl 4
:D37–41. PMID 16479644. Retrieved 2011-09-17. - Raschke RA, Gollihare B, Peirce JC (1996). "The effectiveness of implementing the weight-based heparin nomogram as a practice guideline." Arch. Intern. Med. 156
(15):1645–9. PMID 8694662. Retrieved 2011-09-18. - Erkens P. M., Prins M. H. (2010). "Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism." Cochrane Database Syst Rev
(9): CD001100. DOI:10.1002/14651858.CD001100.pub3. PMID 20824828. Retrieved 2011-09-18. - ↑ 1 2 Paul L. Marino.
Intensive therapy. - Moscow: GEOTAR-Media, 2010. - 770 p. — ISBN 978-5-9704-1399-9. - Dong BR, Hao Q, Yue J, Wu T, Liu GJ (2009). "Thrombolytic therapy for pulmonary embolism." Cochrane Database Syst Rev
(3): CD004437. DOI:10.1002/14651858.CD004437.pub3. PMID 19588357. Retrieved 2011-09-18. - Decousus H, Leizorovicz A, Parent F, et al.
(February 1998).
“A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group.” N.Engl. J. Med. 338
(7):409–15. DOI:10.1056/NEJM199802123380701. PMID 9459643. Retrieved 2011-09-18.
Types of diseases
Disturbances in the functioning of the pulmonary circulation are caused by pathologies associated with the pulmonary artery. All LA diseases are extremely dangerous for humans and require immediate treatment.
Thromboembolism
PA thromboembolism is a dangerous disease associated with blockage of a vessel. The thrombus blocks the base of the pulmonary artery or one of its branches. The cause of thromboembolism is poor blood thinning and the formation of blood clots. Symptoms increase rapidly, the person is in serious condition and needs emergency help.
With thromboembolism, the work of:
- brain;
- respiratory system;
- of cardio-vascular system.
Doctors do not divide thromboembolism into stages, since the symptoms develop very quickly and the patient’s condition worsens. Even death is possible. But sometimes doctors still divide pathology into two conditions:
- Initial. The condition is deteriorating sharply. Problems with the respiratory system appear. Choking develops.
- Progressive. The man is in critical condition. Delay in receiving medical help can result in severe complications and death.
PA stenosis
With stenosis, the lumen of the artery narrows at the point where it branches from the right ventricle of the heart. Due to the narrowing of the vessel in the valve area, a pressure difference occurs in the PA and in the right ventricle.
Stenosis causes the following pathologies:
- the interatrial septum is affected;
- increased blood pressure in the right atrium;
- hypertrophy and failure of the right ventricle.
Stages of stenosis:
- Initial. The lumen is narrowed slightly, but the passage of blood through the PA is impaired. There are minor symptoms in the lungs and heart.
- Progressive. The lumen is noticeably narrowed. Symptoms are more pronounced than in the initial stage. Tachycardia, shortness of breath and heart pain are observed.
- Launched. Dangerous condition. The lumen is completely narrowed. The functioning of almost all organs is disrupted.
For stenosis, only one treatment option is possible - surgery to eliminate the narrowing.
Valve insufficiency
When the pulmonary valve is insufficient, the patient first experiences increased heart rate, shortness of breath, weakness and cyanosis. Sharp pains appear in the heart, the person is drawn to sleep. In the advanced stage, cardiac cirrhosis of the liver may appear.
The most dangerous complications of valve insufficiency:
- pulmonary artery aneurysm;
- pulmonary embolism.
Treatment of pulmonary valve insufficiency:
- Drug therapy. With the help of drugs, heart failure is eliminated and bacterial endocarditis is prevented.
- Surgery. The patient undergoes valve replacement.
In the postoperative period, there is a risk of developing degeneration of bioprostheses and secondary infective endocarditis.
On a note! In pulmonary embolism, a detached blood clot, moving through the vessels, blocks the lumen of the pulmonary artery. This condition can cause infarction of the lung tissue and disruption of the functioning of internal organs.
Possible complications
In the absence of timely and comprehensive treatment, the patient will certainly develop complications. In a healthy person, when the pulmonary artery is damaged, respiratory and heart failure, cirrhosis of the liver develop, and fluid accumulates in the abdominal cavity.
In patients who suffer from other diseases of the heart or blood vessels, their symptoms are aggravated, a critical deterioration in their condition, an artery aneurysm, or complete closure of its lumen is possible. Right ventricular hypertrophy often develops, which interferes with the movement of blood through the chambers of the heart.
The most severe and dangerous complication is considered to be death. Most often it is provoked by thromboembolism, since there is very little time to provide assistance.
The pulmonary artery is one of the most important vessels in the human body, located in the chest cavity and exits directly from the heart chamber. If signs of an artery disorder appear, you should immediately consult a doctor.
Symptoms
With any disease that affects the LA, almost the same symptoms occur. This makes it difficult to make a quick diagnosis. Symptoms are similar to many other conditions.
Primary symptoms:
- pale bluish skin;
- the skin becomes cold to the touch.
The progression of the disease causes:
- increased sweating;
- the skin becomes sticky and damp;
- mucous membranes turn pale;
- In some patients, the skin turns red - this indicates high blood pressure.
In addition to external signs, the following symptoms may be added:
- Shortness of breath even at rest or with minimal exertion. Patients may lack air and develop a fear of death. Patients with angina pectoris may confuse pulmonary disease with another attack.
- Headaches and dizziness. The condition worsens even with little physical activity.
- Low performance and constant feeling of weakness. Even simple actions are very difficult to perform.
- Bad dream. The symptom is aggravated in a horizontal position.
- Depressive state due to powerlessness, poor health and increasing symptoms.
- Pain in the chest. Many people confuse them with heart pathologies and take appropriate medications, which turn out to be useless if the pulmonary artery is affected.
- Heart rhythm disturbance. My heart beats faster.
- Cough. When you cough, you produce sputum containing blood.
- Swelling of the legs. As evening approaches, swelling increases.
- Enlarged veins in the cervical region. This symptom usually indicates stenosis.
Diagnostic measures
Diagnosis of pulmonary embolism is aimed at detecting a blood clot, assessing hemodynamic disturbances, and identifying the cause of the process to prevent relapses. To solve these problems, specialists carefully examine patients: collect complaints and anamnesis, study risk factors and clinical symptoms. To make a diagnosis and prescribe treatment, the results of laboratory and hardware tests are necessary. General clinical and biochemical parameters, gas composition, blood clotting factors and enzymes are determined in the blood.
A highly sensitive but nonspecific laboratory method is the detection of D-dimer, a fibrin breakdown product. If its level increases, recent thrombus formation is assumed. A normal D-dimer value helps rule out pulmonary artery thrombosis in patients.
Instrumental research methods play a more important diagnostic role. These include:
- Electrocardiography - detection of sinus tachycardia with a high P wave, deviation of the electrical axis to the right, increased amplitude of the R and S waves, displacement of the ST segment, negative T wave.
- X-ray examination of the lungs - with embolism, the pulmonary arteries are dilated, the number of contrasted peripheral branches is reduced, and the pulmonary pattern is deformed.
X-ray signs of pulmonary embolism (Fig.: NSC “Institute of Cardiology N.D. Strazhesko”) - Pulmonary angiography is a radiopaque examination of the pulmonary artery, which allows one to detect blood clots and damage in it.
- Perfusion scanning of the lungs is a highly informative method that determines perfusion defects, their area, and the degree of reduction in radioactivity. A decrease in the accumulation or complete absence of an isotope preparation in the lung area indicates a circulatory disorder in this area.
- SCT is a standard non-invasive technique that allows you to visualize the pulmonary artery, assess its condition, and detect blood clots in it. This procedure is easy to perform, highly sensitive and specific.
- Echocardiography - detection of blood clots in the cavities of the heart, identification of signs of pulmonary hypertension, exclusion of heart defects and myocardial pathology. The right chambers of the heart are dilated, the interventricular septum bulges to the left and makes paradoxical movements during the relaxation phase.
- Angiography of pulmonary vessels is an invasive diagnostic method that reveals a filling defect in the lumen of the artery or complete obstruction with “amputation” of the vessel and breakage of its contrast. In this case, the branches of the pulmonary artery are sharply narrowed. Slow removal of the contrast agent is observed.
Diagnosis of pulmonary embolism is a complex process. Nonspecific symptoms of the pathology often mislead doctors. Standard methods of examining a patient can only exclude other diseases: inflammation and pulmonary edema, acute coronary insufficiency. An untimely or incorrect diagnosis is the cause of death of the patient.
Causes of the disease
Due to the proximity of the pulmonary artery to the heart, its pathologies are often associated with its work. There are general reasons and those related to a specific pulmonary artery disease. Thromboembolism is associated with the formation of blood clots, stenosis is associated with narrowing of the artery, and valve insufficiency is associated with congenital defects.
Causes of development of pulmonary diseases:
- Not drinking enough fluid.
- Diseases that cause an increase in the number of platelets.
- Metabolic disease.
- Lack of vitamins and minerals, on which vascular health depends.
- High blood pressure. A severe stage of hypertension, which is difficult to control with medications.
- Prolonged lack of oxygen in the body.
- Respiratory diseases and operations on them.
PA diseases can also be provoked by myocardial infarction, heart disease, heart failure, as well as various lesions of the heart and blood vessels, including changes associated with the aging of the body.
On a note! Platelets are blood platelets on which blood clotting depends. A deficiency of platelets leads to prolonged bleeding, an excess leads to thrombosis.
Epidemiology
PE is a relatively common cardiovascular pathology (approximately 1 case per thousand population per year)[1]. In the United States, PE affects approximately 650,000 people and results in 350,000 deaths per year[2]. PE occurs more often in the elderly (In the United States, venous thromboembolism occurs for the first time in about 100 out of 100,000 people per year and increases exponentially from less than 5 cases per 100,000 people in children under 15 years of age to 500 cases per 100,000 people at age 80 years) [3]. Data on the association of gender with PE vary, but an analysis of a US national database found that men have a 20% to 30% higher mortality rate than women.[4] The incidence of venous thromboembolism among the elderly is higher in men, but in patients under 55 years of age it is higher in women[5].
Diagnostics
The health and even life of the patient depends on how quickly the correct diagnosis is made. For diagnosis, several methods are consistently used to help determine the cause of the pathological condition.
Diagnostic stage and methods:
- Inspection. The doctor puts forward one or more hypotheses regarding the causes of pathological symptoms. Establishes the severity of the disease.
- General and biochemical blood test. Venous blood studies reveal abnormalities and allow one to assess the condition of various organs and systems.
- Electrocardiogram. The work of the heart is assessed and pathologies are identified. The method does not allow you to notice minor problems.
- Ultrasound. Unlike an ECG, it can detect the slightest problems in the functioning of the heart.
- X-ray. Thanks to chest x-ray, it is possible to identify pathologies in the heart and lungs.
- MRI. The most informative way to detect pathologies. Allows you to quickly locate the problem.
Content
- 1 Epidemiology
- 2 Causes and risk factors
- 3 Pathogenesis
- 4 Classification
- 5 Clinical picture
- 6 Diagnostics 6.1 Laboratory diagnostic methods 6.1.1 Determination of d-dimer levels
- 6.2.1 Electrocardiography
- 7.1 Correction of hemodynamics and hypoxia
Treatment methods
The proximity of the aircraft to the heart forces doctors to show maximum efficiency in the event of any pathologies in its work. Treatment begins immediately after identifying problems in the functioning of this vessel.
Medications
Drug therapy depends on the severity and nature of the disease. But there are general treatment tactics used for various LA diseases.
Patients are prescribed medications:
- normalizing blood clotting;
- for persistent hypertension - diuretics;
- cardiac glycosides;
- mild sedatives - for nervous excitement;
- vasodilators - to prevent protrusion;
- for high blood pressure - short-acting diuretics.
The list of drugs may also include corticosteroids and bronchodilators.
Traditional methods
Doctors do not consider traditional methods effective and do not recommend their use. Some of them can even cause complications. If the course of the pathology is not acute, patients are allowed to drink infusions for headaches and panic.
Mint infusion is recommended not only for pulmonary diseases, but also for hypertension. Mint calms, normalizes heartbeat, and slightly lowers blood pressure.
Preparation of mint infusion:
- pour 6 g of freshly picked leaves into 0.6 liters of boiling water;
- leave for 20 minutes;
- strain and drink 0.1 liter 3 times a day for a week.
Motherwort is considered another effective remedy. You can buy a pharmacy tincture or make it yourself.
Preparation of motherwort infusion:
- 40 g of rhizomes pour 0.2 liters of alcohol;
- leave for 14 days;
- strain and drink 2 times a day, 30 drops.
Motherwort tincture should be taken with water. The recommended course is a week.
Folk remedies, like medications, should be used only after consultation with a doctor. Contraindications to their use are acute conditions with stenosis, thromboembolism and valve insufficiency.
Other methods
Surgical interventions are the best way to treat LA diseases. It is rarely possible to get by with medications alone.
Possible operations:
- In patients with thromboembolism, a clot that is blocking blood flow is removed.
- For patients with stenosis, the vessel is dilated by introducing a special device into it. If, with PA stenosis, the pressure gradient rises above 50 mmHg. Art., the question of the expediency of the operation is not even raised; it is carried out without delay.
- Patients with valve insufficiency have a prosthesis implanted.
Oxygen therapy is also recommended for pulmonary diseases. This procedure is carried out in a clinic or in a hospital. Its duration is 20-30 minutes. Patients are prescribed daily treatments. The course of treatment is 2 weeks.
Mechanism of development of cor pulmonale
In order to understand how pathology occurs in people, it is necessary to have a general understanding of how the process of gas exchange and blood circulation occurs in the human body.
These two processes are inevitably interconnected, since saturation of the blood with oxygen is possible only through the breathing process, and the breathing process itself depends on the saturation of the lungs with blood.
Naturally, these physiological functions are provided by the anatomical structure of the human body. Therefore, if there are violations in at least one system, the second inevitably suffers.
The blood is saturated with oxygen in the following way: venous blood is transferred to the right side of the heart, from where it is pushed by the heart muscles into the pulmonary artery. It is when the blood enters the lungs that it takes in the oxygen that was absorbed from the outside, and then the arterial blood enters the left side of the heart, subsequently spreading throughout the body.
Venous blood contains quite a lot of carbon monoxide. Its content is normal, because it is a natural element that is formed as a result of the vital activity of all the cells of our body.
The superior and inferior vena cava converge in the sinus, a small cavity located in the vestibule of the right atrium. After the blood remains in the atrium, it is transported to the right ventricle, which pushes the blood into the pulmonary artery.
It delivers blood to the lungs. Through many branched smaller vessels - arterioles and capillaries - the blood reaches the deepest parts of the lung. The main task of the blood is to move to the smallest alveoli, which take carbon monoxide from the blood and release oxygen into them.
In order for the process of direct gas exchange to take place with maximum benefit, the alveoli are intertwined with many capillaries. For proper exchange of oxygen and carbon monoxide, normal pressure is necessary, both from the circulatory system and from the alveoli.
Despite the fact that the vascular network is quite dense and the capillaries are very narrow, normally the human body is able to ensure blood flow under normal pressure even in the smallest vessel.
Some lung pathologies can cause capillary obstruction, as a result of which the pressure in this area will increase, because the blood volume does not decrease. The pulmonary artery will try to push blood into the lungs with high pressure to supply the entire organ. This is how pulmonary hypertension is formed.
Blood entering the left side of the heart transports oxygen throughout the body. The release is carried out into the aorta under significant pressure.
Pathological mechanisms occurring in the respiratory system also provoke changes in the heart. The situation can develop in two ways: in the acute form, the pressure rises rapidly, which means the right ventricle stretches quickly and to a significant volume.
The walls of the organ simply do not compress with enough force to transport blood to the pulmonary artery. In this case, some of the blood does not leave the ventricle. The new volume of blood from the atrium only further stretches the walls of the compartment.
The second option is gradual stretching of the cavity. This occurs during the chronic course of the pathology. The heart simply has time to adapt to such changes, while the muscle of the right ventricle grows due to an increase in the number of myocardiocytes. Thus, the right side of the heart increases not so much due to the expansion of the cavity, but due to the thickening of the walls of the section.
Despite the fact that the pathology manifests itself differently, the symptoms of the disease are similar in both cases.
Prevention
Prevention of pulmonary diseases includes standard measures to prevent diseases of the cardiovascular system. But there are also specific recommendations.
Prevention of aircraft diseases:
- Quitting smoking and drinking alcohol.
- Regime normalization. A normal working day, rest and normal sleep are necessary.
- The use of vitamin complexes.
- Regular visits to the doctor. Carrying out the necessary examinations.
On a note! To prevent LA diseases, it is recommended to consume products containing ascorbic acid and rutoside. Thanks to these substances, blood clots are prevented.
Treatment process
Pulmonary embolism requires hospital treatment. Patients are placed in the intensive care unit and receive full intensive care. After stabilization of the general condition, the goal of treatment is to normalize pulmonary circulation. For this, patients are prescribed strict bed rest, oxygen inhalation, and medication.
- Conservative therapy involves the use of medications that thin the blood and dissolve blood clots. Patients are prescribed thrombolytics “Urokinase”, “Streptokinase”, “Alteplase”.
- To reduce blood viscosity and maintain blood pressure at an optimal level, massive infusion therapy is performed.
- Heparin therapy is intended to prevent recurrence of pulmonary embolism. Patients are prescribed anticoagulants - Heparin, Enoxaparin, Warfarin.
- To combat hypoxia, oxygen therapy is carried out using special masks or nasal catheters; in severe cases, mechanical ventilation is indicated. Colloidal and crystalloid solutions and vasopressor agents - Adrenaline, Dopamine - are administered intravenously.
In some cases, surgery is indicated. The patient is connected to a heart-lung machine, the chest is opened, the affected artery is cut, and the blood clot is removed. Such a complex operation is difficult for patients to tolerate. With frequent recurrences of pulmonary embolism, surgeons place a special filter in the branches of the pulmonary artery and the inferior vena cava.
When occlusion of the pulmonary artery is caused not by blood clots, but by other emboli, the pathology is treated based on the reasons for its development:
- Foreign bodies are removed surgically.
- Drops of fat do not require any intervention, since they resolve on their own over time. Therapeutic measures are aimed at maintaining a satisfactory condition of the patient.
- Air bubbles are removed from the bloodstream using a catheter.
- Bacterial, parasitic and fungal emboli disappear after intensive treatment of the underlying disease.
Prevention of pulmonary embolism consists of following simple rules:
- early diagnosis and treatment of thrombophlebitis,
- prescribing anticoagulants to people at risk,
- maintaining a healthy lifestyle,
- proper nutrition and maintaining weight within normal limits,
- timely treatment of infectious diseases,
- frequent changes of body position and periodic warm-ups,
- wearing compression stockings,
- drink plenty of fluids without coffee or alcohol,
- fight against smoking.
The prognosis of the pathology is ambiguous. It depends on the form of the disease and the speed of medical care. Timely and adequate treatment of patients makes the prognosis for recovery favorable. In the presence of persistent cardiovascular and respiratory dysfunction, the risk of death increases significantly.
Pulmonary embolism is currently a pressing medical problem. This is due to the onset of almost lightning-fast death of the patient. Blockage of the pulmonary artery is a dangerous condition and one of the most common causes of death. If your breathing becomes shallow, chest pain and a feeling of fear appear, you should immediately go to the hospital.