Hip dysplasia (from the ancient Greek δυσ - “disturbance” and πλάθω - “form”) is a pathology caused by a violation of the formation of the elements of the joint itself and its auxiliary apparatus in the prenatal period.
Stages of joint dysplasia
The hip joint is the largest and most loaded moving joint in the body. Its articular surfaces are made of the acetabulum of the pelvic bone and the head of the femur, the fixation of which (preventing upward displacement) is ensured by the acetabulum lip (another name is “limbus”), a cartilaginous element that limits the cavity.
Anatomically and physiologically, the joint capsule and ligamentous apparatus provide the complete mutual arrangement of the articulating surfaces. The correct structure of the auxiliary structures protects the joint from subluxations and dislocations (displacement of the articular surfaces relative to each other) under conditions of increased load.
During the newborn period, the hip joint, even in healthy children, is a rather biomechanically unstable structure, which is due to a number of age-related characteristics:
- flattened, shallow acetabulum;
- larger size of the femoral head in relation to the size of the socket;
- poorly developed muscle frame in the gluteal region;
- insufficient compaction of the joint capsule.
Additional development of the joint occurs during the first year of life, almost completed by the age when the child begins to move independently.
With dysplasia of the anatomical structures that form the joint and its auxiliary apparatus, there is a high probability of improper development of the hip joint in the first months of life; as a result, the risk of injury increases, and difficult-to-correct defects in gait and posture and subsequent disability may appear.
The incidence of pathology in different countries is from 2 to 10%. Girls are more susceptible to the disease (8 out of 10 cases), the left hip joint is involved in the process most often - more than half of all identified dysplasias, pathologies of the right joint and combined (with damage to both joints) occur equally, in approximately 20% of patients. If a breech fetus is diagnosed, the risk of dysplasia increases 10 times.
General information about hip dysplasia
Hip dysplasia in infants is a pathology that occurs during prenatal development. It is characterized by a violation of the structural development of the articulation: the location of the acetabulum does not correspond to the placement of the femoral head, the axis of the limb is disrupted, and it becomes too mobile. The head of the bone does not ossify as it should. The joint configuration becomes incorrect, so the limb cannot perform its functions.
Hip dysplasia is found predominantly in girls. Moreover, the left side of the body is predominantly affected. Bilateral disease occurs in 20% of all cases. It is not difficult to identify such a disorder in a one-year-old baby, since during this period he learns to crawl and walk. He develops lameness or a “duck gait” and a curvature of the spine.
Hip dysplasia in adults often occurs as a result of traumatic injury. Sometimes it is a continuation of childhood pathology if proper therapy has not been carried out. Eliminating the disease in adult patients is long and difficult. Conservative methods rarely give positive results. In most cases, joint replacement surgery is required.
Causes
The causes of hip dysplasia in children are not fully understood.
What is certain is that dysplasia is more common in girls. Everything is explained by the fact that during pregnancy a woman begins to produce a hormone, the main task of which is to make the joints and muscles soft and elastic so that the woman can give birth. This hormone affects not only the joints and muscle tissue of the expectant mother, but also the baby, especially the joints of a female child.
The second factor that predisposes to the development of hip dysplasia in children is the first birth. It has been proven that during the first pregnancy, more of this hormone is produced than during each subsequent one.
Babies with breech presentation are more at risk. It has been noted that left-sided dysplasia is more common. This occurs due to the physiological characteristics of the position of the child in the womb. The left leg is bent more.
The larger the fetus, the higher the risk that the child will have hip dysplasia after birth. Genetic predisposition, parental age and other factors also play a role in the development of dysplasia.
There are many reasons for the occurrence of hip dysplasia. The main ones are hereditary predisposition, breech presentation of the fetus during pregnancy, pathology of the 1st trimester of pregnancy, oligohydramnios and many others.
Sometimes, a congenitally normal hip joint may lag behind in further development and not correspond to age - then this dysplasia is no longer congenital, but “acquired”.
There are several theories for the occurrence of hip dysplasia, but the most substantiated are genetic (25-30% have female inheritance) and hormonal (the effect of sex hormones on the ligaments before childbirth).
The hormonal theory is confirmed by the fact that dysplasia is much more common in girls than in boys. During pregnancy, progesterone prepares the birth canal for childbirth by softening the ligaments and cartilage of the woman's pelvis.
Once in the fetal blood, this hormone finds the same application points in girls, causing relaxation of the ligaments that stabilize the hip joint. In most cases, if the process is not interfered with by tight swaddling, restoration of the ligament structure occurs within 2-3 weeks after birth.
It has also been noted that the occurrence of dysplasia is facilitated by limited mobility of the hip joints of the fetus during intrauterine development. In this connection, left-sided dysplasia is more common, since it is the left joint that is usually pressed against the wall of the uterus.
In the last months of pregnancy, the mobility of the hip joint can be significantly limited with the threat of miscarriage, more often in first-time mothers, in the case of breech presentation, oligohydramnios and a large fetus.
Today, the following risk factors for hip dysplasia are identified:
- presence of hip dysplasia in parents,
- abnormalities of the uterus,
- unfavorable course of pregnancy (threat of miscarriage, infectious diseases, taking medications),
- breech presentation of the fetus,
- transverse position of the fetus,
- multiple pregnancy,
- oligohydramnios,
- natural birth with breech presentation of the fetus,
- pathological course of childbirth,
- first birth,
- female,
- large fruit.
The presence of these risk factors should be a reason for observation by an orthopedist and preventive measures (wide swaddling, massage and gymnastics).
Reasons for development
Hip dysplasia develops under the influence of internal and external negative factors. The following causes of the disease are identified:
- foot deformities;
- disturbances in the process of gestation: the influence of unfavorable environmental conditions, chemicals, medications;
- spinal cord pathologies;
- mother's age (over 35 years);
- hereditary predisposition (the risk of dysplasia increases to 30%);
- excessively high levels of oxytocin during pregnancy;
- heavy fetal weight or difficult labor;
- prematurity;
- breech presentation of the fetus - there is a high risk of mechanical damage to the joint;
- problems with the development of the spinal column.
Incorrect swaddling of the baby can also provoke the development of the disease. The legs should not only have free space for movement, but the mother will also have to perform special exercises to bring the limbs together and spread them apart.
Find out what the causes of pelvic displacement are and how to treat it in this article.
How is diagnosis carried out?
A newborn child is examined by a neonatologist in the first days of life for congenital developmental anomalies. If the doctor has discovered osteoarticular pathology, then in the discharge summary he will definitely write recommendations for parents (for example, to visit an orthopedist at the age of one month).
For a full examination of the legs, it is necessary to completely expose the child below the waist (including removing the diaper). The first thing the doctor pays attention to is the asymmetry of the inguinal and gluteal folds.
The inspection is carried out as follows. The child is placed on a flat surface, legs are straightened. Normally, the folds will be the same on both sides, and additional folds should not be observed.
However, the presence of asymmetry does not mean that the baby has an orthopedic pathology. The child needs to undergo a series of studies to exclude (or identify) the disease.
The doctor will also spread the baby’s legs bent at the knees. Normally, they will touch the surface on which the baby is located. Breeding should be uniform, easy and painless for the child.
Along with this, the hip is bent at a certain angle. If a characteristic click is heard (this is pathological in many cases), then it can be regarded as the entry of the joint into the acetabulum.
Ultrasound examination of the pelvic bones
Parents should also monitor their baby's feet regularly. There are certain symptoms of hip dysplasia in infants.
Here are some recommendations on how to identify pathology at home (the baby should lie on his back, on a flat surface):
- Align both legs. Look at the level of the heels and make sure that both limbs are the same in length.
- Bend your knees and place your feet on the surface. Check your knees - in a healthy child their level will be the same.
- Regularly perform hip joint exercises (flexion and extension). If you hear clicks and strange sounds (especially on one side), then you need to contact a specialist.
To accurately determine the pathology, it is necessary to undergo an instrumental examination.
The orthopedist will offer the following types of diagnostics:
- Ultrasonography. The advantage of this method is that the condition of soft tissues, tendons and ligaments can be assessed extremely accurately. The diagnosis has no contraindications and is carried out quite quickly. No preparation for the study is required.
- X-ray examination (price approximately 1500-2000 rubles). This is radiation diagnostics, which consists of obtaining a negative image of the object being studied (in our case, a joint) on a light-sensitive film. Modern equipment allows you to transfer the “picture” to the monitor screen, as well as to a digital storage medium. The amount of irradiated dose is one and a half millisieverts, so this procedure is recommended to be carried out no more often than once every six months.
X-ray examination
Important! If the doctor has written out a referral for instrumental studies, then parents must undergo them. You should not refer to the fact that the child will receive “dangerous radiation.” Modern equipment “gives out” a minimum dose, which is not at all dangerous for both adults and children.
Classification of hip dysplasia
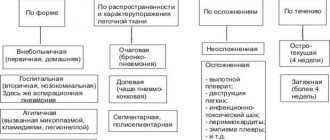
Hip dysplasia is classified depending on the violation of the anatomical structure of the joint. Pathology happens:
- Acetabular. With such damage to the hip joints in infants, problems arise with the acetabulum. It becomes flat, and the cartilaginous dome is poorly developed. The size of the acetabulum decreases. Since the pressure inside the joint increases greatly, the mobility of the limb is impaired.
- Epiphyseal. The cartilage begins to become very dense and ossify in certain places. The joint becomes stiff. The patient experiences pain that progresses over time. With this form of pathology, joint deformation often occurs. The angle between the femoral neck and its body with hip dysplasia is disrupted.
- Rotational. This pathology is characterized by a violation of the physiologically correct placement of articulation fragments. With this type of disease, children develop clubfoot, and the damaged limb becomes shortened.
There is the most severe type of pathology: transient. In this case, the shape of the head of the femur changes. There are problems with the ligaments. The head is capable of periodically extending beyond the cavity, so it must be firmly fixed.
Rehabilitation after treatment
Rehabilitation measures include mandatory minimization of pathological changes in the muscular corset of the leg. Long-term improper load makes a big contribution to the distortion of normal muscle function, so physical therapy will be required for rehabilitation. Physical exercise is the most important factor on which recovery depends.
To prevent inflammation after surgery, a course of non-steroidal anti-inflammatory drugs and adequate pain relief measures are prescribed. Usually these are local intramuscular injections or oral anesthetics. What physiotherapeutic measures are prescribed for the recovery of adults?
- electrophoresis with calcium and potassium preparations;
- swimming;
- massotherapy;
- magnetic therapy and laser therapy;
- walking.
If the disturbances have a very significant impact on the symmetry of the limbs, complete recovery will not be possible, but the extent of the disturbances will be significantly reduced. To summarize the results of treatment, an X-ray examination of the pelvic bones is performed, as a result of which it is assessed how correctly the femur was positioned in the acetabulum. Sometimes an inflammatory process occurs as a postoperative complication even while taking non-steroidal anti-inflammatory drugs. This is especially dangerous when replacing a joint. When should you seek emergency medical help?
- if the victim has a fever;
- if signs of intoxication, headache and vomiting develop;
- if the thigh and pelvis swell, redness occurs;
- if severe pain is felt when moving or at rest;
- if there is a feeling of local heat, fullness or pulsation.
In these cases, hospitalization will be carried out in a hospital to relieve the acute condition. Following the recommendations of your doctor will help prevent complications and eliminate dysplasia as much as possible.
Read also other articles about health!
Share link:
Degree of disease development
For hip disease in children, treatment depends entirely on the type and severity of the disease. For some patients, it is enough to perform special physical exercises, while others require surgical intervention and long-term wearing of orthopedic devices. The following degrees of development of the disease are distinguished:
- Initial. Here, anatomical defects are not always detected during visual inspection. The symptoms are not pronounced, so parents may not see a doctor.
- Mild (pre-luxation). In this case, a violation of the anatomy of the articulation is present, but the deviations are minor.
- Moderate (hip subluxation). At this stage of development of the pathology, gait is disrupted, and the limb becomes visually shorter.
- Severe (congenital hip dislocation in children). In this case, the anatomical defects are significant and numerous.
Despite the severity of dysplasia, this disease must be treated, as it is prone to progression. In the absence of therapy or its ineffectiveness, a person may remain disabled.
How does hip dysplasia manifest?
To understand what DTS is, it is necessary to study the description of the disease, the list of symptoms, its variations and stages. In fact, dysplasia is not a disease; it is the name given to pathological changes in the structure of the hip joint, the anatomy of which normally guarantees mobility, providing movement in all planes.
The dysplastic type of development of the hip joints is the extreme limit of normal. During it, the anatomical and histological state of the joint changes, and the functionality of the limb is disrupted. In newborns with such deviations, different stages of development of the pathological process and, accordingly, the severity of the limitation of the body’s capabilities may be observed.
A severe form is considered to be a condition characterized by a discrepancy between the sizes of the head of the femoral joint and the acetabulum, an integral part of the massive pelvic bone. When contact is lost, the hip dislocates and when the head moves completely beyond the cup-shaped socket, hip dislocation occurs.
In the absence of adequate treatment, the consequences are serious: the cavity of the empty acetabulum becomes filled with connective and loose adipose tissue over time, and as a result, it becomes difficult to correct the dislocation.
There are unilateral and bilateral dysplasia (pathology on the right and left). It has been noticed that the left joint is more often affected, this is explained by the peculiarity of the intrauterine position of the fetus, in which the child’s left leg is compressed more strongly. Right-sided processes and bilateral dysplasia are recorded less frequently.
Symptoms of hip dysplasia
In the early stages, it is not always possible to detect the disease on time. Over time, the following symptoms of congenital dislocation appear:
- a clicking or crackling sound when trying to move the limbs bent at the knees to the sides;
- pain syndrome, which becomes stronger over time (in severe forms of the pathology, sensations cannot always be eliminated with medications);
- incomplete hip abduction;
- asymmetrical placement of skin folds (this symptom is specific and, if detected, requires consultation with an orthopedist);
- change in foot rotation;
- problems with gait (the patient begins to limp or walk on his toes).
Depending on the side of the lesion, the limb appears shorter. If left untreated, muscle tissue atrophy occurs on the injured leg.
Prevention of dysplasia in children
For early detection and prevention of displacement of the femur, all newborns undergo an ultrasound of the hip joints in the maternity hospital or at 1 month.
When immaturity of the hip joint is detected, wide swaddling is used. One or two folded diapers are placed between the baby’s legs, giving the legs a position of extension and flexion.
The third diaper secures the baby's legs. It is quite possible to place a diaper on top of a disposable diaper. It is only important to ensure that the baby’s legs are not pressed against each other.
It is recommended to carry the child in a sling in a position on the side and on the stomach.
First of all, doctors recommend wide swaddling. You will need three diapers. The first diaper must be folded several times. So that you get a rectangle twenty centimeters wide. Place it between the baby's legs, spread apart.
Fold the second diaper into a scarf. Wrap the corners around the baby's hips. This way the legs are fixed at an angle of 90°. Wrap the third diaper around the baby's lower body. At the same time, with the help of a diaper, the legs are pulled up. This will prevent the baby from connecting his feet.
Gymnastics is especially good for prevention. In this case, focus on the abductor-adduction movements performed in the hip joints. Of course, this must be done carefully, without using force.
With a mild degree of dysplasia, this will be enough for the hip joint to develop as expected.
Exercises to prevent the development of the disease in children
The baby lies on his back. Starting position - the child lies on his back, abduct the legs bent at the knees to the sides, like a book, 150-200 times a day (but not at one time). It is necessary to place “free” fingers along the hips to control abduction.
There is no need to try your best to force your legs apart so that they touch the surface of the changing table. Movements shouldn't be painful! The main thing is not the force with which the legs are abducted, but the number of abductions. It is advisable to avoid strong rotational movements in the hip joints.
Baby on the tummy. Starting position - the baby lies on his stomach. You grab the baby's feet and try to bring the heels towards the buttocks. It should look something like a frog. In this case, you can lightly press your buttocks against the table. The number of times a day is about 100-150.
Stroking and rubbing. A light massage of the buttocks and thighs in the form of stroking and rubbing for 10 minutes a day can be done by the mother, but a more intense massage with kneading is best left to a professional children's massage therapist when the baby is already more than 2 months old. Naturally, an orthopedist must be seen at the ages of 1, 3 and 6 months.
Sources: spine5.com, deti.health-ua.org, orthoped.in.ua, www.mif-ua.com, doctorignatyev.com, asclepion.ru, www.medplus24.ru, 5gdp.by, www.moirebenok. ua
Diagnostic measures for dysplasia
For damage to the hip joint in children, treatment is prescribed only after a thorough examination. To begin with, the orthopedist conducts a visual examination of the child. This should be done in a warm room, in a calm environment, after the baby has eaten. Particular attention is paid to those patients who are at risk. Pathology in newborns can be diagnosed in the maternity hospital. A set of instrumental studies is also required, which includes:
- Ultrasound. The advantage of this method is complete safety for the child. It allows you to detect all defects in the structure of the joint, damage to soft tissues, ligaments. Such diagnostics are highly accurate and maximally informative.
- Radiography. It can only be used for dysplasia in adults. This technique is not used in infants, as it causes serious harm to health.
- CT or MRI. This technique is required if the patient is scheduled for surgery.
In difficult cases, adult patients are prescribed a minimally invasive examination of the joint cavity - arthroscopy.
Useful tips
If your child has been diagnosed with hip dysplasia, you should under no circumstances panic, but you should prepare for what will be difficult.
Children with splints, splints and Freika pillows may sleep worse and be more capricious, want to be held in their arms and, of course, parents have a completely natural desire to get rid of orthopedic structures as early as possible.
This is absolutely impossible to do, since the state of stabilization in children occurs quickly, but is also quickly lost, so it is necessary to adhere to the period indicated by the orthopedist-traumatologist.
You should not skip routine examinations with an orthopedic doctor, since early diagnosis of diseases in general and hip dysplasia in particular is the key to a child’s health in the future.
Do not neglect the recommendations for the use of wide swaddling for a baby. This type of swaddling does not cause any inconvenience to the child and is a guaranteed preventive measure for severe joint pathology.
Don't take lightly things like your child's limited hip mobility or unsymmetrical crotch folds.
Even if your doctor said that everything is fine, but your parent’s heart is restless, in this case it is better to consult with another specialist and conduct an additional examination than to calm down and discover an obvious problem when it will be very difficult, and sometimes impossible, to correct it.
Treatment of dysplasia
If hip dysplasia in children is diagnosed, treatment should be immediate. The sooner it starts, the greater the chance of recovery. Medicines are prescribed for any form of pathology. Therapy must be comprehensive. Its duration depends on the severity of the disease and ranges from several months to a year. Sometimes the course of treatment can be extended.
Features of conservative therapy
When diagnosing subluxation in children, treatment involves the use of conservative methods of therapy. These include:
- Free swaddling. It is carried out like this: a thick diaper is placed on the baby’s crotch, which is fixed with another cloth. In this case, the legs are constantly in a spread position. In difficult cases, the limbs can be additionally fixed with plaster. The duration of such treatment ranges from 2 months to a year. If necessary, the doctor can extend this time.
- Orthopedic devices. In this way, the joints of infants are fixed in the desired position. This requires tires, Freik pillows or Pavlik stirrups. It is recommended to wear them continuously for 1 year.
- Physiotherapeutic treatment. This method of therapy improves the innervation of cartilage tissue and blood supply to muscles. Procedures will help with mild or moderate severity of the disease. Physiotherapy is also necessary after surgery. The patient is prescribed the following procedures: ozokerite and paraffin compresses, warm baths, electrophoresis, ultraviolet heating.
- Unconventional methods. One of them is mud therapy. It has a positive effect on the joints, warms them up, and reduces the intensity of pain.
For congenital dislocation of the hip, treatment involves closed reduction of the hip bone. It is performed in children from one to 5 years of age, and then surgery is performed. Reduction is contraindicated in cases of displacement of the femoral head or severe underdevelopment of the acetabulum. The procedure requires anesthesia. After this, the patient is put in plaster for six months.
We recommend reading - How to treat trochanteritis of the hip joint?
Therapeutic exercises
Exercises for hip dysplasia in adults and children help well in the early stages of the development of pathology. The frequency of performing a complex specially selected by an orthopedist-rehabilitologist is 2-3 times a week, and its duration is 15-20 minutes. Some forms of the disease require daily repetition of exercises. It is better to exercise during the day some time after eating.
There are these types of exercises:
- Raising the lower limbs to the sides. In this case, the baby lies on his back, and the mother carefully covers her knees and spreads her legs left and right in a circular motion. It's good if the thigh touches a horizontal surface. But you can't overdo it.
- Playing “Ladushki” with your feet.
- Simulation of cycling.
Children really love the ball exercise. The baby can lie on his stomach or back. Training for adults is also selected by a rehabilitation specialist, taking into account the type and severity of the injury. For older patients, the “bicycle” exercise is perfect.
Rules for massage
Massage for dysplasia allows you to avoid atrophy of muscle fibers, improve microcirculation in the affected area, strengthen the muscle corset, and normalize its tone. The procedure is performed by a professional massage therapist. During this treatment, the specialist works on the back, neck and hip area.
The procedure can be carried out even with stirrups, without removing them. It is better to massage the baby on the changing table. The duration of the session does not exceed 10-15 minutes. Massage for hip dysplasia in children is done once a day. A total of 10-15 sessions will be required. Courses of therapy are repeated 2-3 times a year, but between them you need to rest for 1-1.5 months.
Need for surgery
Surgical treatment of subluxation in adults or children is rarely used, only in cases where conservative methods have failed. Surgery is not prescribed for babies under one year of age.
The type of operation is selected after assessing the degree of damage to the joint elements. Sometimes it is enough to simply set and fix the bones in the correct position; the patient requires a plaster cast and long-term rehabilitation. In severe cases of dysplasia, the structural elements of the joint will need to be replaced.
Treatment
Therapy for hip dysplasia is based on giving the lower limbs a forced position of full abduction in the corresponding joints, bending them to an angle of 90º while maintaining active movements.
For corrective purposes, special devices are used: preventive pants, wide swaddling, stirrups, diverting splints, pads and Freika-type pillows. The use of such means is possible only if there is no displacement of the articular surfaces relative to each other (subluxation, dislocation); otherwise, there is a worsening of the pathological condition.
Types of fixation for hip dysplasia
The period of wearing retainers for mild dysplasia is 3-4 months, although in some cases it can reach 8-10.
After removing the abductor devices, it is necessary to carry out a set of rehabilitation measures (physical therapy, massage, swimming, magnetic therapy, electrical stimulation, etc.), then (after 2-4 months) walking is allowed, in the first months - exclusively in the abductor orthopedic splint.
If therapeutic methods of correction are ineffective and in severe cases, surgical treatment is indicated.
If a breech fetus is diagnosed, the risk of dysplasia increases 10 times.
What consequences are possible?
If the pathology is not treated in early childhood, it is fraught with serious complications in adulthood. The person will simply become disabled. The consequences of hip dysplasia are:
- problems with gait;
- severe attacks of pain that cannot be relieved even with medications;
- dysplastic coxarthrosis (degenerative disease requiring surgery);
- reconstruction of the articulation;
- aseptic necrosis of the femoral head;
- amyotrophy;
- pelvic distortion.
With improper therapy, the newborn begins to have problems with the development and functionality of internal organs.
Symptoms
The symptoms of the disease are caused by a violation of the structure and, as a consequence, the functions of the articular apparatus. With this pathology, the articular capsule is overstretched, the acetabular lip is often deformed, the cavity is beveled, its depth is reduced, and the ligamentous apparatus is not able to maintain the anatomical relative position of the articular surfaces.
The main manifestations of hip dysplasia:
- shortening of the femur on the affected side, caused by the protrusion of the femoral head beyond the acetabulum;
- asymmetry of the gluteal, inguinal, popliteal skin folds of the thighs; when comparing a healthy limb and a limb with suspected dysplasia, their discrepancy in shape and number is noted (the affected side is characterized by more pronounced, deep and numerous skin folds);
- a positive symptom of slipping, or clicking (Marx-Ortolani), revealed during an objective examination by an orthopedist;
- difficulty abducting the involved hip, manifested by incomplete abduction of the limbs bent at the hip and knee joints. Normally, in children under 3 months of age, in this case the outer surface of the thigh should touch the surface on which the child is lying;
- external rotation of the affected limb.
Hip dysplasia is characterized by asymmetry of the gluteal, inguinal, and popliteal folds of the thighs.
In addition to hip dysplasia, asymmetry of skin folds and limited abduction of the lower extremities can be detected in some neurological pathologies accompanied by disturbances (dystonia, hypertonicity, hypotonicity) of muscle tone. These tests are most informative in the first 2-3 months of life; later, these methods do not demonstrate objective results.
The incidence of hip dysplasia in different countries ranges from 2 to 10%. Girls are more susceptible to the disease (8 out of 10 cases).
After reaching 1 year of age, the following signs may indicate pathology:
- a characteristic gait disturbance with a fall on the sprained leg and deviation of the body to the affected side (Duchenne symptom with unilateral dislocation);
- pelvic tilt towards the affected side;
- characteristic “duck” gait with bilateral lesions;
- Trendelenburg's symptom, determined when standing on the limb with the affected joint and manifested by drooping of the gluteal fold on the opposite side.
Prevention
With proper treatment for hip dysplasia, there is a chance of achieving a full recovery. However, it is better to prevent such a problem from occurring at all. The following preventive measures should be observed:
- Swaddle your baby freely.
- It is correct to hold a child in your arms. His legs should not be pressed too tightly towards you. This rule must also be followed when feeding the baby.
- Periodically undergo preventive examinations by an orthopedist.
- When transporting a child in a car, he must be in a special seat.
- Try to follow all the doctor’s advice while carrying a child. This especially applies to those expectant mothers who are at risk.
Hip dysplasia is a serious disorder of its structure, for which therapy should be carried out immediately after pathological changes are detected. Only proper treatment will achieve a favorable result.
Share the article on social media. networks:
Types of dysplasia
Dysplasias are very diverse and heterogeneous, congenital and acquired dysplasias are essentially very different processes, some involve several systems, others only areas of the mucous membrane.
Congenital dysplasias are manifested by developmental anomalies - deviations in the structure that do not interfere with normal functioning, and developmental defects - these anomalies already disrupt the functioning of the anatomical region.
Mucosal dysplasia does not form defects or developmental anomalies, but can lead to malignant processes. Absolutely different manifestations of dysplasia do not allow creating a unified classification; each researcher of the problem offers his own systematization of heterogeneous pathology, not free from shortcomings.
Congenital dysplasias are formed in the prenatal period; clinical manifestations affect the integumentary tissues and the musculoskeletal system; their division is very conditional.
Dysplasia of the ectoderm is distinguished - the superficial tissue of the embryo from which the outer integument is formed: skin with nails and hair and the oral mucosa with teeth. Pathology can manifest itself at any age, in any set of symptoms and with any severity. This can only be dry skin with small spots of atrophy and an almost complete absence of teeth, or baldness with no nails and moon-shaped defects in the tooth enamel with a full set of teeth. It is also possible that there is simply a decrease in the number of sweat glands in the skin, which leads to rapid overheating already in infancy and the danger of sudden death.
The vast majority of those suffering from genetic connective tissue dysplasia may experience disorders of all body systems from minor to life-threatening and with any set of symptoms: neurological disorders, heart valve defects, skeletal changes, vascular aneurysms, softening of the tracheal rings, prolapse of the kidneys, and also leading to sudden death due to combined damage to the cardiovascular and respiratory systems. The most active surge in manifestations is observed in adolescence, when, for example, scoliosis and flat feet progress sharply, cardiac arrhythmia and myopia appear. Several syndromes with characteristic external manifestations have been formed, again with variable severity - from scanty individual manifestations to extremely pronounced ones with early death from complications, such as Marfan syndrome and osteogenesis imperfecta.
Joint dysplasia is manifested by congenital malformations of large - hip and knee, as well as small joints of the hand and foot, and in essence can be considered the same connective tissue dysplasia, but in a separate articular system. As a rule, the pathology is detected in infants, but in a minimal form it can go unnoticed, which is discovered during an examination for an accidental leg injury.
Fibrous dysplasia is indicated by single and multiple cysts in the bones. Some people live healthy lives into old age and learn about genetic pathology in the form of a small brush by chance during an X-ray for another reason. Others suffer from chronic pain and limb deformity, often with shortening, due to multiple cystic cavities in the bone tissue.
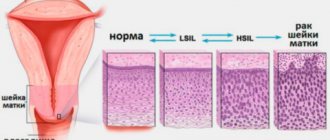
Dysplasia of the mucous membranes of internal organs is “earned” during life. In most cases, the process does not manifest symptoms or has uncharacteristic and unstable minimal signs, which are found by microscopy of a piece of tissue. Dysplasia can progress from mild, through moderate and severe, up to stage zero cancer - and this is its main danger. Severe dysplasia is difficult, and sometimes impossible, to reliably distinguish from non-invasive carcinoma in situ.
Gastric dysplasia can be clinically manifested by gastric pathology; the patient is often infected with Helicobacter. The pathology lies in the simplification of the cellular structure - decreased differentiation, changes in cell nuclei and other intracellular structures. Mild dysplasia not only turns into moderate, but also regresses; moderate dysplasia proceeds similarly, while severe dysplasia is considered a precancerous process and is subject to serious treatment and observation. Gastric dysplasia in frequency of occurrence is significantly inferior to metaplasia - the formation in the mucosa of areas of cells very similar to the cells of the large or small intestine. During microscopy, areas of intestinal metaplasia are always found around any dysplasia, and this is also a precancerous process.
Primary urothelial dysplasia is an uncommon pathology, manifested by symptoms of an irritable bladder with frequent and painful urge to urinate. This variant of dysplasia is not usually divided into degrees; the probability of developing cancer on a dysplastic background is slightly more than 15% and the transition to stage zero cancer will take from 4 to 8 years.
Cervical or dysplasia of the cervical mucosa is a very common pathology, since its leading cause is infection with the human papillomavirus. The virus itself cannot be killed - it is resistant to any drugs, but it is fatal and in the vast majority of women it will heal on its own in the next two to three years.
Therapy tactics
Therapy for hip dysplasia implies a comprehensive approach to the problem and should begin as soon as possible from the day the disease is diagnosed. Treatment includes the following standards:
- Massage sessions include 10 procedures, increasing or decreasing the number of procedures depends on the level of damage to the problem joint and the age of the patient.
- Orthopedic products – patients are prescribed to wear specialized underwear and bandages. An orthopedist selects the necessary products for patients based on the complexity of the disease and the individual characteristics of the body.
If the disease is complicated by coxarthrosis, then the following medications are included in therapy:
- PNNS - help reduce swelling and inflammatory reactions in soft and cartilage tissues. Therapy is carried out with tablets, rectal suppositories, injections: Indomethacin, Diclofenac, Ibuprofen.
- Muscle relaxants - help reduce muscle spasms: Baclofen, Sirdalud, Mydocalm, Tizanidine.
- Hormonal drugs - prescribed for complications of aseptic or autoimmune origin, to quickly solve the problem of joint inflammation: Prednisolone, Dexamethasone, Metypred.
- Chondroprotectors - used to accelerate the regeneration of cartilage discs, treatment has a long duration: Dona, Artra, Toad Stone, Teraflex, Structum.
Drug therapy is classified as a secondary subgroup of care, which helps get rid of the symptomatic manifestations of the disease during complications.
Physiotherapeutic procedures and exercise therapy
Common methods include:
- electrophoresis - helps stimulate metabolic processes at the tissue level, restore normal blood circulation, increase the tone of the muscles of the gluteal region, and deliver the medication unchanged to the affected area;
- applications with ozokerite, paraffin - procedures help improve the quality of tissue nutrition due to improved blood circulation, improve the range of motion of the diseased joint, reduce pain, and the inflammatory reaction;
- UFO accelerates the production of vitamin D, has an antibacterial spectrum of action, and stabilizes blood circulation.
Therapeutic exercises are recommended for all patients, regardless of age. Special exercises help increase muscle tone and strengthen the ligamentous-tendon system. Classes are conducted under the supervision of an instructor.
Diagnostics of DTS
If, during a daily massage or playing with your child, you discover one or more symptoms of dysplasia, you can try to find information on forums and Internet sites yourself. But the only right decision on subsequent actions will be to immediately contact an orthopedic doctor.
Only a competent doctor, after examining the patient, can confirm your fears or conclude that he is healthy. If a disease is suspected, a referral will be given for an ultrasound examination of the hip joints or an x-ray.
Ultrasound is a completely harmless method, which, however, does not provide a complete picture of the condition of the joint. Therefore, it is used mainly for preventive examinations of infants up to six months.
For children older than this age, or if there are still controversial issues after the ultrasound examination, the doctor will insist on an x-ray of the joint. This diagnostic method is more reliable, but there are difficulties in its implementation. Since in order to obtain an accurate result, the child must lie still during the procedure, which is quite difficult at this age. You can significantly simplify the process by doing the examination while the little patient is sleeping.
X-ray of the hip joint
To understand how to interpret an x-ray, you need to know the norms of the angle of the hip joint, as well as the numbers characteristic of different degrees of dysplasia. These data can be found in the table below.
| Age | Normal joint | Subluxation | Dislocation | High dislocation |
| up to 4 months | 25-30 | 30-35 | 35-40 | >40 |
| 5 months – 2 years | 20-25 | 25-30 | 30-35 | >35 |
| 2-3 years | 18-23 | 23-28 | 28-33 | >33 |
Surgery
Surgical intervention is prescribed in the following cases:
- late diagnosis of pathology;
- lack of results from conservative methods;
- complete dislocation of the joint with complicated dysplasia;
- repeated dislocation after closed surgery.
Even if the surgical method is effective, a rather long period of rehabilitation will be required, which is largely determined by the severity of the disease.
Important! The older the child, the lower the likelihood of successful reduction of the femoral head.
Possible consequences
Prolonged ignoring of the symptomatic manifestations of the pathology, a long-term hidden process can lead to the formation of arthrosis in the hip joint in the age range from 25 to 55 years.
Complications of dysplasia in the hip joint in childhood are:
- clubfoot, flat feet;
- lameness – a consequence of lameness can be the development of scoliosis;
- waddling gait – with bilateral lesions.
When children are ill, they begin to walk later than their peers, and their gait is unsteady. There is a risk of developing lumbar lordosis, thoracic kyphosis, and osteochondrosis. Lack of therapy leads to the degeneration of unilateral dysplasia into bilateral, and in complex cases – to loss of ability to work and disability.
Instrumental diagnostic methods
Many mothers are interested in the question: how to determine dysplasia in newborns with one hundred percent certainty? In order to clarify the diagnosis, it is necessary to perform the following diagnostic procedures.
X-ray examination - Before taking an image, the following conditions must be met: symmetrical positioning of the newborn, minimum procedure time, use of protective pads. When taking radiographs, it is necessary to involve assistants or parents who will help fix the baby in the desired position. TS dysplasia has characteristic X-ray signs:
- obliquity of the roof of the acetabulum;
- departure of the femoral head from the central axis;
- discrepancy between the size of the glenoid cavity and the size of the head;
- displacement of the thigh outward from the vertical line.
Arthrography allows us to judge the X-ray negative elements - ligaments, capsule. Using this method, even grade 1 hip dysplasia can be established. On an arthrogram it is possible to determine the position of the head and its shape, fibrosis of the capsule, fusion of the acetabulum. The procedure is performed under general anesthesia. A thin needle pierces the skin, subcutaneous fat, capsule, and penetrates into the cavity of the vehicle. A contrast agent containing iodine or an inert gas is injected. X-rays are then taken.
Arthroscopy - A conductor with a camera is inserted into the joint cavity, and an image of all elements is displayed on the TV screen - bone surfaces, ligaments, cartilage.
Ultrasound examination of the vehicle. Advantages: the possibility of repeated use to monitor treatment, no radiation exposure compared to radiography. The method is non-invasive, safe for the child. Ultrasonography can detect congenital hip dislocation in the early stages. Ultrasound is performed for the following indications:
- presence of clinical manifestations of DTS;
- severe pregnancy and childbirth;
- decreased muscle tone in the lower extremities.
Computed tomography allows you to evaluate additional radiological indicators - the degree of atrophy of the soft tissues surrounding the joint. The main disadvantage of the method is the high radiation dose, even with a single examination. Magnetic resonance imaging is used to determine indications for surgical treatment.