The “classical” operation for varicose veins under anesthesia with incisions in the groin area and along the legs, which was used to remove superficial varicose veins at the beginning of the last century, is an atavism of the past. The suffering of patients, long hospitalization and pain in the legs after such operations aimed at improving blood flow are completely unjustified. Severe varicose veins can be treated without resorting to “inquisition methods.” Today, treatment of advanced varicose veins can be carried out without anesthesia and hospitalization. The work of a phlebologist becomes office-based, without the attributes of major surgery.
Knowledge of what causes varicose veins in the legs allowed us to develop hemodynamic principles of treatment. Their implementation is possible by removing or switching off the vein from the blood circulation. Modern technologies are based on the principle of fusion of vein walls in the area of insufficient venous valves. The method of influencing venous circulation can be different, but its goal is the same - to stop the pathological discharge of blood through the affected vein (anti-reflux). At the Innovative Vascular Center, there are methods for effective treatment of varicose veins of the lower extremities without the slightest incisions or scars, eliminating both the causes and signs of venous pathology. Phlebologists at our center are pioneers in the introduction of modern technologies for varicose veins. Our clinics successfully treat more than 1,000 phlebological patients per year. We are responsible for the results of our operations for varicose veins of the lower extremities and provide written guarantees.
Medical history
The history of varicose veins began in the times of Byzantium, Ancient Egypt, and Old Testament Israel, as evidenced by archaeological excavations. In different eras, people tried to treat this disease, in particular, Avicenna and Hippocrates did this. In the second half of the 19th century, Russian and German doctors started talking about the effectiveness of ligation of the great saphenous vein.
This is what varicose veins of the lower extremities look like
At the beginning of the 20th century, very traumatic operations were carried out in Russia, during which the tissues of the thigh and lower leg were deeply dissected, veins were damaged, which were then ligated, nerve endings, arteries, and lymphatic ducts. Healing took a very long time, leaving large and noticeable scars.
In 1908, foreign doctors proposed removing the great saphenous vein and introduced a metal probe, which reduced injury to the patient. This was the first step towards minimally invasive surgery.
The breakthrough came when it became possible to take X-rays. It was first performed for varicose veins in 1924. At the same time, contrast based on strontium bromide solution was injected into the vein. Then ultrasound appeared, and the technique was further improved.
In the late 90s of the 20th century, laser therapy appeared, which became a modern breakthrough in the treatment of varicose veins.
Watch our video in which a doctor from Dr. Gruzdev’s clinic talks in detail about what varicose veins are:
Prevalence of the disease
Today, varicose veins of the lower extremities are the most common vascular pathology. About 20% of men and 40% of women suffer from various forms of this disease i Kenzhebekov E.T. Surgical treatment of patients with varicose veins of the lower extremities / E.T. Kenzhebekov, E.N. Zhanikulov, M.K. Ismailov // Bulletin of KazNMU. - 2021. - No. 1. - P. 299-300.. In Russia, varicose veins are diagnosed in 30 million people i Zadorozhny V.D. Modern methods of surgical treatment of varicose veins / V.D. Zadorozhny, V.M. Rzhevskaya // Bulletin of the Council of Young Scientists and Specialists of the Chelyabinsk Region. - 2021. - No. 4 (23). — T. 3..
Preparing for surgery
In cases where vein surgery is scheduled, it is necessary to undergo a preliminary preparation process organized in accordance with certain requirements. What does it include? In order for the operation to take place, regardless of whether the laser vein removal method or phlebectomy is chosen, you need to undergo a number of tests:
- general clinical urine and blood tests;
- coagulogram or hemostasiogram to assess the coagulation system;
- blood tests for AIDS, HIV, hepatitis B and C;
- blood group and Rh test;
- blood chemistry.
In addition to taking tests, preparation for surgery includes examinations such as:
- fluorography;
- electrocardiogram.
After the patient has been tested and undergoes the necessary examinations, it will be necessary to obtain a conclusion from a therapist. If the test results do not reveal any abnormalities and the examination results do not reveal concomitant diseases in the acute stage, the patient will receive a conclusion about the possibility of undergoing surgery for varicose veins of the lower extremities. Otherwise, the surgical intervention can be either canceled or postponed, due to the fact that in order to obtain a conclusion from the therapist, repeated tests and/or additional examinations and consultations with various specialists will be required.
How to prepare for surgery on the day of surgery?
!
You must stop eating at least 7 hours before.
Take a hygienic shower. If varicose veins have affected the veins of both lower extremities, then you will need to remove hair from both legs, starting from the inguinal fold. Surgical treatment will be carried out after examining the patient by an anesthesiologist.
Expert opinion
You should first purchase compression garments. It will be useful after the operation. It is also worth worrying in advance about comfortable, loose-fitting clothes made from natural materials.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Possible consequences of vein surgery
Causes of the disease (etiology)
The main cause of varicose veins is genetic predisposition.
There are a number of other provoking factors:
- sedentary lifestyle;
- pregnancy;
- obesity;
- hormonal disbalance;
- endocrine diseases;
- taking oral contraceptives and other hormonal drugs;
- work in hot shops;
- strong physical activity;
- work that involves standing on your feet for a long time or, conversely, sitting;
- chronic diseases of the bronchi and lungs, accompanied by a prolonged cough.
Contraindications
Experts consider any actions that can cause additional stagnation in the vessels of the lower extremities to be contraindications for varicose veins on the legs. These include:
- staying in static positions for a long time;
- lifting weights;
- sitting with legs tucked or crossed.
Patients should also avoid drinking alcohol, which increases blood viscosity and weakens the walls of blood vessels. Smoking can also negatively affect the course of the disease. Therefore, after diagnosis, it is necessary to give up bad habits.
Symptoms of varicose veins
The first symptoms that appear in the initial stages:
- legs get tired quickly;
- short-term swelling appears;
- there is pain in the veins;
- At night there are cramps in the calves;
- There is a feeling of burning, fullness, heaviness in the legs.
A characteristic feature of pain in chronic venous diseases is its localization in the calf muscles. The pain is never sharp and does not radiate to the hip or foot. The sensations are moderate, pulling, dull, appear in the evening, disappear after a night's rest i Zhane A.K. Possibilities of diagnosis and treatment of chronic diseases of the veins of the lower extremities / A.K. Zhane [et al.] // Kuban Scientific Medical Bulletin. - 2010. - No. 9 (123). - pp. 78-84..
There are no dilated veins in the initial stages, but the disease is already developing. Sometimes this takes decades.
Gradually the symptoms intensify, signs of venous insufficiency appear:
- Swelling of the legs. In patients with chronic venous diseases, the volume of superficial tissues in the distal parts of the leg usually increases, while swelling, as well as pain and heaviness, occurs in the afternoon and regresses by the morning. Swelling of the foot, which is a symptom of disorders of lymphatic edema (lymphedema), is not typical for venous pathology. i Zhane A.K. Possibilities of diagnosis and treatment of chronic diseases of the veins of the lower extremities / A.K. Zhane [et al.] // Kuban Scientific Medical Bulletin. - 2010. - No. 9 (123). - pp. 78-84..
- Skin itching.
- Nodes visible to the naked eye, dilated veins, pathological tortuosity.
- Darkening, thickening of the skin, acquiring a brownish or bluish tint.
As the disease progresses, the symptoms intensify, signs of nutritional deficiency in the legs appear - deterioration in the condition and appearance of the skin, eczema, trophic ulcers.
Main symptoms and signs of varicose vascular pathology
The main symptomatic signs of structural venous disease include:
- pain during prolonged stays in an upright position and when walking;
- regular nocturnal attacks of local convulsive syndrome;
- feeling of heat and burning of the skin in the calf muscles;
- a pronounced feeling of fatigue and swelling of the lower extremities, with a disorder of superficial and deep sensitivity;
- bursting pain both during the day and at night;
- pathological changes in the color and trophism of the integumentary epithelium are manifested by severe dryness of the skin, the appearance of trophic ulcers on the leg and areas of hemorrhage in the area of rupture of damaged venous vessels. Formed ulcers on the skin are difficult to regenerate and are easily susceptible to bacterial infection;
- pronounced deformation and expansion of the walls of venous vessels under the influence of increased pressure. Deformed vessels are visible through the skin with the naked eye.
Why varicose veins are dangerous: possible complications of the disease
Thrombophlebitis
- life-threatening condition. When it occurs, blood clots form in the veins, which can break off and clog the pulmonary vessels, leading to myocardial infarction. If a large vessel is affected, death is possible.
Venous thrombosis
- blockage of a vessel with a blood clot. It manifests itself as pain in the limb, which intensifies with physical activity, and swelling.
Pulmonary embolism
– blocking of the lumen of the pulmonary artery by a detached thrombus. Death can occur in the first 30 minutes. If the thrombus is small, then a pulmonary infarction occurs and the patient requires resuscitation measures. The condition is accompanied by pneumonia and chronic heart failure.
Trophic ulcers
– compaction of the subcutaneous tissue, darkening and thinning of the skin with the subsequent appearance of ulcers. Such ulcers exist for a long time, do not respond to treatment, and close very slowly.
What can varicose veins lead to?
Complications of venous insufficiency
Varicose veins are a chronic incurable disease, so treatment has certain goals - to stop the progression and prevent complications. If the treatment is prescribed incorrectly or the patient does not seek help from a medical specialist, complications of the disease develop.
Thrombophlebitis is inflammation of the vein walls in the presence of a blood clot. Nearby vessels and soft tissues may be involved in the inflammatory process. There are several forms. It can be acute (lasts about 30 days), subacute - lasting up to six months, and chronic.
Migrating thrombophlebitis is rare. It is characterized by inflammation that occurs in different parts of the vein and resolves quickly.
Symptoms of acute thrombophlebitis include:
- A clear outline of the inflamed vessel is visually visible.
- Acute pain syndrome, with palpation the pain becomes stronger.
- Swollen nodules protruding above the skin.
- Local increase in temperature.
Thrombophlebitis with varicose veins of the legs can lead to other complications. For example, to periphlebitis - inflammation of surrounding tissues, wet gangrene of the extremities, deep vein thrombosis. When inflammation spreads, complications appear that extend beyond the limbs - thromboembolism and sepsis.
Deep vein thrombosis is a common complication of varicose veins of the legs. The pathology is characterized by the formation of a dense blood clot, which completely or partially clogs a blood vessel, which impairs proper blood circulation. With this complication there is a risk of death due to blood clot rupture.
Trophic ulcers appear in severe cases. An infectious process is often associated, which aggravates the clinical picture. Wounds can affect not only tissue, but also deeper layers - muscles. They heal for a long time. Complex treatment is required.
Varicose eczema is characterized by the following symptoms:
- Inflammatory hyperpigmentation of the skin, purple or bright red;
- Microvesicles are formed, which open on their own;
- Severe swelling of the legs;
- Skin itching that occurs constantly;
- Weeping, which after drying becomes covered with a crust;
- Abnormal thickening of the skin.
Varicose eczema can become chronic, resulting in hardening of the skin and subcutaneous tissue.
When an infection occurs, eczema is complicated by trophic ulcers.
Risk factors for developing varicose veins
- Heredity.
Weakness of the vein walls is passed on to children. If both parents have varicose veins, then the child has a 90% chance of getting the disease. If only one has 60%. - Pregnancy.
During pregnancy, varicose veins are provoked by three factors:- Changes in hormonal levels - the production of large amounts of progesterone. This hormone relaxes the muscles, so the veins become more vulnerable.
- Pressure of the uterus, which increases in size. In this regard, the outflow of blood from the legs worsens.
- An increase in the amount of blood by an average of 20-30%. Venous valves cannot withstand such stress, especially if they were naturally weak.
- Obesity and simply being overweight
, which is accompanied by lipid metabolism disorders. This process causes vascular pathologies. - Poor nutrition
– predominance of fried foods, fatty foods, fast food, animal fats, milk fats. Uncontrolled consumption of salt and sugar, semi-finished products. - Hormonal background
- a surge in hormone production can weaken the muscle layer of the vein walls, which expands the lumen of the vessel and prevents the normal closure of the valves. - Incorrect clothing
, which negatively affects blood circulation. Pants that put pressure on the waist, tight belts, and too-tight jeans, the fabric of which lacks elasticity, have a negative impact on the condition of the veins. - High-heeled shoes
, which cause the veins to work to the limit. This is due to the fact that the load is unevenly distributed - the main part of it falls on the forefoot, the vessels of which are under too much pressure. Women who wear high-heeled shoes usually note that in the evening their feet hurt, ache, and swell. These are the first signs of beginning varicose veins.
What is reticular varicose veins
In the human body, blood circulates through arteries, veins, capillaries, and venules. Arteries are the largest vessels of the circulatory system. They connect to the veins. The smallest vessels are venules. On the lower extremities, superficial intermediate venous vessels are visible under the skin. Their diameter is greater than the diameter of the capillaries, but less than the diameter of the main veins. This venous network is called reticular. In other words, reticular veins are small millimeter-sized vessels that are visible under the skin of the legs.
Every vein has valves. They filter the direction of blood movement and its volume. The reticular vein has only one valve. If it is deformed, the vein expands, twists and carries a larger volume of blood. Venous pressure in the retinal layer of the skin increases due to the accumulation of blood in a certain area. Valve insufficiency develops and reticular varicose veins form - a plexus of small vessels of red, blue, purple color, visible through the skin.
Degrees of varicose veins
Currently, it is generally accepted in world phlebological practice to use the classification of chronic venous diseases, called CEAP. The distribution of patients into clinical classes is based on visual symptoms of chronic venous disease. There are seven clinical classes in total:
- Class C0. There are no visible symptoms of the disease upon examination and palpation, but there are characteristic complaints.
- Class C1. Telangiectasia and reticular veins.
- Class C2. Varicose veins.
- Class C3. Swelling, pain, heaviness and fatigue in the calf muscles.
- Class C4. Trophic disorders (skin pigmentation, lipodermatosclerosis).
- Class C5. Skin changes mentioned above + healed trophic ulcer.
- Class C6. Skin changes as above + open ulcer.
Where varicose veins can occur: areas of localization of the disease
Lower limbs
The most common localization. It usually appears at a young age, and in women - during pregnancy or after childbirth. In the initial stages, symptoms are few and nonspecific - leg fatigue, heaviness in the legs, burning, bloating, night cramps. Already at the very beginning of varicose veins, pain and swelling appear along the vein. Usually the ankles, legs, and feet are affected.
Upper limbs
The most common symptom in this case is numbness in the hands. It can be partial or complete, most often manifesting itself during sleep. The patient becomes weather dependent, his hands hurt and ache with any weather changes. It becomes difficult to hold even light objects in your hands. Then more characteristic symptoms develop - the vessels swell, nodes form, pain begins, intensifying over time, the veins become tortuous and prominent.
Groin and pelvis
Manifestations of the disease differ in men and women.
Among women
There is itching, swelling of the labia, heaviness in the pelvic organs, and bursting pain. If natural childbirth occurs against the background of varicose veins, bleeding may develop.
The disease can occur in the form of venous congestion syndrome. In this case, there will be pain in the lower abdomen, radiating to the sacrum, groin, lower back, and perineum. Their intensity will vary depending on the phases of the cycle. Pain will occur during intimacy, standing or sitting for a long time.
In men
In mild stages there are almost no symptoms. As the disease progresses, aching pain appears in the lower abdomen and perineum. The pain may radiate to the lower back and intensify during intimacy and after ejaculation. The scrotum and perineum also swell. In the later stages, urination becomes more frequent.
Signs
The disease at the initial stage is latent. You can suspect the reticular form of varicose veins of the lower extremities by the bluish color of the skin. Thin veins appear on the legs in the form of:
- tree-shaped (many vessels branch from one base to the left and right);
- cobwebs or stars (vessels extend from the center in different directions);
- lines (even stripes of blood vessels).
Branched veins are especially noticeable at the end of the day after sports, heavy lifting, prolonged static position, running or walking long distances. In the morning the defect on the legs is invisible.
As blood flow worsens, accompanying symptoms worsen:
- discomfort in the calf muscles. Involuntary spasms occur suddenly and disappear after massage of the limbs;
- heaviness and fatigue in the legs;
- burning and itching in the legs and feet.
The clinic is more pronounced during menstruation due to increased blood flow.
Symptoms subside after resting while lying down with legs elevated. Unlike varicose veins of deep veins, there is no pain, swelling and trophic disturbances.
Methods for diagnosing varicose veins
In the early diagnosis of chronic venous diseases, the most widely used ultrasound methods are Dopplerography and angioscanning.
Doppler ultrasound (USDG) is the simplest way to objectively assess the peripheral vascular bed, based on changes in the frequency of the ultrasound signal reflected from the blood cells (Doppler effect). Doppler ultrasound assesses the condition of the vessel based on indirect signs: the presence of spontaneous blood flow, the reaction of blood flow to functional tests (Valsalva breathing test, muscle compression above and below the ultrasound sensor). An important task of ultrasound examination is to determine the ankle-brachial index (the ratio of pressures on the posterior tibial and brachial arteries). Normally, this indicator exceeds 1.
Ultrasound angioscanning (USAS) is the most informative method of non-invasive examination of peripheral vessels. It allows you to obtain a two-dimensional image of the vessel, visualize intravascular structures (venous valves, thrombotic masses, endovasal devices, etc.), as well as assess the nature and direction of blood flow.
In complex diagnostic cases, when USAS does not allow obtaining a complete answer about the nature and extent of damage to the vascular bed, they resort to computed tomography (CT) .
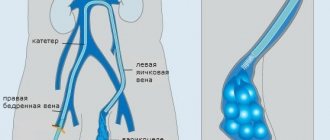
X-ray contrast venography is used in the diagnosis of acute venous thrombosis and their consequences, arteriovenous angiodysplasia, as well as varicose veins of the small pelvis.
Methods for treating varicose veins
Surgical techniques
A complete cure for varicose veins is possible only after surgical treatment. It can be carried out in three ways:
- Phlebectomy – removal of varicose veins.
- Sclerotherapy is the introduction of a sclerosant into a varicose vein - a special substance that “glues” its walls, stopping blood flow through it. As a result, the vein collapses, even the cosmetic defect disappears.
- Laser coagulation - the walls of the vein are destroyed due to thermal effects, as a result of which the venous lumen is “sealed”. Such an operation can be performed only if the vein is dilated by no more than 10 mm.
Also, one of the most modern methods of treating chronic varicose veins is adhesive obliteration of veins VenaSeal .
Sclerotherapy Sclerotherapy is a method of treating varicose veins by injecting a sclerosant (a special medication) into the affected veins.
More details
FILM sclerotherapy The newest and unique method of combating varicose veins of any size.
More details
Adhesive obliteration of veins VenaSeal Non-surgical treatment of chronic venous insufficiency and varicose veins using VenaSeal bioadhesive.
More details
Endovasal laser coagulation (EVLC) If you have varicose veins, this does not mean that you will have to have surgery! New medical technologies make it possible to get rid of this disease without surgery.
More details
Phlebectomy Phlebectomy is a minimally invasive operation to remove varicose veins in the legs through a puncture or incision.
More details
Miniphlebectomy Miniphlebectomy is an operation to remove veins using microscopic incisions and punctures.
More details
Drug treatment
Venotonics play a leading role in drug treatment
, which are taken in tablet form and act systemically. They correct disturbances in circulatory function. As a result, the blood vessels of the whole body are healed. Venotonics are also available in the form of gels and ointments, but they are less effective and act only at the site of application for a short time.
Phlebotonics are also used
– venotonic drugs. They are indicated for thinning of the walls of blood vessels, reduced elasticity, increased permeability, and blood stagnation. The drugs strengthen the venous walls, increase their elasticity, eliminate congestion, reduce swelling and other negative symptoms. An additional property of phlebotonics is the normalization of microcirculation in the affected area.
Antiplatelet agents are used to thin the blood
. The drugs are used when it is necessary to reduce the intensity of blood clot formation. Indicated for patients with increased blood viscosity. Antiplatelet agents can be used only if there is no tendency to bleeding.
Anticoagulants are also prescribed to stop the thrombus formation process.
. They destroy blood clots and reduce blood viscosity.
Compression therapy
A good helper in the fight against varicose veins is compression knitwear. The operating principle of such products:
- Throughout the length of the compression stocking, pressure is applied to the superficial and deep veins.
- The greatest pressure is at the bottom, where the veins are most narrowed and the outflow of blood is fastest.
- Thanks to the narrowing of the veins, the efficiency of the valves increases.
- Swelling, pain, and fatigue in the legs go away.
Conservative treatment of varicose veins of the legs
Conservative treatment of varicose veins includes medication and wearing compression garments. Compression hosiery differs in compression class and purpose - it can be used for the prevention and treatment of pathology. Tights, stockings and knee socks should be selected by a doctor taking into account specific characteristics. Only the right underwear gives the desired result.
Medicines are prescribed. There is no ideal effective medicine that would affect all pathological parts of the disease. It is recommended to use systemic medications - tablets and local remedies - gels, balms, creams and ointments.
To normalize the tone of the vascular wall, eliminate venous congestion and improve microcirculation at the cellular level, the following venotonics are prescribed:
- Detralex.
- Phlebodia 600.
- Lyoton gel.
- Antistax (dietary supplement).
- Venitan.
- Venarus.
- Troxerutin.
The dosage and method of application are determined individually, as is the duration of the course for varicose veins of the legs. Self-administration is prohibited. The drugs can lead to side effects in the form of an allergic reaction and dermatological diseases that are difficult to treat.
For the prevention and treatment of thrombosis, improving the rheological properties of blood, medications are prescribed:
- Thrombo ACC;
- Aspirin;
- Chime;
- Venolife;
- Hepatrombin;
- Heparin ointment, etc.
To relieve pain and severe swelling, non-steroidal anti-inflammatory drugs are used. Diclofenac is most often prescribed in the form of a cream for external use.
Additionally, physiotherapeutic procedures are prescribed - magnetic therapy, electrophoresis; special gymnastics. You can use folk remedies - recipes with medicinal herbs help reduce the severity of symptoms.
Sometimes hirudotherapy is recommended - treatment with leeches.
Ways to prevent varicose veins
- People at risk, especially those with a hereditary predisposition, need to regularly visit a phlebologist and have an ultrasound scan to diagnose the disease at an early stage.
- It is necessary to do leg exercises regularly if you sit for a long time.
- The diet should include foods that improve liver function - tomatoes, carrots, olives, apples, blueberries. Thanks to the good functioning of the liver, the blood does not stagnate and thins out.
- Prevention of constipation is necessary, because regular constipation is a direct cause of stagnation of blood in the legs.
- You need to get proper rest, especially for women, who need 2-3 times more time to recuperate than men. You need to lie with your legs slightly elevated, and in case of swelling and fatigue, do foot baths with sage, chamomile or calendula.
- In the hot season, you need to drink as much as possible - at least 2 liters per day and not stay in the sun for a long time. Otherwise, the thickness and viscosity of the blood will increase.
- Swimming is very beneficial. During this, the legs cool down and work well while in a horizontal position.
Addresses of our clinics:
St. Petersburg, Manezhny lane, 13 m. Chernyshevskaya
St. Petersburg, st. Bolshaya Raznochinnaya, 27 metro station Chkalovskaya
Horse chestnut tincture for varicose veins
After three courses you will notice an improvement. To prepare the tincture, horse chestnut flowers (50 grams) need to be poured with half a liter of alcohol, then let it brew for 14 days, shaking the bottle every day. Pass the tincture through the mesh and take a tablespoon with water three times a day before meals. Once you have been treated for a week, take a break for two weeks. Then treatment can be started again.
Read more: video recipe for making horse chestnut flower tincture
Reviews from patients of our clinic
Semenenko O.A.
The clinic treated varicose veins of the legs. The treatment result is excellent. I thank all the clinic staff for their kind and attentive attitude and wish them success in their work.
Filatova Karina Karpovna
Many thanks to all the staff of the clinic and personally to Vitaly Alexandrovich Kiselev. Treated varicose veins. Everyone was very attentive and responsive. Your clinic has a high professional level. I will recommend it to all my friends.
Gubanova T.P.
For many years I suffered with varicose veins. My legs were terrible, painful, and bluish veins were sticking out. And my son, seeing my suffering, agreed on an operation with Dr. Nikolai Andreevich Spiridonov. I was so afraid and worried, but I lay down on the operating table.
The operation was completely painless, I did not believe that it was all over. 3.5 months have passed since the operation. I am so grateful to my doctor and the entire clinic team. You give us health!!! Low bow to you!!!!
Read all reviews about the clinic
FAQ
Who to contact for varicose veins?
Varicose veins are treated by a phlebologist. You can learn more about phlebologists from our article or make an appointment online with one of our doctors in St. Petersburg.
How to cope with leg fatigue with varicose veins?
You need to lie with your legs slightly elevated (put a sofa cushion under them) and do foot baths with chamomile, sage or calendula.
What is the nature of pain with varicose veins?
Pain varies from patient to patient. It can be stabbing, dull, aching, sharp in areas of varicose veins, bursting, hot pulsating, aching, burning.
Is alcohol bad for leg veins?
A doctor at our clinic will answer this question:
Sources:
- Zhane A.K. Possibilities of diagnosis and treatment of chronic diseases of the veins of the lower extremities / A.K. Zhane [et al.] // Kuban Scientific Medical Bulletin. - 2010. - No. 9 (123). — P. 78-84.
- Kenzhebekov E.T. Surgical treatment of patients with varicose veins of the lower extremities / E.T. Kenzhebekov, E.N. Zhanikulov, M.K. Ismailov // Bulletin of KazNMU. - 2021. - No. 1. - P. 299-300.
- Komarova L.N. Results of treatment of patients with varicose veins of the lower extremities over 10 years / L.N. Komarova [and others] // Archives of Internal Medicine. - 2021. - No. 3. - P. 215-218.
- Kukeev T.K. Chronic venous insufficiency: current state of the issue / T.K. Kukeev [and others] // Bulletin of AGIUV. - 2011. - No. 4. P. 35-38.