What it is?
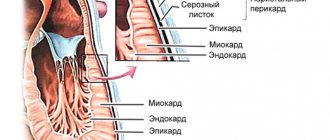
Atrial fibrillation is a rhythm disorder in which the muscle fibers of a given part of the heart contract not just at random, but also with enormous frequency - from 300 to 600 beats per minute.
In this case, the process is uncoordinated, chaotic and also leads to ventricular dysfunction. Externally, this “dancing” of the heart is manifested by an increase in heart rate. The latter is often difficult to feel, because it seems to flicker. It was this comparison that gave the pathology its second name – atrial fibrillation. Next to the formulation of the diagnosis on the disability certificate, you can find code I 48, which belongs to atrial fibrillation in the ICD 10th revision.
We have to admit that, despite the enormous achievements of medicine in the treatment of this disease, it remains a key cause of stroke, heart failure and sudden death. At the same time, an increase in the number of such patients is predicted. The latter is associated with an increase in life expectancy and, accordingly, the number of elderly people suffering from arrhythmia.
What is the difference between fibrillation and flutter
I would like to note that a common mistake is to equate these two rhythm disturbances. In fact, atrial fibrillation and atrial flutter have different genesis and manifestations. The first is characterized by:
- chaotic contraction of cardiomyocytes (heart muscle cells) with different intervals between them;
- the presence of multiple foci located in the left atrium and creating extraordinary pathological discharges.
Flutter is a milder version of arrhythmia.
Although the heart rate reaches 200-400 beats per minute, the heart beats at regular intervals. This is possible due to the coordinated contraction of muscle fibers, since the impulses come from one source of excitation. You can read more about this type of rhythm disorder here.
Traditional medicine recipes
How to relieve arrhythmia at home? For this, the following traditional medicine recipes will be useful, thanks to which you can quickly get rid of unpleasant symptoms, stabilize the heart rate and increase the level of the body’s natural defenses:
- Freshly squeezed juice from radish, carrots and beets, mixed in equal proportions, is taken daily in the first half of the day. Regular use of this drug significantly improves the general condition of all types of arrhythmia.
- Lemon zest with figs helps reduce heart rate.
- A decoction of the dried parts of peppermint is a very universal recipe that saves you from various forms of tachycardia. You need to drink it every day for a long time shortly before your first meal.
The following have good therapeutic properties: blood-red hawthorn, motherwort, beet juice with honey, calendula, lemon balm, valerian, hop cones, wild rosemary, foxglove, cornflower flowers and asparagus. For adults and children suffering from arrhythmia, it will be very useful to diversify your diet with foods rich in magnesium and potassium (bananas, buckwheat, oatmeal, dried fruits, new potatoes and nuts). It is best to eat food by dividing it into small portions. Otherwise, a full stomach causes irritation of the vagus nerve, which puts pressure directly on the sinus node.
Prevalence in society
Tachysystolic form of atrial fibrillation, which is the most common, occurs in 3% of adults aged 20 years and older. Moreover, older people suffer from the disease to a greater extent. This trend is explained by several factors:
- increasing life expectancy;
- early diagnosis of asymptomatic forms of pathology;
- the development of concomitant diseases that contribute to the appearance of atrial fibrillation.
According to the World Health Organization, in 2010 the pathology was detected in 33.5 million people on the planet.
It was found that the risk of getting sick in women is slightly lower than in men. But at the same time, the former are more often susceptible to strokes, have a greater number of concomitant diseases and a pronounced clinical picture of fibrillation.
Causes of the disease and genetic aspects
I would like to note that it is very important to distinguish the true cause of atrial fibrillation from factors that only contribute to the manifestation of the disease.
The pathology is based on a genetic mutation, a kind of “breakdown”. Even in the absence of associated cardiovascular risks, the chance of developing atrial fibrillation in patients with such a DNA defect is very high.
At the moment, about 14 variants of changes in the genotype are known that lead to rhythm disturbances. The most common and significant mutation is believed to be located on chromosome 4q25.
In this situation, a complex disruption of the structures and functions of the atrial myocardium occurs - its remodeling occurs.
In the future, it is planned to resort to the help of genomic analysis, which will improve the prognosis of the disease and reduce disability through early diagnosis of pathology and timely treatment.
Radiofrequency catheter ablation
Radiofrequency ablation has become the most effective treatment for atrial fibrillation today. The essence of the technique is to destroy the source of additional electrical impulses in the heart without open intervention. The operation is performed only in a specialized medical institution.
Before performing the manipulation, the doctor uses special devices to detect a pathologically changed area of the heart muscle. Then a special catheter is inserted into the femoral vein, which reaches the heart with blood flow. This catheter is capable of releasing radiofrequency electrical impulses that destroy the pathological focus. After the manipulation, the catheter is removed.
Diagnostics
The most informative method for diagnosing atrial fibrillation is an ECG.
But before that, the doctor will collect anamnesis. Important information will include information about:
- similar rhythm disturbances in close relatives;
- concomitant diseases, for example, pathologies of the lungs, thyroid gland, gastrointestinal tract;
- initial manifestations of menopause in women.
If the patient independently notices an irregular pulse, the doctor will ask how long these changes have been observed, and whether attempts have been made to eliminate them. This is followed by a physical examination, which will immediately provide a differential diagnosis for flutter. Indeed, with atrial fibrillation, heart beats occur at different intervals.
When listening, the ineffectiveness of the contractions of our “engine” will be revealed. This means that the heart rate determined in this case will differ from the pulse rate palpated on the wrist. The “floating” volume of the first tone will also attract attention. No matter how informative the physical examination is, in some cases with severe tachycardia the doctor is unable to understand the cause of the disease and give a conclusion about the irregularity of the rhythm. Then a cardiogram comes to the rescue.
Signs on ECG
An ECG examination of the patient, especially in old age, should be carried out during each visit to the doctor. This can significantly reduce the number of consequences of atrial fibrillation (ischemic stroke, acute heart failure) and improve the diagnosis of its latent (asymptomatic) and paroxysmal forms. Therefore, when you are recommended to undergo this procedure at an outpatient appointment or in a hospital, you cannot refuse, because many patients do not feel any interruptions in the functioning of the heart until a “vascular accident” occurs.
New techniques are being developed that will allow you to independently determine violations. For example, portable skin recorders, smartphones with ECG electrodes, blood pressure monitors with built-in arrhythmia detection algorithms.
But all of them are still inferior in terms of information content to a traditional cardiogram, on which the following changes are detected during atrial fibrillation:
- there is no P wave;
- RR intervals responsible for the ventricular rhythm have different lengths;
- ff waves are present, which are considered the main sign of the disease.
I draw your attention to the fact that to diagnose the paroxysmal form of the pathology, you should resort to either daily short-term ECG recordings or round-the-clock Holter monitoring.
The photo below shows examples of films of people with atrial fibrillation.
Classification of atrial fibrillation
There are currently three classifications of atrial fibrillation used by practicing cardiologists. Pathology is divided by:
- form (implies the duration of the arrhythmia, that is, paroxysmal, constant, persistent);
- the reason for its occurrence, or rather, according to the factor contributing to its development;
- degree of severity, taking into account the severity of symptoms that accompany heart rhythm disturbances.
Such a distribution is extremely important, as it allows the doctor to further determine the most effective way to treat the disease and prevent its secondary complications.
Forms
National cardiology guidelines list 5 forms of atrial fibrillation:
- newly identified;
- paroxysmal;
- persistent;
- long-term persistent;
- constant.
In some patients, the disease is progressive in nature, that is, rare short-term attacks of arrhythmia gradually become more frequent and longer lasting. As clinical experience shows, this situation ends in the development of permanent heart rhythm disturbances. Only 2-3% of patients can “boast” of periodic flickering for 10-20 years.
In this section, I would like to mention the atypical form of pathology included in Frederick's syndrome. The described disease belongs to the category of tachyarrhythmias, which are manifested by increased heart rate and different intervals between beats. But this extremely rare type of pathology, occurring in 0.6-1.5% of patients, is considered normosystolic, and sometimes bradysystolic. That is, the heart rate will be either within the normal range - 60-80 beats/min, or less than 60 beats/min, respectively.
Frederick's syndrome is a combination of fibrillation and third degree atrioventricular block. This means that the discharge from the atria simply does not reach the ventricles; the latter are excited by their own pacemaker.
A similar development of events is possible if the patient has severe organic pathologies of the heart, for example, ischemic heart disease, heart attack, myocarditis, cardiomyopathy.
First identified
Newly diagnosed is considered to be atrial fibrillation that was diagnosed at the moment, and there is no mention of its earlier detection. This type of atrial fibrillation can be either paroxysmal or permanent, asymptomatic and with a pronounced clinical picture.
You must remember that this classification form of heart rhythm disturbance is assigned regardless of the duration of the disease, which is quite difficult to judge in the absence of attacks of shortness of breath and palpitations, and the severity of its manifestations. And I note that when you seek medical help for this pathology again, the prefix “first identified” will no longer appear in the formulation of the diagnosis.
Paroxysmal
Paroxysmal atrial fibrillation is one that begins suddenly and disappears on its own within 1-2 days. Although there are also attacks of atrial fibrillation that last up to 7 days, they are also classified as this form of pathology.
With this course of the disease, patients periodically experience interruptions in the functioning of the heart, accompanied by shortness of breath, chest pain, weakness, dizziness, and fluctuations in blood pressure. Sometimes, against the background of these paroxysms, presyncope develops.
Persistent
Persistent atrial fibrillation is atrial fibrillation that lasts longer than a week. This also includes attacks that are eliminated only due to cardioversion or the action of medications after 7 days or more.
In practice, it is sometimes extremely difficult to differentiate between the paroxysmal and persistent types, since it is not always possible for the doctor and the patient to carry out such long-term ECG monitoring. Then certain difficulties arise in choosing the most effective treatment tactics. In some cases, there is an alternation of these two forms of rhythm disturbance.
Long-term persistent
Long-term persistent atrial fibrillation, or stable, “haunts” the patient for a year, and sometimes longer. The condition for such a formulation of the diagnosis is that for such a patient the cardiologist has chosen a heart rhythm control strategy. Moreover, some time after the onset of the pathology, a person at rest ceases to feel the characteristic symptoms. The clinic becomes pronounced only at the time of physical activity.
In such a situation, it is almost impossible for doctors to determine the duration of the onset of arrhythmia or the appearance of its last attack without appropriate medical history or medical documentation.
Constant
A long-term persistent disease, in which the doctor and patient decided not to take steps aimed at restoring normal sinus rhythm, subsequently acquires a different name. From now on, it is called the permanent form of atrial fibrillation.
This situation is also possible if attempts to “fix” the heartbeat have already been made, but failed. Then interventional transcatheter radiological technologies are simply not used.
And when the patient changes his mind and agrees to measures that will lead to rhythm control, the permanent form again turns into a long-term persistent one.
Clinical classification (by reason of pathology)
The clinical classification is designed to differentiate atrial fibrillation by trigger factors, that is, concomitant diseases or conditions that increase the risk of arrhythmia. After all, even though the genetic cause of the pathology was mentioned above, this does not mean at all that it will definitely develop. For a mutation to manifest itself, it needs to be “nudged.”
The table lists situations that contribute to the development of certain types of fibrillation.
| Fibrillation type | Cause |
| Secondary against the background of organic heart lesions | It is provoked by heart diseases, accompanied by left ventricular dysfunction, arterial hypertension with myocardial hypertrophy. |
| Focal | It is observed in young patients with a history of atrial tachycardia or short-term episodes of fibrillation. |
| Polygenic | Occurs at an early age against the background of multiple genetic mutations. |
| Postoperative | It is provoked by open cardiac surgery and usually resolves on its own as the patient recovers. |
| Fibrillation in patients with valve pathology | Develops with mitral stenosis, after surgical interventions to correct the valve apparatus. |
| Arrhythmia in athletes | It manifests itself in paroxysms and depends on the duration and intensity of exercise. |
| Monogenic | Formed in patients with a single gene mutation. |
I note that this division of atrial fibrillation by type is intended to adjust the treatment algorithms for the disease.
Modified EAPC scale
This scale is used to assess the patient’s quality of life, that is, it takes into account the extent to which signs of the disease interfere with his ability to perform daily work. After all, the treatment tactics for atrial fibrillation depend on the severity of the clinical picture.
Minimal symptoms are observed in 25-40% of patients, 15-30% report significant discomfort and a sharp limitation of physical activity against the background of manifestations of pathology.
The table shows the severity of atrial fibrillation.
| Degree | Severity of the clinical picture |
| 1 | There are no symptoms of the disease. |
| 2a | Signs of pathology are minimal and do not bother the patient. |
| 2b | Although the patient performs daily work, shortness of breath and palpitations are already felt. |
| 3 | The patient’s normal functioning is disrupted as a result of severe symptoms of arrhythmia (shortness of breath, palpitations, weakness). |
| 4 | A patient with this degree of severity of fibrillation is not able to care for himself. |
Heart rate monitoring
Keeping your heart rate within a reasonable range reduces the risk of recurrent atrial fibrillation. What are these limits?
Strict control (in younger people) involves a heart rate of 60-80 at rest and 90-115 during moderate exercise. In this case, control is carried out only by daily ECG monitoring.
For patients with a high risk of organ ischemia (primarily the brain) - and these are primarily old people - a heart rate of less than 110 per minute is acceptable.
For drug control, drugs of several groups are used:
- Beta blockers (Metoprolol, Atenolol, Carvedilol).
- Cardiac glycosides (Digoxin)
- Calcium channel blockers (Verapamil. Diltiazem)
- Antiarrhythmics (Dronedarone, Amiodarone)
- It is rational to combine a bkta blocker with a cardiac glycoside and an antiarrhythmic drug.
If the three-component scheme is ineffective, surgical correction is required.
Treatment of atrial fibrillation (atrial fibrillation)
Treatment of atrial fibrillation should be carried out comprehensively, that is, it requires interaction between primary care doctors (general practitioners, family doctors), to whom patients first turn for help, and more specialized specialists (cardiologists, cardiac surgeons). Only with this approach and continuous training of the patient in behavioral tactics for this pathology can positive results be achieved.
When choosing therapeutic measures, the following factors are taken into account:
- stability of hemodynamics (blood pressure indicators), severity of the clinical picture;
- the presence of concomitant cardiovascular and other diseases (thyrotoxicosis, sepsis, etc.), which aggravate the course of arrhythmia;
- the risk of developing a stroke and the need in this regard to prescribe blood thinning drugs (anticoagulants);
- Heart rate and the importance of reducing this indicator;
- symptoms of the pathology and the possibility of restoring sinus rhythm.
Only after a comprehensive assessment of the patient’s condition is a decision made on the tactics of his further management.
Stroke Prevention
It has long been proven that atrial fibrillation significantly increases the risk of ischemic strokes. This occurs due to the formation of blood clots in the chambers of the heart, followed by their migration into the vessels of the brain.
Therefore, treatment of a permanent form of atrial fibrillation, as well as other types of the disease, includes the use of blood thinning drugs.
Previously, everyone in such a situation was prescribed antiplatelet drugs (Aspirin Cardio, Cardiomagnyl) almost uncontrollably. But at present they have been proven ineffective in preventing thromboembolism. Now they are resorting to the use of vitamin K antagonists (Warfarin) and new anticoagulants that are not vitamin K antagonists (Apixaban, Dabigatran). Moreover, the prescription of the latter group of drugs is accompanied by a lower risk of developing hemorrhagic strokes (intracerebral hemorrhages).
Heart rate monitoring
There are two key strategies used by practicing cardiologists to combat atrial fibrillation. One of them is aimed at controlling heart rate, and the second is aimed at restoring physiological sinus rhythm. As you understand, the choice of tactics depends on many factors. These include the age of the patient, length of illness, and the presence of serious concomitant pathologies.
Treatment of the chronic form of atrial fibrillation in elderly people is most often based on the first of the above methods and can significantly reduce the manifestations of the disease and improve the daily activity of patients.
Relieving an attack
A rapid decrease in heart rate may be necessary against the background of newly detected fibrillation and with reversible tachysystoles that occur against the background of anemia, infectious pathologies, and decompensated thyrotoxicosis.
In such a situation, beta-blockers (Bisoprolol, Concor) and calcium channel blockers (Diltiazem, Verapamil) become the drugs of choice, as they have a rapid effect and affect the tone of the sympathetic nervous system.
In the case of a decrease in blood ejection from the ventricles, when arrhythmia is combined with heart failure, a combination of beta blockers and digitalis drugs (Digoxin, Digitoxin) is usually used. And in patients with unstable hemodynamics, they resort to intravenous administration of Amiodarone, which is an antiarrhythmic agent.
Means for continuous use
If there is an emergency decrease in heart rate, then, of course, there is also a long-term option for this type of therapy.
Most often, to slow down the heartbeat, they resort to monotherapy with beta blockers (Metoprolol, Nebivolol, Esmolol, Carvedilol), which are well tolerated by patients of any age, regardless of the presence of sinus rhythm or fibrillation.
Calcium channel blockers, which include Verapamil and Diltiazem, although they provide heart rate control and better eliminate the symptoms of the disease by increasing exercise tolerance, are still contraindicated in chronic heart failure accompanied by reduced ventricular output.
Another group of drugs prescribed for long-term use are cardiac glycosides - Digoxin and Digitoxin, which have a rather toxic effect if the dosage is incorrectly selected.
Antiari, whose analogues include Cordarone, is considered a reserve drug. Its “services” are used extremely rarely, since its action causes a lot of side effects outside the heart.
So, to summarize: to achieve the target heart rate level, which is within 110 beats/min, the choice of means is made individually, taking into account concomitant pathologies. And its prescription begins with a minimum dose, which is gradually increased until the desired effect is obtained.
Rhythm restoration (cardioversion)
In emergency situations, when the patient’s hemodynamic parameters are unstable, cardiologists have the right to decide to restore sinus rhythm. A similar tactic can be chosen with the usual consent of the patient, whose atrial fibrillation, while maintaining a normal heart rate level, is accompanied by a clear clinical picture (shortness of breath, palpitations, weakness, fainting).
Similar to the strategy described above, this treatment algorithm also has immediate and long-term measures. Cardioversion itself can be electrical or medicinal.
Emergency method
Emergency cardioversion is divided into pharmacological and electrical.
There is repeated experimental evidence of the effectiveness of antiarrhythmic drugs in returning sinus rhythm in 50% of patients with the development of paroxysm of atrial fibrillation. In this case, there is no need to carry out preparation, unlike the hardware method, that is, there is no need for fasting and prescribing sedatives. The agents used in this procedure include: Dofetilide, Flecainide, Propafenone, Amiodarone, etc.
A method has been developed that allows patients to adjust their heart rhythm on their own at home, the so-called “pill in your pocket” therapy. Flecainide and Propafenone are suitable for this purpose.
Electrical cardioversion with direct current is chosen as the main method in patients with pronounced hemodynamic disturbances in the event of a paroxysm of atrial fibrillation.
Long-term use of drugs
Long-term use of antiarrhythmic drugs is designed to reduce the number of symptoms associated with atrial fibrillation and improve the general condition of the patient. But, before choosing this tactic, the doctor assesses the severity of the disease, the risk of side effects and, of course, the opinion of the patient himself.
The main drugs used in this case are:
- "Amiodarone";
- "Dronedarone";
- "Flecainide" and "Propafenone";
- "Quinidine" and "Disopyramide";
- "Sotalol";
- "Dofetilide."
The choice of drug is made only after a comprehensive examination of the patient and taking into account the presence of concomitant pathologies. For example, Dronedarone is contraindicated in chronic heart failure.
Catheter ablation
Catheter and radiofrequency ablation (RFA), in fact, are surgical methods that isolate trigger zones in the pulmonary veins and “cauterize” arrhythmogenic areas in the left atrium, that is, areas of the myocardium capable of generating those same pathological discharges.
This method of restoring sinus rhythm is considered the most effective in patients with paroxysmal, persistent and long-term persistent fibrillation, accompanied by a severe clinical picture. I note that the procedure is resorted to only after objectively unsuccessful therapy with antiarrhythmic drugs.
Prevention of thrombosis
- administration of heparin at a dosage of 4000-5000 units intravenously;
- the use of low molecular weight heparins - flenox, clexane, cibor, fraxiparin in a dosage of 0.2-0.4 ml subcutaneously;
- after stopping an acute attack of arrhythmia, switch to warfarin 5 mg/day;
- an oral thrombin inhibitor - dabigatran (Pradaxa) - is used as an alternative to warfarin 150 mg 2 times a day.
- antiplatelet agents – acetylsalicylic acid (cardiomagnyl, aspecard 75 mg per day), clopidogrel (Plavix, trombonet 75 mg/day).
Risk factors and comorbidities
Here we come to a discussion of pathologies that can “push” the development of atrial fibrillation and increase the number of its relapses and complications. If these risk factors are identified in time and skillfully dealt with, many problems that arise during the treatment of heart rhythm disturbances can be avoided in the future.
Diseases that provoke atrial fibrillation include:
- chronic heart failure;
- arterial hypertension;
- pathology of the heart valve apparatus;
- diabetes;
- obesity;
- respiratory diseases (COPD, sleep apnea, i.e. stopping breathing, etc.);
chronic kidney disease.
How to avoid complications?
The main danger of arrhythmia is that it occurs without symptoms, the patient does not even suspect the disease, while critical changes are already observed in the body. In rare cases, even the symptoms themselves are dangerous; for example, loss of consciousness can immediately lead to death if a person is driving or on a subway platform.
But the main problem is the serious consequences that arise due to insufficiently effective treatment. How to avoid such problems? To avoid complications, you should follow all the doctor’s recommendations, as well as regularly visit a cardiologist, do an ECG, and at the first sign of an attack, urgently call an ambulance.
Arrhythmia in 90% of cases leads to serious consequences due to untimely contact with specialists or the patient’s unwillingness to comply with all prescriptions. Often a person voluntarily refuses to take medications, believing that harmless symptoms are the only thing that threatens him. Some people are careless about their health and simply forget to take medications, others do it deliberately and switch to unconventional methods of treatment, deciding not to consult with specialists.
Doctor's advice
I think there is no need to talk about lifestyle modification, which can reduce the risk of obesity, diabetes and arterial hypertension. But many people forget that, having a family history of arrhythmia, it is necessary to promptly treat all diseases of the lungs and bronchi, choose a profession wisely, avoiding work with a high content of dust in the air (for example, the mining industry). This will reduce the risk of fibrillation associated with COPD.
Clinical case
Patient A., 25 years old, was brought to the emergency department with complaints of lack of air, inability to breathe deeply, palpitations, dizziness, and severe general weakness.
The patient was engaged in semi-professional powerlifting, and during the next approach he lost consciousness. In the family, the grandmother and mother were diagnosed with atrial fibrillation. Objectively: the skin is pale, shortness of breath at rest, blood pressure is 90/60 mm Hg, heart rate on auscultation is 400 beats/min, the first tone is also heard louder than normal, the rhythm is irregular, the pulse on the radial artery is 250 beats/min. Preliminary diagnosis: “Newly diagnosed atrial fibrillation.” To confirm the diagnosis, the following were used: clinical blood and urine tests, determination of TSH levels, ECG, Echo-CG. The patient underwent pharmacological cardioversion with Dofetilide, after which sinus rhythm was restored with a heart rate in the range of 60-64 beats/min. During the hospital stay, 24-hour ECG monitoring was carried out, and no paroxysms of fibrillation were observed. The patient was advised to limit physical activity.
Goals of MA therapy
- Restoration and maintenance of sinus rhythm (in cases where appropriate)
- Prevention of subsequent episodes of atrial fibrillation
- Reducing and monitoring heart rate during persistent atrial fibrillation (for example, persistent arrhythmia) to reduce discomfort from palpitations and as a preventive measure for heart failure.
- The main direction is to recognize the reduction of the risks of thromboembolic complications and mortality from them.