The branch of medicine called gastroenterology deals with pathologies and treatment of the digestive system and its organs (gastrointestinal tract, etc.), their structure and functions. In turn, gastroenterology is divided into many areas, depending on the organs they study. For example, coloproctology studies the colon and all its parts, the anus and rectum are under the supervision of proctology, and the biliary tract, gallbladder and liver are studied by hepatology.
Like other medical fields, gastroenterology often interacts with other areas such as surgery, pediatrics, etc. The initial examination and diagnosis are usually carried out by therapists (pediatricians), and only then the patient is referred directly to a gastroenterologist (coloproctologist, hepatologist, etc.).
Patients are encouraged to go to the hospital for pain or digestive disorders, which results in the identification of gastrointestinal pathologies such as ulcers, hepatitis, various colitis, pancreatitis, inflammation of the duodenum (gastroduodenitis) or inflammatory processes of the gastric mucous membranes (gastritis), inflammation of the esophagus (esophagitis), pancreas (pancreatitis), gall bladder (cholecystitis), etc.
How the intestines work
Food processing begins in the mouth, where the salivary glands are located. The saliva they produce contains some enzymes that begin to break down carbohydrates - substances that the body considers most necessary, since they provide energy to the internal organs the fastest.
The entry of food into the mouth “presses” receptors that go directly to the glands located in the stomach and pancreas. These organs are tuned to help with digestion in the intestinal tract.
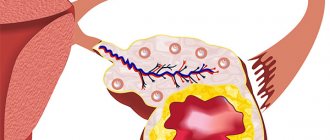
From the mouth, food enters the esophagus, and then into the stomach. There, partial disinfection of food occurs with hydrochloric acid from gastric juice. The same stomach secretion partially breaks down the proteins present in food. After this initial processing, food enters the intestinal tract: first into the duodenum, then through two more sections of the small intestine, and only then into the large intestine.
The excretory duct of the pancreas opens into the duodenum, which produces enzymes that break down proteins, fats and carbohydrates into “elementary structures”: amino acids, fatty acids and monosaccharides, respectively. The main bile duct also exits here, the bile flowing from it helps to break down fats well. Further, gradually, as it moves through the small intestine, “elementary structures” are absorbed by its mucous membrane and enter the blood and lymph.
This liquid food porridge reaches the border with the colon. There is a kind of valve that allows passage only in one direction. He does this gradually so that the appendix, which is a kind of tonsil, has time to “filter” the contents of the intestinal canal from microbes. Fiber and connective tissue processed by local bacteria are absorbed in the colon. The latter “add” vitamins to the absorbed substances, which are necessary for blood clotting and transmitting impulses from nerves to other nerves, and from them to muscles. It is in this section that bacteria process the remaining proteins in such a way that the products of such processing become the formation of toxic substances (normally they should be excreted in feces), and feces acquire that characteristic smell that is felt when going to the toilet.
The final section of the large intestine is created to form feces by absorbing water from food gruel, in which there is no longer anything nutritious left.
Belching
Belching is a sudden involuntary release of gas into the oral cavity from the stomach or esophagus (sometimes mixed with food). As the amount of gas in the stomach increases, the pressure increases, then the cardiac sphincter relaxes and the pylorus contracts at the same time.
Belching usually occurs after eating. In the etiology of belching, an important role is played primarily by aerophagia - excessive swallowing of air during meals due to overeating, fast eating, talking while eating, drinking carbonated water, smoking.
Belching can also be caused by excess food consumption, including large amounts of fresh bread, beans, peas, cabbage, and swallowing food with the mouth closed. In some diseases (pancreatitis, gastritis, peptic ulcer of the stomach and duodenum), leading to the development of fermentation and putrefaction in the stomach, so-called rotten belching occurs, accompanied by an unpleasant taste and smell.
To combat belching, you should reduce the consumption of carbonated drinks, legumes, and slowly eat small portions of food. Drug therapy should be aimed at reducing the acidity of gastric juice and strengthening the sphincter of the cardia.
Symptoms of intestinal diseases
Since different parts of the intestinal tube are responsible for different processes:
- small intestine - for the absorption of nutrients necessary for the existence of the body into the blood,
- large intestine - for the absorption of water from the “former food gruel” back into the blood, for the formation of formed feces and their timely excretion, for the production of vitamins and ensuring the processing of fiber,
then the symptoms of diseases of the large and small intestines will differ. Most often it happens that the process, which can be:
- hereditary: for example, congenital deficiency of one or another digestive enzyme;
- infectious: both in the form of poisoning, the symptoms of which are caused by the entry of microbial toxins into the gastrointestinal tract, and in the form of inflammation of the intestinal wall caused by the microbes themselves, as well as the simplest amoebae and balantidia;
- parasitic (caused by worms);
- tumor;
- neurogenic or endocrine, when intestinal symptoms are caused by dysregulation of its activity carried out by hormones and the nervous system;
- adhesive;
- chronic inflammatory: for example, Crohn's disease, Whipple's disease, ulcerative colitis,
develops simultaneously in both the large and small intestine.
How do small intestinal diseases manifest?
Diseases of the small intestine manifest themselves:
- Pain that is usually localized in the navel area.
- Liquid stool, which most often has a light color, foamy or mushy character with “inclusions” of undigested foods, especially of plant origin, and a sour, unpleasant odor.
- Feelings and sounds of “transfusion” in the abdomen.
- A feeling of bloating, heaviness, distension of the abdomen, which is slightly relieved by the act of defecation.
- The urge to defecate is imperative and cannot be tolerated.
- Inflammatory bowel diseases can be accompanied by an increase in temperature to different numbers, which depends on the number of microbes ingested, the degree of their toxicity to the body, and the resistance (immunity) of the body itself.
- With the long-term existence of such symptoms, there are signs of suffering in other organs: fatigue;
- weakness;
- weight loss;
- the skin becomes dry and thin;
- nails become thinner, brittle, and become covered with transverse striations;
- visual acuity decreases;
- jams appear in the corners of the mouth;
- the whites of the eyes turn red;
- frequent headaches;
- Dots often “float” in front of your eyes;
- Joints of different locations periodically ache and swell, in which arthritis is diagnosed.
How do colon diseases manifest?
These diseases are characterized by:
- Pain syndrome. Pain in the large intestine is usually localized along the perimeter of the abdomen: on the left side, on the right side. They can be localized above the navel or “in the pit of the stomach,” but less frequently. They are strong, dull, bursting, and make you want to go to the toilet to relieve the condition. The pain comes in waves; not related to food intake. Usually such pain increases in the evening.
- The feces are frequent, foul-smelling, and may contain: blood, mucus, pus, “stripes” resembling swamp mud.
- If the colon becomes inflamed due to infection, the body temperature rises to different levels, appetite decreases, headache and dizziness appear.
- Incontinence of gas and stool.
- Rumbling in the stomach, which, together with a feeling of bloating, increases in the evening, weakening towards the night.
Diet
Taking medication alone is not enough to treat intestinal diseases. The patient must follow a special diet that is aimed at:
- normalization of digestion;
- stimulation of restoration processes in the intestinal mucosa;
- normalizing microflora;
- replenishment of the body with nutrients;
- elimination of metabolic disorders.
Dishes should include a maximum of vitamins and beneficial microelements. The products used are well boiled, stewed or baked, but not fried. Food must be taken 5-6 times every day at regular intervals. The optimal serving size is 200-250 g. Other nutritional rules:
- do not eat dry food;
- do not overeat;
- do not eat 3-4 hours before bedtime;
- not to starve.
It is necessary to completely exclude from the diet foods that impair digestion, lead to constipation, diarrhea or flatulence. Their list includes:
- roast;
- fat;
- smoked;
- spicy;
- sweets;
- fatty broths;
- fried soups;
- bananas;
- fatty meat, fish;
- strong coffee and tea;
- muffins.
The menu should not contain products with coarse fiber: potatoes, beans, cabbage, zucchini, celery, bran, beans, nuts. If you have diarrhea, you need to pay attention to fluids. It is recommended to drink more warm water to prevent dehydration. Lemon tea, non-carbonated alkaline drinks, blueberry infusions, and apple juice are useful in this case. They are consumed on the first day of diarrhea. On the second day you can add crackers without spices and additives, on the third day you can add products that reduce intestinal motility:
- rice concoctions;
- liquid porridge;
- weak chicken broths;
- fine-grained low-fat cottage cheese;
- vegetable puree;
- jelly from berries and fruits.
For constipation, on the contrary, you need to consume more fiber, but also continue to drink plenty of fluids. Reduced portions of food eaten help to activate intestinal function in case of difficulty in defecation. For easy digestion, it should have a temperature of 38-40 degrees and be as crushed as possible. Helpful for constipation are:
- buckwheat, pearl barley, wheat and oatmeal;
- fresh vegetables;
- greenery;
- apples, plums, kiwi;
- rich vegetable soups;
- kefir, sour cream, yogurt, yogurt.
Causes of intestinal tract diseases
Diseases of any part of the intestinal tube can occur due to one of the following reasons:
- Defects or “unsuccessful combination” of genes responsible for the structure and function of the gastrointestinal tract.
- “Overactive” immunity, which, when a microorganism (amoeba, bacteria, virus, fungus) enters the intestinal tract, not only destroys it, but also damages the intestinal wall.
- Incorrect, almost monotonous diet: excessive infatuation with carbohydrates, fats or proteins, carbonated drinks or foods rich in fiber.
- Taking certain medications. “Leaders” in the field of intestinal diseases are antibiotics, which do not damage the organ wall, but change the composition of the microflora, as a result of which not only the absorption of beneficial substrates from food and the production of necessary vitamins changes, but also affects the overall human immunity.
- Sedentary lifestyle. Peristalsis, that is, contractions of the gastrointestinal tract necessary for the movement and “kneading” of food with its uniform processing by enzymes and digestive juices, also depends on human motor activity.
- Bad habits, such as smoking and drinking alcohol, leading to ischemia (that is, a lack of oxygen in the intestinal wall).
- Eating foods contaminated with microbes. The “leaders” in this area are expired dairy products, confectionery products with cream, as well as “healthy” raw eggs, uncooked meat and raw water.
- Eating food with dirty hands or from the same container as a person with an intestinal infection.
- For some viruses that cause intestinal infections, there is also an airborne route of transmission of the microbe from sick to healthy.
- Stress. This factor, influencing the regulation of the digestive system, can cause symptoms of damage to any part of it.
- Some poisons, such as those found in mushrooms, pesticide-treated plants, or liquids not intended for human consumption.
- Increased production of VIP hormone. This leads to impaired absorption of water from the intestines, resulting in frequent watery stools.
- Disruption of brain-gut interaction, which occurs through the spinal cord and fibers of the sympathetic and parasympathetic nervous system.
- Imbalance between hormones and hormone-like substances: histamine, bradykinin, serotonin, cholecystokinin-pancreozymin, which take part in the regulation of the digestive tract.
How the small intestine of the digestive system can be affected
The most common inflammation of this section is called “enteritis”. Also, this section can be “pinched” by adhesions, cancer can develop in it or its interaction with the nervous system can be disrupted. The main symptoms of these pathologies are associated with one of two conditions:
- malabsorption - impaired absorption from the intestine;
- maldigestion - a “disruption” of the ability to break down food into its main components. This process can be disrupted either in the intestinal cavity, or in the area of its villi, which absorb food, or already inside the intestinal cells.
Each of these conditions has its own cause:
- Digestive insufficiency in the intestinal cavity is associated with diseases of the glands that help break down food into its components: the pancreas, liver and gall bladder. The condition is aggravated by an unbalanced diet, when, against the background of a large amount of carbohydrates and fats taken, few vitamins are supplied to the food, psycho-emotional stress, as well as previous intestinal infections, when the composition of the microflora of the small intestine has changed significantly.
- Disturbance in the interaction of food with the intestinal villi, which must absorb it, occurs as a result of damage to these villi by various disease processes. This type of maldigestion develops with enteropathies, chronic enteritis, and Whipple's disease. We will talk about them further.
- Disturbance in the supply of nutrients inside the intestinal villi itself, where the blood vessel is located where food should flow. This happens with congenital or acquired deficiency of enzymes that break down carbohydrate disaccharides.
- Impaired absorption of food in the small intestine is associated with changes in the structure of the mucous membrane due to inflammatory and tumor processes, as well as treatment of the latter with radiation therapy. The cause is also a violation of the motor function of the intestine and dysbacteriosis. Malabsorption is also caused by diseases of the liver, pancreas, inflammation of the peritoneum, and systemic diseases that cause damage to all connective tissue present in the body. Impaired absorption of essential substances will also develop after removal of more than 1.5 meters of the small intestine.
Why this “smart” division of dysfunctions of the thin section of the digestive tube? The fact is that they are treated differently, and understanding where the “block” occurred will help to overcome it, and not take general measures.
Prevention
Gastrointestinal diseases are much easier to prevent than to treat. To do this, you need to normalize your diet and give up unhealthy foods. It is important to exclude canned food, smoked foods and carbonated drinks from the menu. In addition, you should minimize the amount of alcohol consumed.
One of the most important methods of prevention is the elimination of stress.
It is recommended to remain calm in any situation so as not to provoke the production of hydrochloric acid.
If you need to work night shifts, you should try not to adhere to such a schedule on weekends so that the body does not adapt to such a schedule. During treatment with antibiotics and non-steroidal anti-inflammatory drugs, it is necessary to additionally take medications that protect the gastric mucosa. They will help prevent organ damage during treatment.
Patients who abuse tobacco products are advised to give up their addiction.
The most common diseases of the small intestine
There are quite a lot of diseases in this part of the digestive tract. With each of them, one or more of the mechanisms described above will be disrupted: absorption or digestion in or outside the intestinal cells.
Eosinophilic enteritis
This is a disease that occurs due to the accumulation in the intestinal wall of blood cells released from the vessels that are responsible for allergies - eosinophils. The reason for it is not clear.
It manifests itself with the following symptoms:
- pain in the umbilical region of the abdomen;
- nausea, vomiting;
- diarrhea, with fecal stools that are difficult to wash off the walls of the toilet;
- food allergies;
- weight loss;
- Ascites may develop - fluid effusion into the abdominal cavity.
In this case, the examination does not reveal signs of tumor, parasitic or other diseases. Typically, relatives of such a person have food or drug allergies.
Whipple's disease
This is an infectious pathology that occurs in people with impaired cellular immunity, whose macrophage cells are unable to “digest” bacteria or bacterial antigens.
This is a rare disease that affects mainly men 40-50 years old.
The first symptoms of the disease: fever, pain in all joints without external changes, abdominal pain of uncertain localization. Then, gradually, the person loses weight, he often has diarrhea, which is accompanied by the passage of fatty, difficult-to-wash feces.
The further course of the disease “brings” extraintestinal symptoms:
- hearing and vision impairment;
- headache;
- inability to look away in any direction;
- hand trembling;
- insomnia;
- heart rhythm disturbance;
- difficulty breathing;
- desire to drink and eat a lot;
- Dementia (dementia) gradually progresses.
Small bowel cancer
It is extremely rare, occurring in 2% of all gastrointestinal cancers. Statistics say that this cancer develops 2 times more often in men. It mainly affects older people, over 60 years of age. The causes of cancer are considered:
- polyps that develop in the mucous membrane when it is frequently inflamed;
- chemical carcinogens contained in canned, genetically modified and fried foods;
- some genetic forms of intestinal polyposis;
- Crohn's disease (more on that below);
- celiac disease;
- diverticulitis;
- nonspecific ulcerative colitis (we will also talk about it briefly);
- irradiation of the abdominal cavity;
- oncological pathologies of other localizations, in which cancer cells enter the small intestine through the bloodstream;
- some genetic abnormalities (for example, Yegers syndrome).
Symptoms of cancer are associated with the fact that the tumor usually grows into the lumen of the intestine, narrowing it and preventing food from passing through this place. Sometimes the first signs are associated with the fact that the tumor “solders together” several organs (intestinal loops, bladder, colon, internal genital organs, neighboring lymph nodes or vessels), growing into them. The visible “beginning” of the disease may be tumor metastasis.
Small intestine cancer manifests itself with the following nonspecific signs:
- periodic nausea, vomiting;
- bloating;
- compressive pain in the navel area that goes away after taking No-shpa, Baralgin or similar drugs.
Subsequently, weight loss, dry skin, and blurred vision appear and increase.
If obstruction develops associated with a critical decrease in the lumen of the intestinal tube, this is manifested by severe bloating, vomiting, cessation of gas discharge, abdominal pain and dehydration. This condition requires urgent surgical intervention.
Crohn's disease
If the specific inflammation that develops with this pathology affects the wall of the small intestine, the following symptoms occur:
- pain in the navel area;
- rumbling in the stomach;
- diarrhea.
Gradually, a person experiencing such attacks loses weight, his skin becomes thinner and dry, jams appear in the corners of his mouth, nails crumble and turn yellow, and red spots appear on the skin.
Common pathologies of the large intestine
The most common diseases affecting the large intestine are:
Colon dyskinesia
It is also called “irritable colon”, “mucosal colitis”. The pathology manifests itself as periodic attacks of bloating, rumbling in the abdomen, and pain in the abdomen, usually relieved by defecation. Attacks occur after an error in diet or stress. When examining, no changes in the digestive canal are detected, since the basis of the disease is a violation of the nervous regulation of its work.
Diverticulosis
Diverticula are sac-like protrusions of the intestinal wall in the direction opposite to its lumen. They occur in people who prefer food poor in plant fibers and fiber. Most often, diverticula begin to appear only in old age or senility. Their “favorite” localization is the left sections of the intestine.
The disease does not manifest itself in anything special for a long time. Occasionally, abdominal pain and constipation may occur. The appearance of symptoms is associated with complications of diverticulosis: diverticulitis (inflammation of the protrusion), the occurrence of ulcers and suppurations in the diverticula. This is manifested by persistent abdominal pain, vomiting, weakness, fever, pain when touching the abdomen. This clinical picture suggests that surgical intervention is required.
Chronic colitis
This disease can occur after suffering from dysentery; it can be caused by worms and protozoa such as Giardia. Chronic colitis can develop as a result of chronic poisoning with salts of heavy metals, and also become a “response” to taking allergenic foods.
Symptoms are nonspecific and occur in attacks:
- stomach ache;
- bloating;
- the urge to defecate, after which the bowel movement itself does not occur;
- diarrhea, which is replaced by constipation;
- nausea;
- mucus and streaks of blood are found in the stool;
- weight loss;
- decreased appetite;
- irritability;
- insomnia;
- headache.
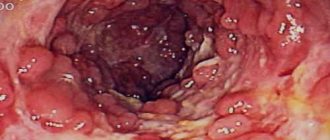
Nonspecific ulcerative colitis
This is a disease whose cause has not yet been determined. The most common theory considers bacteria to be the main “culprit” for the appearance of ulcers on the mucous membrane of the colon. It is confirmed in treatment: taking specific antibiotics can significantly improve a person’s condition.
UC appears:
- bleeding of scarlet blood from the rectum;
- periodic diarrhea;
- severe pain in the left half (maybe in the right) of the abdomen;
- decreased performance;
- weakness.
Ulcerative colitis can become a precancerous disease, as well as a cause of intestinal contents entering the abdominal cavity, so it must be “kept under control” with medication, checking the condition of the ulcers by endoscopic methods (sigmoidoscopy, colonoscopy) every 6-12 months.
Crohn's disease
With this pathology, there is the appearance of areas of inflammation in any part of the gastrointestinal tract, from the esophagus to the sigmoid colon. In this case, all the membranes of the “digestive tube” are affected.
The first symptoms of this intestinal disease:
- pain in the abdomen, usually in the right side, reminiscent of an attack of appendicitis;
- bloating;
- diarrhea;
- increased body temperature;
- rumbling in the stomach.
If the swelling of the intestinal wall is so significant that it blocks the lumen of the digestive canal, partial or complete intestinal obstruction develops, which is manifested by bloating, cessation of gas discharge, and vomiting. At first there may be stool, then it stops and becomes impossible.
When Crohn's disease persists for a long time, a person's joints often hurt and become swollen, pain begins on the right side under the rib, and red spots appear on the skin similar to an allergic rash.
Colon cancer
This disease develops quite often. Risk factors for its development are considered to be a diet rich in animal fats, flour foods and foods without fiber, alcohol intake, stress and trauma to the mucous membranes from foreign objects. The “culprit” is also the long-term existence without treatment of intestinal polyposis, ulcerative colitis, when the cells of the lining of the intestinal gastrointestinal tract, modified as a result of chronic inflammation, have to transform even more, becoming little similar to those that should be in this localization.
Signs of colon cancer are:
- constipation, especially if the tumor grows inside the intestinal canal;
- stomach ache;
- the appearance of blood in the stool, although there does not have to be a lot of it; single blood streaks are sufficient for examination;
- increase in temperature, usually to small numbers;
- weight loss;
- periodic diarrhea;
- weakness.
In the early stages, the disease is “silent”; it can only be detected if you undergo annual preventive endoscopic examinations.
Other diseases
The large intestine can become a localization for the development of such surgical diseases as:
- papillitis;
- paraproctitis;
- cryptite;
- anal fissures;
- haemorrhoids;
- rectal polyposis;
- rectal condylomatosis;
- epithelial coccygeal duct and its cyst.
Diseases that affect both intestinal sections
This includes adhesive disease, which is treated in a surgical hospital, and infectious gastroenterocolitis, which is treated by infectious disease specialists.
Adhesive disease
Adhesive disease is a pathology that is characterized by the appearance of “jumpers” between the abdominal organs. They consist of the same tissue that makes up the outer wall of the digestive canal and the peritoneum, and can lead to compression of the internal organs from the outside and a change in their localization.
Symptoms of intestinal adhesive disease are nonspecific and depend on the location of the moorings (also called adhesions): swelling and severe edema can also appear when they, like adhesions, block the lumen of the “tube” through which food moves. They are as follows:
- abdominal pain, which initially has a clear localization, then becomes diffuse;
- constipation;
- feeling of bloating;
- stopping the passage of gases;
- nausea;
- vomiting, and the vomit may have a fecal odor.
Until the passage of food through the digestive canal is disrupted, adhesive disease will practically not make itself felt. This can only occur:
- unstable stool, when constipation gives way to diarrhea,
- also abdominal pain, which is initially local in nature (localization can be indicated with a finger) and appears several hours after eating food.
Infectious gastroenterocolitis
This diagnosis is made when there are signs of an intestinal infection, but there is still no bacteriological analysis of stool, by which it would be possible to say which microbe caused the disease: is it dysentery, salmonellosis, coli infection or another.
The disease usually appears 3-24 hours after eating an expired, sour, unrefrigerated product, or a product prepared in violation of technical specifications. Most often, such foods are dairy and fermented milk products, raw eggs, products with pastry cream, salads with mayonnaise and undercooked meat. The cause may also be water drunk from an open reservoir and unboiled.
Symptoms of infectious gastroenterocolitis are:
- temperature increase;
- weakness;
- nausea and vomiting;
- cramping abdominal pain that decreases after bowel movements;
- the stool may be fecal in nature (especially at first), then “just water” may be released;
- there may be streaks of blood, mucus, “swamp mud” in the stool, the stool itself may resemble “jelly”;
- with profuse vomiting or diarrhea, dehydration quickly sets in, characterized by hoarseness, severe weakness, even fainting, decreased blood pressure, darkening of urine and a decrease in its quantity (up to complete cessation of urination);
- if the microbe that caused the process is very aggressive, then weakness, decreased blood pressure and clouding of consciousness can occur even without dehydration.
Nausea and vomiting
Nausea is a painful sensation in the epigastric region and pharynx, often preceding vomiting.
Vomiting is a reflex eruption of the contents of the stomach (sometimes the duodenum) through the mouth (possibly through the nose). Vomiting is a protective reaction of the body (except for prolonged vomiting) that helps remove toxic and irritating substances.
The act of vomiting consists of three phases: nausea, the urge to vomit, and vomiting itself.
Vomiting is regulated by two structures of the medulla oblongata: the vomiting center and the chemoreceptor trigger zone (it only triggers the act of vomiting).
There are central (nervous, irritation of the meninges), hematogenous-toxic (action of poisons, toxic substances) and visceral (reflex) vomiting (gastritis, peptic ulcer, cholecystitis). In the etiology of vomiting, gastrointestinal diseases (gastritis, ulcers, infections), intoxication, dysfunction of the vestibular apparatus, and reflex reactions—irritation of the pharynx, root of the tongue, and stomach wall—play a role.
The most dangerous localization of pain is in the right abdomen
Pain on the right side of the abdomen can accompany diseases not only of the intestines, but also of other organs. Let's try to find the cause of the pain depending on its nature:
Nagging pain
Their reasons may be:
- in women – inflammation of the uterine appendages (adnexitis, salpingoophoritis);
- right ovarian cyst;
- in men: prostatitis;
- in men and women: cystitis.
Aching pain
If they develop in pregnant women in the first two trimesters of pregnancy, they may indicate a threat of miscarriage. After 30 weeks, they “talk” about an imminent birth.
In non-pregnant women and men, this type of pain may indicate the onset of infectious enterocolitis or a functional bowel disorder caused, for example, by foods rich in fiber or fat.
Sharp pain
This type of pain indicates the need to contact a surgeon, because it may be:
- appendicitis;
- ovarian rupture;
- intestinal tumors;
- torsion of the pedicle of the right ovarian cyst;
- in men, it can also be a sign of sexually transmitted diseases, cystitis or urethritis.
Stitching pain
This character most often indicates diverticulitis or intestinal tumors.
Severe pain
They are characteristic of Crohn's disease, appendicitis, and sometimes of ulcerative colitis.
Acute pain
It is typical for an ectopic pregnancy during a rupture of the right fallopian tube in which the fetus ends up. The same word can be used to describe ovarian apoplexy and acute appendicitis.
Blunt pain
Among the many reasons, the main ones are:
- adnexitis;
- pyelonephritis;
- cysts of the uterine appendages;
- cystitis.
Cramping pain
This is how it is usually described:
- ectopic pregnancy;
- renal colic, associated, for example, with the passage of a stone through the ureter;
- appendicitis;
- biliary colic;
- in pregnant women - labor has begun.
Appetite disorders
They manifest themselves in the form of decreased appetite (hyporexia), anorexia (lack of appetite), increased appetite (hyperrexia) and pararexia (perversions of appetite - desire to eat coal, chalk, etc.).
The etiology of appetite disorders is associated with diseases of the digestive organs and endocrine system, vitamin deficiencies, infections, intoxications, encephalitis, mental disorders, anemia, and malignant tumors.
A pathological increase in appetite (bulimia, “ravenous appetite”) occurs, as a rule, when the hypothalamic centers are damaged. With bulimia, a person cannot get enough even with an excess of food.
Intestinal diseases in children
In childhood, several pathologies of the intestinal tract are most common. This:
- intestinal infection caused by rotavirus, salmonella, shigella dysentery and many other microbes;
- congenital deficiency of enzymes, most often those that break down the components of mother's milk;
- malformations of the intestinal tract, for example, Hirschsprung's disease, congenital megacolon, stenosis (obstruction) of the lumen of the intestinal tube;
- intussusception, that is, the “insertion” of one section of the intestine into another, which most often develops at the age of 1.5 months or later, requires urgent surgical intervention.
Slightly less common are diverticulitis, spastic, ulcerative and pseudomembranous colitis, polyposis of the intestinal tract, and local tumors.
Symptoms of intestinal diseases in children will depend on the cause of the disease:
- With an intestinal infection, this will include fever, vomiting, diarrhea, sometimes streaked with blood, and refusal to eat.
- Surgical pathology: intussusception, appendicitis, intestinal stenosis have rapidly increasing symptoms: the baby’s tummy swells, vomit appears, which most often has a greenish color or contains uncurdled milk or undigested food. The child initially cries, is restless, presses his legs to his stomach, but quickly becomes lethargic, indifferent, and refuses to eat or drink.
- Enzyme deficiency is manifested by profuse diarrhea in the presence of certain (usually dairy) foods; when the formula is replaced with a lactose-free one, this symptom disappears and the child begins to gain weight.
In children under 6 years of age, any complaint of abdominal pain, bloating or vomiting should prompt an immediate examination by a surgeon with an ultrasound scan of the abdominal cavity. Due to the peculiarities of the innervation of the intestinal tract at this age, the child will not be able to indicate the exact location of the pain, and even appendicitis will not have a characteristic location of pain - in the lower and right abdomen.
Parents should remember that the younger the child, the less fluid loss he needs for critical dehydration, so “stool 10 times, with a volume of 2 tablespoons” in an infant is a reason to contact a pediatrician, infectious disease specialist or pediatric surgeon on the same day.
When to see a doctor
If you experience problems with the digestive tract, it is recommended not to delay your visit to the doctor. Such diseases are treated by a gastroenterologist, but in the absence of such a specialist in the locality, the treatment is carried out by a general practitioner.
If the patient shows signs of gastrointestinal bleeding, it is necessary to immediately call an ambulance, which will take the patient to the surgical department. You should not postpone a visit to a specialist, even if there are no acute symptoms of the disease.
Treatment of intestinal diseases
In order to begin treatment, you need to find the cause of the disease. For this purpose, studies such as:
- Ultrasound of the abdominal cavity, for which you need to prepare;
- X-ray of the abdominal organs. Conducted without contrast, it only allows one to see intestinal obstruction that has arisen against the background of an adhesive, inflammatory or tumor process, but not to find out the cause. If there are no signs of obstruction, then an x-ray with contrast can be performed. This will make it possible to see a tumor, diverticula or area of inflammation.
- CT scan. A precise research method that allows you to visualize many different pathologies.
- Endoscopic examinations, which make it possible to examine the digestive tube from the inside by inserting a device into its cavity. This may be a FEGDS, when the examination is carried out up to and including the duodenum, or a colonoscopy, when an endoscope will help examine the colon. To examine the small intestine, special capsules are used that a person swallows, and they display an image of the section where they are currently located on the monitor.
- Bacteriological examination of stool: used if infectious gastroenterocolitis is suspected.
- It is possible to clarify the nature of the process, the malignancy or benignity of the tumor only with the help of histological examination. To do this, during an endoscopic examination (if there are no signs of malignancy) or separately during laparoscopy, you need to “pinch off” a piece of the formation or inflamed intestine to make a diagnosis. If a malignant process cannot be excluded, the material taken during the operation is sent for histological examination, because the risk of further potential spread of cancer cells is greater than a “pity”. The surgeon first makes sure that there are no metastases in the liver, bones, or kidneys, and acts accordingly during such an operation, removing only a section of the intestine. If metastases are visualized before the intervention, the volume of the operation is increased and chemotherapy and radiation therapy are started.
Diagnostics
Since the symptoms of different intestinal diseases are similar, you cannot diagnose yourself. When the first pathological signs appear, you should consult a doctor. Based on the examination and a series of studies, the specialist will be able to get a complete understanding of the disease, its nature and location. To make a correct diagnosis, the following methods are used:
- Flexible sigmoidoscopy. Using a special device - a sigmoidoscope, the doctor examines all parts of the intestine.
- Irrigoscopy. This is an x-ray procedure in which a contrast agent is injected into the cavity of the organ being examined. To study the small intestine, the patient is given a suspension of barium sulfate to swallow, and the large intestine is injected with a special drug through the anus.
- Upper endoscopy. This method involves the use of an endoscope that has illumination and fiber optics. This helps the specialist examine the tissues of the esophageal tube, stomach and intestines.
- Colonoscopy. This is a specialized type of endoscopy. In this case, the endoscope device is inserted through the anus and not through the mouth.
- Capsule endoscopy. This is a modern technique in which the intestines are examined using a tiny container. The patient simply swallows it. Throughout the day, the device records incoming information.