Lumbosacral osteochondrosis is a disease in which there is a gradual destruction of connective tissue in the intervertebral discs. As the pathology progresses, ligaments, intervertebral joints, and vertebral bodies undergo changes.
Sacrolumbar osteochondrosis begins to develop with the breakdown of glycoproteins. These substances are polysaccharides combined with proteins. They provide elasticity as well as firmness to the connective tissue. Gradually, cartilage and adjacent structures of the spine are involved in the pathology. This mechanism of disease progression is called degenerative-dystrophic.
Osteochondrosis of the lumbosacral zone primarily affects the intervertebral disc, which consists of a fibrous ring and a nucleus. When the disease occurs, the core substance in the disc dries out, losing its shock-absorbing properties. Gradually, the structure of the fibrous ring itself is affected: breaks and cracks appear on it.
As a result of this process, the vertebrae begin to take on a very large load, which will contribute to the formation of bone tissue in the area of greatest stress. This process is accompanied by the formation of osteophytes.
The following information about this disease will help you better understand what osteochondrosis of the lumbosacral region is and how to treat it:
- More than 50% of people after thirty years of age have at least once suffered from lower back pain, the cause of which was an exacerbation of spinal osteochondrosis.
- 80% of the population is susceptible to osteochondrosis of the lumbosacral spine , but the disease is often diagnosed in physically active middle-aged people.
- Lumbosacral osteochondrosis is a common form of this pathology, occurring in 65% of all cases. Less commonly, people are diagnosed with damage to the thoracic or cervical spine.
- The first manifestations of this disease are observed in adolescents aged 16-18 years. Every year (if left untreated) the disease will worsen its course and provoke more and more dangerous complications.
- Osteochondrosis of the sacrolumbar region occurs due to both congenital and acquired reasons .
Back pain with osteochondrosis of the lumbosacral spine can radiate to the patient’s leg, buttock or stomach, which often makes it difficult to identify the disease. Therefore, during diagnosis, you should be extremely careful to find the root cause of the pain and select the appropriate treatment therapy.
Causes and provoking factors
Before treating osteochondrosis of the lumbosacral spine, the root cause that started this degenerative process in the patient’s body should be identified. Common reasons:
- Flat feet.
- The presence of excess weight, due to which a large load is placed on the spine, making it susceptible to a number of degenerative diseases, including osteochondrosis.
- Various back injuries (injuries, bruises, history of microtraumas). This category includes spinal fractures of varying severity.
- Prolonged stay in an uncomfortable position, including prolonged sitting.
- Lifting heavy objects, loads, bags, etc.
- Regular excessive physical activity that puts pressure on your back. This is especially common among athletes.
- Wrong diet, when the body does not receive enough “feeding” that enriches the vertebrae with useful substances.
- Genetic predisposition to the disease.
- Incorrectly chosen pillow or mattress.
- The influence of severe progressive diseases of the joints, as well as body systems.
- Hypothermia.
- Lack of any physical activity.
- Improper organization of the computer workplace.
Symptoms of lumbosacral osteochondrosis
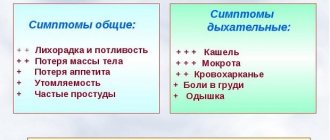
Symptoms of osteochondrosis of the lumbosacral spine depend on the degree of neglect of the disease. Characteristic signs of pathology during an exacerbation:
- aching pain in the lumbar region, which may intensify with coughing or physical activity;
- back muscle spasm;
- tingling sensation in the legs;
- shooting sensations, up to acute pain in the lower back, which are especially pronounced after hypothermia;
- weakness;
- constant chilliness of the feet;
- impaired sweating;
- gait disturbance due to severe pain can force a person to walk in a bent position.
Osteochondrosis of the sacral spine, the symptoms of which may not be felt at all for a long period, is aggravated by sudden lifting of weights or awkward movements. In this condition, signs of the disease can cause serious deterioration in a person’s condition and even deprive him of the ability to exercise for several days.
Stages
With osteochondrosis of the lumbosacral spine, a person develops an irreversible degenerative process. The disease can occur in four different degrees, each of which is accompanied by its own characteristic manifestations and disorders.
- The first degree of the disease begins with the formation of pain due to irritation of the nerve endings located in the fibrous ring. Symptoms of osteochondrosis will be periodic, occurring after physical activity. Such patients suffer from acute lower back pain (lumbodynia). At the first stage of its course, lumbosacral osteochondrosis, the treatment of which will be the simplest, provokes circulatory disorders. The disease can give impetus to the development of pathologies of the lower extremities (atherosclerosis). Urinary incontinence is less common.
- Osteochondrosis of the 2nd degree of the lumbosacral region is accompanied by an increase in the mobility of the vertebrae, which provokes persistent muscle spasm. The person suffers from pain, discomfort and impairment of physical activity.
- In the third degree, lumbosacral osteochondrosis, the treatment of which must be comprehensive, leads to loss of fragments of the affected disc and the development of radicular syndromes. In this condition, people may experience loss of sensitivity due to a pinched nerve, and there is a risk of muscle atrophy and even partial paralysis.
Characteristic complications of the third stage of the disease are dysfunctions of the pelvic organs (reproductive system, bladder, kidneys).
The last stage in which large osteophytes are formed.
Osteochondrosis of the lumbosacral spine leads to disc fibrosis. This condition may be accompanied by a temporary disappearance of pain and even restoration of a person’s activity, but the patient’s well-being may sharply deteriorate to the point of being critical. Medical treatment with drugs will no longer be effective enough. The patient is prescribed surgery.
Expert advice
If you notice the first signs of discomfort in the lower back when lifting something heavy or simply during active movements and twisting, do not delay diagnosis.
The sooner you start treatment, the easier it will be to cope with the disease and avoid unpleasant health consequences.
Many people are accustomed to taking lumbar osteochondrosis for granted. But this disease can progress, which will ultimately bring many untidy consequences to the patient. Remember that you yourself are responsible for your health, not doctors, and if you find signs of osteochondrosis, start treatment as quickly as possible.
Diagnostics
Lumbosacral osteochondrosis, the symptoms of which develop suddenly, requires careful diagnosis. To do this, a person needs to visit a neurologist and undergo the following tests:
- X-ray in two different projections. The study will allow you to see the structure and shape of the vertebrae, their anomalies. Using X-rays, the doctor identifies bone formations (osteophytes), narrowing of the joint space, and salt deposits. This study is mandatory when diagnosing osteochondrosis.
- CT. This informative, painless procedure will allow you to see in detail the structure of the spine and determine the extent of its damage. With the help of a CT scan, the doctor will be able to understand how advanced the disease is and whether the person has complications.
- MRI is a study using an electromagnetic field that will allow you to see all the structures of the spine and intervertebral discs. The study will also provide information about compression of nerves and the presence of a hernia.
Computer tomogram.
If necessary (to clarify or differentiate the diagnosis), a person may require examination and consultation with a urologist, gynecologist (for women), surgeon, or rheumatologist.
Methods of treating lumbosacral osteochondrosis
Osteochondrosis of the lumbosacral spine, the symptoms and treatment of which are determined by the degree of neglect of the pathology, has a wave-like course with periods of remission and exacerbation.
Traditional therapy for this disease is complex. It provides for a course of drug treatment and surgery (if necessary). Physiotherapy, folk remedies, therapeutic massage, reflexology and exercise therapy are used as auxiliary methods.
Drug treatment
Drug therapy is prescribed immediately after the disease is diagnosed. It is also carried out during periods of exacerbation of pathology.
Painkillers and various anti-inflammatory drugs (Diclofenac, Ibuprofen, Nimesulide) are prescribed in the form of injections or local preparations. In case of severe pain, novocaine blockades with analgesics are carried out to relieve pain and relieve muscle spasms for several weeks.
In cases of severe inflammation, hormonal agents (Prednisolone, Betamethasone) and B vitamins are used. Sedatives and anticonvulsants can be used to eliminate unpleasant symptoms. Chondroprotectors (Structum, Chondroitin) are very effective, promoting the restoration of cartilage tissue.
Surgical treatment
Osteochondrosis of the sacrolumbar region, the symptoms of which are most pronounced during exacerbation of the disease, is treated surgically only in extreme cases. Direct indications for surgery:
- lack of effect from drug therapy, severe pain;
- compression of the spinal cord, which leads to weakness and paralysis;
- cauda equina syndrome.
Both endoscopic and open surgical treatment are actively practiced. The prognosis after these operations is comforting. The recovery period will be several months, after rehabilitation the person will be able to be physically active again.
Traditional therapy
Folk remedies will help stop the inflammatory process, improve back mobility and relieve pain. The following recipes are used:
- Grate raw potatoes and mix with honey. Apply to the sore area of the back. Secure with a bandage and leave for two hours. You can practice treatment with boiled warm potatoes, which should also be applied to the back.
- Mix lingonberries and mint with a spoon. Pour a glass of boiling water. Infuse, strain, drink throughout the day.
- Mix grated garlic and ginger in equal proportions. Add olive oil. Use to rub your back at night. A similar mixture can be prepared from honey and red pepper: it will help improve blood circulation and relieve muscle spasms.
- Take a spoonful of menthol and fir oils. Use for back rubs.
Treatment with folk remedies can only be carried out after prior consultation with your doctor. Practicing therapy without the supervision of a specialist can be dangerous. Such remedies only relieve discomfort and eliminate inflammation, but they are not able to completely get rid of the disease.
Symptoms of lumbosacral osteochondrosis in women can be similar to menstrual pain, so often with pain in the sacral area, women turn not to a neurologist, but to a gynecologist, which is a mistake.
What is accompanied by and how is lumbar osteochondrosis diagnosed?
It is possible to select an effective treatment method for this pathology only by knowing exactly each cause of its occurrence, as well as having an idea of how damaged the tissue is. You can diagnose lumbar osteochondrosis by examining the patient, collecting anamnesis data on symptoms, and also using instrumental diagnostics.
The signs of lumbar osteochondrosis are as follows:
- pain from pathology in the lower back, leg, and buttock;
- problems with sensitivity - its loss or, conversely, increase;
- stiffness in leg movement;
- problems with the functioning of the pelvic organs.
As the disease progresses, its symptoms also increase. They are a reason for the doctor to suspect lumbar osteochondrosis. For a final diagnosis, it is necessary to examine the patient and do several studies.
A doctor who knows his business in such cases always checks to see if there are a number of reflexes characteristic of this pathology.
Checking for the Lages reflex, the doctor straightens the patient's leg and at the same time lifts it. If the reflex is present, the pain becomes stronger, going away immediately after bending the leg.
With the ankylosing spondylitis reflex, straightening the knees and pressing them against a flat surface, such as a wall, causes pain.
It is possible to determine whether there is osteochondrosis in the human body using MRI, X-ray and CT
Using special equipment, you can obtain additional information about the current state of the spinal cord and nerve roots near the area of inflammation. In most cases, X-rays and MRIs are taken, and CT scans are used less frequently.
Having found out that this pathology is precisely osteochondrosis of the lumbar spinal column, the doctor decides on the actual method of its treatment. Many of these same techniques have been developed, from drug treatment to surgery. Massage and reflexology are often used with great success.
Preventive recommendations
Doctors say that it is easier to prevent the development of osteochondrosis of the lumbosacral spine than to deal with its long-term treatment later. A person should take the following preventive measures at home:
- Properly organize your workspace at the computer. The table should be no more than 70 cm in height. The chair should be selected with an orthopedic supporting back, equipped with comfortable armrests. It is important that the keyboard is positioned below your elbows.
- While working at the computer, take frequent breaks to stretch your back . During such pauses, it is worth performing gymnastic exercises, squats, and bends. This will relieve muscle tension and improve blood circulation.
- Organize a proper sleep schedule . This means choosing your mattress and pillow wisely. They must be orthopedic and of high quality. You need a mattress with a medium degree of hardness that preserves the natural curves of the spine during sleep.
It is advisable to have a rectangular pillow of small height.
- Give up habits that affect the body with toxic substances, which exposes it to degenerative diseases.
- Stick to a healthy diet. For prevention purposes, you need to completely exclude salty dishes, white bread, sweets, and fatty foods from the menu. Fermented milk products, vegetables, fruits, herbs, and nuts are good for bones. Oily fish and boiled meat should be regularly included in the menu.
- Avoid hypothermia.
- Avoid heavy lifting and excessive physical activity, which can damage the spine.
- Regularly engage in healthy sports. Swimming, long walks, and gymnastics are suitable. They help maintain muscle tone and improve blood circulation.
If lumbosacral osteochondrosis is being treated, active physical activity is contraindicated for the patient: running, jumping, heavy training in the gym. Such loads can only worsen the patient’s well-being and provoke another attack of pain due to a pinched nerve.
Prevention
Exacerbation of lumbar osteochondrosis can be prevented if you follow several rules:
- Do morning exercises every day.
- Avoid drafts and body hypothermia.
- Don't gain excess weight.
- Sleep on an orthopedic mattress.
- Eat more foods rich in calcium, minerals and vitamins.
- Avoid stressful situations, do not be nervous.
- Do not lift heavy objects, avoid sudden movements.
- Swim more often, walk more.
- Don't slouch, always keep your back straight if possible.
- Avoid high-heeled shoes.
- Avoid heavy physical activity.
Periodically you need to visit a doctor and undergo the necessary examinations . Early detection of spinal pathologies will help avoid severe complications and long-term treatment.
Exacerbation of lumbar osteochondrosis is accompanied by severe pain and inflammatory processes in the spine. Tissues, vertebrae, nerves and intervertebral discs are affected. To avoid complications, the disease must be treated. For this, various medications, massages, folk remedies, acupuncture, and physiotherapy are used. The exacerbation of the disease can be prevented if preventive measures are followed.
What will happen if left untreated?
Without timely treatment, osteochondrosis will gradually progress, causing dangerous complications. In this condition, the patient may develop the following consequences of the pathology:
| Complication | Peculiarities |
| Protrusion of intervertebral discs | This is the primary manifestation of an intervertebral hernia with protrusion of the disc beyond the vertebrae, which provokes irritation of the nerves and severe pain. Numbness of the legs, difficulty urinating, foot pain and tingling may develop |
| Neuralgic disorders | Manifest in the form of severe pain, shooting sensations in the back, impaired mobility, stiffness |
| Arthrosis of the spine | This disease is a consequence of degenerative changes in cartilage. It will lead to their gradual destruction |
The disease can cause lameness, migraines, arterial stenosis, and spondylosis. Often patients completely lose their ability to work and become disabled.
Lumbosacral osteochondrosis, whose ICD 10 code is designated M42, can provoke the so-called cauda equina syndrome. This condition will be accompanied by severe neurological disorders and pain in the sacral area.
Medicines
For the treatment of lumbar osteochondrosis, approximately the same medications are used as for other parts of the spinal column. This is due to the same nature of the pathology.
Classification of drugs according to the principle of action:
- analgesics to relieve the patient of acute pain;
- non-steroidal anti-inflammatory drugs to relieve swelling and inflammation;
- muscle relaxants to combat muscle spasms;
- glucocorticoid hormonal drugs, but only in cases where other drugs are useless;
- chondroprotectors, so that the necessary nutrition is better supplied to the cartilage;
- those medications that improve microcirculation, which speeds up local metabolism;
- vitamins and minerals to improve the functioning of the nervous system, as well as the general condition of the patient.
To get rid of exacerbation of osteochondrosis, take drugs of various groups
Performing exercise therapy
Therapeutic exercise for osteochondrosis of the lumbosacral region is recommended for almost all patients who have no contraindications to such exercises. This is justified by the following advantages and effectiveness of these trainings:
- pain relief for lumbosacral osteochondrosis;
- relieving muscle tension and spasm;
- improved blood circulation;
- strengthening the muscle corset;
- strengthening ligaments;
- effective fight against radicular syndrome;
- increased mobility of the spine.
Set of exercises:
- Stand straight, place your feet shoulder-width apart. Place your hands on your hips. Perform circular movements with the pelvis in one direction and then in the other. Repeat ten times.
- Get on all fours, stretch your arms forward. Lunge back, stretch out as much as possible. Repeat twenty times.
- Lie on your back, bend your knees. Raise your pelvis off the floor, arching your back. Repeat ten times.
- Lying on your side, raise your head and hold it for five seconds.
- Standing, bend over, reach your hands to the floor. This may be difficult to do at first, but with frequent practice the person will be able to place the entire palm of the hand on the floor.
- Lie on your back. Press your head onto the hard pillow, rise, but offer resistance with your hands. This will train your back muscles.
To achieve noticeable improvements, you need to practice such physical activity daily for twenty minutes.
A set of exercises will help not only cure, but also prevent the development of intervertebral osteochondrosis of the lumbosacral spine. Reviews about the effectiveness of physical activity for disease prevention can be read on numerous patient forums.
It is contraindicated to perform exercises for osteochondrosis of the lumbosacral region, acute back pain, high temperature, elevated blood pressure, or recent surgical interventions. Pregnant women, the elderly, and patients with severe diseases of the joints, liver, kidneys and heart should practice treatment with exercise therapy only with caution and only after permission from a doctor.