Skin cancer is a malignant disease of the skin. This form of the tumor process is considered one of the most common in the world. Until now, specialists in the field of oncology have not established the exact causes of the pathological focus. Like many other oncological neoplasms, skin cancer is a multi-etiological disease. There are predisposing factors and precancerous diseases, the presence of which increases the possibility of developing a skin tumor process. Depending on the stage and type of cancer, appropriate treatment is selected. You can suspect the presence of skin cancer yourself by examining the skin, paying special attention to nevi. The prognosis for life and disease when a tumor of the skin surface is detected also depends on the form and stage of the process. In accordance with the international classification of diseases (ICD-10), skin cancer is coded C43-C44.
Causes of skin cancer
There are several main causes of skin cancer:
- Prolonged exposure to ultraviolet radiation on unprotected skin. This could be intense tanning or frequent visits to the solarium. When exposed to UV rays, cell DNA is damaged. In this case, mutations arise that activate oncogenes and “turn off” genes that suppress tumors. For example, in squamous cell carcinoma, the activity of the TP53 suppressor gene, which causes the death of cells with damaged DNA, is often suppressed. Basal cell carcinoma often has a mutation in the PTCH1 gene, which controls cell proliferation.
- Exposure to ionizing radiation. This may be work involving x-ray radiation or open radiation sources. A history of radiation therapy also increases the risk of developing skin cancer.
- Immunodeficiency conditions, both congenital and acquired (HIV, organ transplantation, the need for cytostatic therapy, etc.).
- Chronic trauma to the skin, for example, rubbing from shoes or clothing.
- Contact with chemical carcinogens - soot, coal dust, paraffin, tar, household chemicals, etc.
- Infection with human papillomavirus of high oncogenic risk.
- The presence of precancerous skin diseases - leukoplakia, cutaneous horn, xeroderma pigmentosum, etc.
Why do they occur?
The study of skin tumors is still ongoing. The exact reasons for their occurrence have not been established, but scientists put forward several theories about this.
Provoking factors may be:
- family history (presence of neoplasms in relatives);
- individual characteristics of a person (light skin and hair, old age);
- exposure to ultraviolet, radiation and x-ray radiation;
- viral infection;
- long-term trauma to the skin;
- chronic exposure of the skin to chemical carcinogens (nitrosoamines, benzopyrene, aromatic amines, etc.);
- insect bites;
- metastatic processes in the presence of an oncological process in the body;
- violation of the trophism of the skin, hence chronic skin ulcers;
- weakened immune system (due to immunosuppressive therapy, HIV infection, etc.).
What is the cause of basal cell carcinoma?
Most often, basalioma is provoked by prolonged ultraviolet radiation, so most often it occurs on open areas of the skin. In addition, the development of basal cell carcinoma is facilitated by chemical carcinogens, ionizing radiation, immunosuppression, exposure to retroviruses, and genetic predisposition.
Basalioma occurs in both men and women in approximately equal proportions. People over 50 years of age are especially susceptible to it. The majority of blonde patients with fair skin and blue eyes automatically fall into the risk group. According to numerous studies, basal cell carcinoma is more common in the southern regions among fair-skinned and blue-eyed residents.
Treatment of basal cell carcinoma should be started as soon as possible, since in advanced cases the disease is more difficult to treat.
The choice of treatment for basal cell carcinoma depends on the clinical form, size and location of the tumor, the patient’s age, and concomitant diseases. Modern methods of treating basal cell carcinoma include:
- radiation therapy;
- photodynamic therapy;
- cryotherapy;
- laser therapy;
- radio wave therapy;
- drug treatment.
All of them are aimed at the destruction of the pathological focus. However, the most radical treatment for basal cell skin cancer remains surgical excision.
Get a treatment program
Is it possible to prevent the development of basal cell carcinoma?
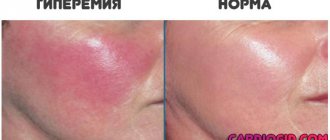
The best way to reduce the risk of basal cell carcinoma is to avoid exposure to sunlight and strictly observe personal hygiene measures when working with substances that contain carcinogens. People at risk must undergo regular self-examinations: long-term redness on the skin and non-healing wounds can be an alarming sign. Therefore, if such lesions appear, it is necessary to contact an oncologist.
Squamous cell skin cancer
Squamous cell skin cancer is the most malignant epithelial tumor. Squamous cell skin cancer accounts for about 20% of all malignant skin tumors.
In almost every case, squamous cell carcinoma develops against the background of altered skin (precancerous skin diseases, psoriasis, trophic ulcers, scars, etc.). It most often develops after 50 years of age (with the exception of cases of the disease in persons in a state of immunosuppression, here development can be observed much earlier). Excessive sun exposure plays an important role in the development of squamous cell skin cancer—the greater the total amount of sun exposure over a lifetime, the higher the likelihood of developing skin cancer. Other environmental factors are ionizing radiation, HPV-16 and 18 types, and chemical carcinogens.
Diagnosis of squamous cell skin cancer
The diagnosis of squamous cell skin cancer is established on the basis of clinical and laboratory data with mandatory morphological examination (cytological and histological). Histological diagnosis has its own difficulties in the early stages of development of squamous cell carcinoma and in the case of an undifferentiated variant. It is necessary to carry out differential diagnosis with various diseases. But histological examination is crucial when diagnosing squamous cell skin cancer.
Get a treatment program
What problems does an oncodermatologist solve during a consultation?
You should come to an appointment with an oncodermatologist at the first suspicion of the development of oncology. The doctor assesses the likelihood of malignant degeneration of benign formations. At the initial appointment, the doctor collects anamnesis, examines and palpates the lymph nodes. It is important to talk about the accompanying symptoms (burning, pain, itching). Using electronic mapping, a “map” of all the moles on the body is created, so you can track their changes in the future. If oncology is diagnosed, adequate treatment is prescribed.
Treatment of squamous cell skin cancer
The choice of treatment method depends on the stage of the disease (presence/absence of metastases), localization, extent of the primary process, the patient’s age and general condition (presence/absence of concomitant diseases). Typically, the following treatments are used for squamous cell skin cancer:
Surgical - based on excision of the primary tumor within healthy tissue, 1 cm away from the edge of the tumor, followed by plastic surgery or without it. In case of metastases to regional lymph nodes, an operation is performed to remove the affected collector (lymphodissection of the corresponding lymphatic collector).
Radiation therapy is most often used in the treatment of elderly patients, as well as when the primary lesion is large (especially in the scalp or face), when it is impossible to perform adequate surgical treatment with plastic surgery of the defect. It is possible to combine cryotherapy with radiation therapy. Typically, the first stage involves freezing the patient with liquid nitrogen (cryotherapy), then the patient is sent to radiation therapy.
Drug treatment - usually for squamous cell skin cancer is used in cases of large inoperable tumors, metastatic tumors when other treatment methods are not possible. The drugs of choice may be: platinum drugs (cisplatin, carboplatin), taxanes (paclitaxel, docetaxel), bleomycin, methotrexate, fluorouracil.
Prevention of squamous cell skin cancer involves the timely detection and treatment of precancerous skin diseases.
Skin cancer stages
There are five main stages of non-melanoma skin cancer:
- Stage 0 - “cancer in situ.” At this initial stage, cancer of the scalp, face, neck and other areas of the body is located within the top layer of the skin - the epidermis.
- Stage I - the tumor is no more than 2 cm in diameter and has one high-risk feature.
- Stage II is a tumor larger than 2 cm in diameter or having 2 high-risk features.
- Stage III - cancer cells have spread to the jaw, eye socket, skull bones, and lymph node (its diameter does not exceed 3 cm).
- Stage IV - cancer cells have spread to the skull, spine, ribs, lymph nodes, or distant metastases have been detected.
Benign neoplasms
New growths on the skin, classified as benign, as can be seen in the photo and their description, are not prone to rapid growth, metastasis and relapse after removal.
Differences between benign and malignant moles.
These tumors include:
- atheroma;
- hemangioma;
- lymphangioma;
- warts;
- moles (nevi);
- fibromas, etc.
The structure of a lipoma (benign tumor, popularly called a wen)
| View | Description |
| Atheroma | Damage to the sebaceous gland in the form of a cystic growth. Location: face. A raised formation, indistinguishable from normal skin in color, is tightly fused to it at one point. The contours are clear. Palpation of the atheroma is painless. |
| Hemangioma | Neoplasm of vascular origin, refers to childhood tumors. It can be either an independent disease or a manifestation of another pathology. The course depends on the patient’s age, location, size and depth to which the hemangioma has grown. Frequent locations are the head, face, neck, but other locations are also possible. The first manifestation is a red nodule (papule) up to 5 mm in diameter. Complaints include bleeding when accidentally touched, and sometimes dysfunction of the organ where the tumor is located. |
| Lymphangioma | There are two possible development options - a congenital defect or consequences of impaired lymph flow. The tumor can be located anywhere, but more often it is the oral cavity, neck, and upper limbs. Capillary lymphangiomas are multiple blisters with a yellowish transparent liquid inside. The same tumors that arose as a result of impaired lymph circulation look like plaques or spots, the diameter of which slowly increases. |
| Lipoma | Tumor of adipose tissue. More often they have a nodular shape. The course is asymptomatic. It is a painless pale pink neoplasm on a stalk. The consistency is doughy. The boundaries are unclear. |
| Seborrheic warts | Also called "senile". They arise as a result of impaired differentiation of cells in the basal layer of the epidermis. Appearance: Nodules or plaques raised above the skin. The surface is lumpy. The shape is often round or oval. The color of the wart varies from yellow-brown to black. |
| Moles | Or nevi. They are a developmental defect and consist of unchanged melanocytes. The characteristic color of the rash is from light brown to black, which is associated with different amounts of melanin (dark pigment) in the cells. More often, moles have a smooth surface and sometimes rise above the skin. |
| Fibroma | Fibroma is a tumor that forms from connective tissue. Dense to the touch. Reaches large sizes. Malignancy (transition to a malignant formation) of the tumor is possible. |
Neoplasms on the skin (photos and descriptions are presented above) of a benign nature, despite their relatively safe nature, can sometimes still develop into precancrosis and even cancer.
Skin Cancer Symptoms
How skin cancer manifests itself and how quickly it develops will depend on the histological appearance of the tumor.
The most common type is basal cell carcinoma. It develops extremely slowly and very rarely metastasizes, which is why it is also called a semi-malignant tumor. It can be presented as a nodular-ulcerative, superficial and morphea-like form.
The initial stage of basal cell carcinoma appears as a nodule that rises above the surface of the skin. Over time, an ulcer covered with crusts forms on its surface. If it is removed, the bottom of the ulcer is revealed, covered with red-brown tubercles.
The superficial form of basal cell carcinoma first appears as a spot or plaque, which may resemble psoriasis. Then small waxy nodules begin to form along its edges.
The first sign of squamous cell skin cancer is a papule or crusty lump. It very quickly begins to ulcerate and increase in size. Squamous cell carcinoma can be of two types:
- Exophytic - the tumor looks like a large node or mushroom-shaped formation located on a broad base. It is covered with crusts and easily begins to bleed under mechanical stress.
- Infiltrating - the tumor has the appearance of an ulcer, with crater-shaped edges. The ulcer grows quickly and invades the tissue.
Melanoma
It is diagnosed in 2.5-10% of patients and has a high probability of a malignant course and leads to death in 89% of cases. It is characterized by rapid progression and rapid transition from stages 1 to 4 of development.
This neoplasm develops from melanocytes - pigment cells of the skin. Women are more susceptible to the disease, especially after 50 years of age (at this age the risk increases sharply for all people). Most often, a tumor in women develops on the lower extremities, mainly on the lower leg; in men - on the torso, especially on the back. In older patients (65 years and older), melanoma in the head and neck area is quite common.
It is one of the most aggressive types of oncology. The human immune system reacts poorly to melanoma, which is why the tumor develops quickly - weeks, and in some cases days, pass from the initial stage to life-threatening.
The disease also quickly metastasizes, with metastases penetrating both adjacent skin and distant organs and lymph nodes. The patient can be completely cured only at the first stage, after which the prognosis is unfavorable. The neoplasm tends to grow into other tissues.
Melanoma looks like an uneven spot several millimeters wide (in later stages - up to several centimeters), which protrudes slightly above the skin surface. At an early stage, it can be identified by pain and bleeding. As for color, it is usually black, dark blue, rarely red or white. Ulcerations are quite common.
It is noteworthy that melanoma can form from age spots and on clean skin as a result of injury, intense tanning, contact with carcinogens, burns or frostbite, self-treatment and removal of nevi, and hormonal imbalances.
Also of great importance is genetic predisposition, endogenous constitutional characteristics and the nature of pigmentation, such as the color of the skin, hair and eyes, the presence of freckles on the face, hands, body, the number, size and shape of moles on different parts of the body, skin reaction to ultraviolet rays.
First of all, malignancy is characteristic of dysplastic nevi. They are larger than normal moles. In some cases, there may be many nevi on the body. Other types of nevi rarely become cancerous. However, with multiple formations or with very large moles, the likelihood of melanoma is also increased.
When do you urgently need to see a doctor for melanoma?
There are criteria (ABCDE), thanks to which patients can independently suspect a problem and consult a doctor:
- A (asymmetry) – asymmetry .
The mole grows unevenly to the side. Normally, if you draw an imaginary line through the middle of the mole, the halves will be symmetrical. - B (border irregularity) - an uneven edge. It may be jagged, indistinct, and this may suggest melanoma. Normally, a mole has smooth edges.
- C (color) – color. You should be wary of uneven color, inclusions of black, red, bluish dots or areas. Normally, a mole is one color.
- D (diameter) – diameter. If the mole is more than 6 mm in diameter, consult a specialist.
- E (evolving) - variability of any characteristic: color, shape, size - all this is a reason for an early consultation with a dermato-oncologist. Normally, moles do not change over the course of life.
What to do if a mole is located in an inconvenient place?
If the mole is located in places where it is subject to friction or traumatized - by a chain on the neck, elastic bands and underwear straps, on the head when combing - it is recommended to remove it. Any injury, including incomplete removal, can trigger degeneration into melanoma.
Diagnosis of skin cancer
During the initial appointment, the dermato-oncologist asks the patient about complaints, when the skin tumor appeared, and how its appearance has changed over time.
Then an external examination of the skin is performed. The doctor uses a special device - a dermatoscope - to examine the skin under magnification, this helps to identify changes that are invisible to the naked eye. The European Oncology Clinic uses even more advanced equipment - PhotoFinder. Using it, you can create a “map of moles”, detect skin cancer, moles that have undergone malignant transformation, and other pathological changes, and track them over time.
If, based on the results of the examination, there is a suspicion of cancer, a biopsy is performed. The doctor prescribes an operation during which he completely excises the tumor and sends it to the laboratory for cytological and histological examination.
If there is a suspicion that the lymph nodes may be affected, they are also examined. A sentinel lymph node biopsy may be performed . During this procedure, the doctor removes the lymph node closest to the tumor and sends it to the laboratory. If cancer cells are found in it, this indicates that they have probably managed to spread to other regional lymph nodes.
To search for distant metastases, computed tomography, MRI, and PET scanning will be used.
Diet
Often with skin cancer, patients suffer from exhaustion of the body. If the patient has protein-energy deficiency, the number of calories in the diet should be 3200-3500 kcal per day. If body weight does not decrease, 2100-2400 kcal is required.
It is important that the food contains useful microelements - it is recommended to add foods containing potassium to the patient's diet - bananas, dried fruits, legumes, cabbage, zucchini, pumpkin.
Squirrels
The recommended content of this component in the diet depends on the level of its deficiency in the patient’s body and existing disorders. If there is no deficiency, 90 g per day is sufficient. For protein deficiency – 140 g.
If the patient develops liver or kidney failure, this component in the diet should not exceed 60 g per day. The diet should include animal proteins (meat, fish, eggs, milk) and plant proteins (lentils, beans, cereals).
Fats
At least a third of the total amount (90 g per day) should be animal fats. In case of protein-energy deficiency, the amount of fat in the patient’s diet should be 120 g per day. Lean meats and poultry, fish, oils and dairy products are shown.
Carbohydrates
If you have skin cancer, you should reduce the amount of sugar, jam and syrups in your diet. It is useful to eat vegetables, fruits and cereals, which contain microelements and vitamins important for the body, as well as fiber. You can diversify your diet by adding bran to your diet.
Special food
Specialized nutrition for cancer patients has long been common abroad, but in Russia less than half of patients know about its existence. Created for people who have nutritional problems due to the detection of a malignant neoplasm and its treatment.
These products contain a large number of calories, protein and other substances beneficial to the body. The advantage of this food: it does not need to be consumed in large quantities: a small portion will saturate the body with the necessary amount of energy.
Sample menu for 7 days
The first day:
- 1st meal: fresh apricot juice.
- 2nd meal: barley porridge, dried bananas, tea with oregano.
- 3rd meal: soup with barley; cherry and cucumber salad with sour cream and parsley; boiled halibut and lentils; green tea.
- 4th meal: durum wheat pasta with cheese, fireweed tea.
- 5th meal: apple, kefir, dried peaches.
Second day:
- 1st meal: soy cheese, green tea.
- 2nd meal: millet porridge, dried melon, tea with chamomile.
- 3rd meal: onion soup; carrot and cabbage salad; boiled turkey; baked potatoes with parsley; green tea.
- 4th meal: seaweed salad with cranberries; steamed salmon; chamomile tea with mint.
- 5th meal: kefir, banana.
Day three:
- 1st meal: sea buckthorn, yogurt.
- 2nd meal: corn porridge, fireweed tea.
- 3rd meal: cabbage soup; cherry and cucumber salad with flaxseed oil; boiled hake; pearl barley; green tea.
- 4th meal: boiled beans; tea with mint.
- 5th meal: cottage cheese, dried mango.
Day four:
- 1st meal: fresh beetroot-pumpkin juice.
- 2nd meal: persimmon; tea with linden.
- 3rd meal: pumpkin soup; grated carrots; stewed broccoli with halibut; green tea with mint.
- 4th meal: vegetable stew; boiled hake; carrot and cabbage salad with dill, fireweed tea.
- Meal 5: yogurt, dried pineapples.
Day five:
- 1st meal: peach juice.
- 2nd meal: barley porridge, tea with immortelle.
- 3rd meal: soup with tomatoes, grated beets with hard cheese; boiled turkey meat; green tea.
- 4th meal: boiled seafood, Chinese cabbage and carrot salad, mint tea.
- 5th meal: kefir, apple.
Day six:
- 1st meal: carrot juice.
- 2nd meal: millet porridge, apricot.
- 3rd meal: fish soup, salad with radish, kohlrabi and parsley; boiled halibut, tea with chamomile and lemon balm.
- 4th meal: pea porridge, green tea.
- 5th meal: banana, lemon balm tea.
Day seven:
- 1st meal: beetroot-celery juice.
- 2nd meal: physalis, tea with chamomile.
- 3rd meal: soup with buckwheat, arugula and kohlrabi salad, boiled turkey, lentils, green tea.
- 4th meal: pearl barley, dried pears, fireweed tea.
- 5th meal: cookies, kefir.
General recommendations
Doctors advise patients with skin cancer:
- Eat often (5 times a day) and in small portions.
- When choosing drinks, opt for water, fresh fruit and vegetable juices, green tea without sugar, and herbal infusions.
- Limit salt intake - a large amount of it contributes to the accumulation of fluid in the body, which is harmful for this disease.
Prohibited Products
It is necessary to remove from the diet:
- alcohol;
- chocolate, cocoa;
- coffee, black tea and strong green tea;
- salted, smoked, canned and pickled foods;
- products with artificial colors and additives;
- sweets.
Preventing skin cancer
It is impossible to protect yourself 100% from skin cancer. But there are measures that will help significantly reduce the risks:
- If you have to be outside in sunny weather, try to be in the shade.
- Wear clothes with long sleeves and long legs.
- Use sunscreen.
- When going outside, wear a hat, preferably with a wide brim, to protect your face.
- Wear sunglasses.
- Stop smoking and other bad habits.
- Avoid visiting solariums.
- Carry out a skin self-examination regularly—either yourself using a mirror, or ask someone close to you to examine your body. If you notice any suspicious changes, it is better to immediately consult a doctor.
| Read more about dermatological research at the European Clinic | |
| Consultation with a dermatologist-oncologist | from 5100 rub. |
| Skin examination using the German FotoFinder device | 12100 rub. |
| Diagnosis of melanoma | from 5100 rub. |
Book a consultation 24 hours a day
+7+7+78