Description
Ichthyosis is a skin disease in which the process of keratinization of the epidermis in a person is disrupted, as a result of which hard scales appear on it.
At the same time, pathologically altered keratin accumulates in the skin of patients. The disease gets its name from the Greek “ichthyo”, which means fish. This is due to the fact that the skin of patients is similar to fish scales.
Ichthyosis is inherited. In more rare cases, a person may develop acquired ichthyosis. The disease is not a consequence of infection, which means that you cannot become infected with it.
The first signs of ichthyosis in patients appear in childhood, and sometimes even immediately after birth.
If the disease is caused by genetic disorders, then patients, as a rule, have disturbances in thermoregulation and have a slow metabolism. Due to the fact that patients have an increased level of enzymes in the body during oxidative reactions, their skin respiration increases significantly. People suffering from hereditary ichthyosis often suffer from diseases of the thyroid gland, reproductive organs, and adrenal glands. They often have a deficiency of immunity (cellular and humoral together).
In these patients, the functioning of the sweat glands is almost always impaired, which, in combination with a deficiency of vitamin A, can lead to increased keratinization of the skin.
With this pathology, there is always an excess amount of keratin in the skin, the structure of which is disturbed. In this case, the rejection of old skin cells occurs extremely slowly. As a result, scales appear on human skin, in the space between which amino acid complexes accumulate, causing them to harden. For the same reason, the scales are tightly connected to each other.
Patients suffering from ichthyosis experience dry and brittle hair and nails, and many have teeth affected by caries.
With ichthyosis, eye diseases are often observed: such as retinitis, conjunctivitis and myopia.
Causes of ichthyosis
The main cause of ichthyosis is a mutation in genes, which is accompanied by a disturbance in the metabolism of proteins and fats in the body. However, the biochemistry of these processes has not yet been fully studied.
If ichthyosis is an acquired pathology, the causes may be the presence of the following unfavorable factors:
- malfunction of the thyroid gland;
- disturbances in the functioning of the gonads;
- deficiency of vitamins, micro- and macroelements;
- pathologies of the adrenal glands that lead to the occurrence of hormonal disorders;
- serious pathologies of the cardiovascular system;
- various changes that occur to the skin as we age.
Types of ichthyosis
Today, scientists identify the following types of ichthyosis:
- Ichthyosis vulgaris or ichthyosis vulgaris is the most common form of pathology. It is passed on from parents to children. In a mild form, the disease manifests itself in pathological dryness of the skin and the formation of gray or white plaques on them. In more severe cases, these plaques become very dense. At the same time, the skin remains healthy on the folds or in natural folds. Patients with this form always have nail and hair diseases. It is worth noting that the course of the disease becomes more complicated in the summer, especially during the rainy season. At the same time, in winter, the symptoms of the disease decrease or may even disappear completely;
- abortive ichthyosis is ichthyosis in a mild form. With it, the lesion is not present throughout the body, but only on the buttocks and legs;
- black, shiny and white ichthyosis. The distinctive features of black ichthyosis are the appearance on the body of scales of a dark brown, almost black color, white - white, and shiny - shiny;
- X-linked ichthyosis is a pathology caused by a congenital deficiency in the body of steroid sulfatase (the substance through which steroids become active). This disease occurs in approximately 1 person out of 2-6 thousand;
- spiny ichthyosis - differs from other types of this pathology by the presence of a huge number of horny layers that look like needles or thorns;
- pityriasis or simple ichthyosis - a distinctive feature of this form of ichthyosis is the presence of a large number of gray scales, which are attached to the skin in the central region;
- Harlequin ichthyosis is the most severe form of the disease. With it, the skin of babies from the moment of birth is already covered with thick and rough plates. At the same time, their skin already has deep cracks and splits. The mass of plates in this type of disease can be so large that with its weight it can pull back the skin on the face and thus distort facial features, impair breathing and make eating impossible. Such children require long-term and difficult treatment from birth. According to statistics, harlequin ichthyosis is found in approximately 1 in 500 thousand newborns;
- lamellar ichthyosis (lamellar). A recessive gene is responsible for the development of this pathology. The disease occurs equally often among boys and girls and can affect the skin of people regardless of their race. According to statistics, lamellar ichthyosis occurs in 1 child out of 200 thousand. The disease does not affect life expectancy;
- recessive ichthyosis. This is a congenital form of the disease, which affects mainly boys. Children with recessive ichthyosis are more often diagnosed with mental retardation than others. In addition, they often have disturbances in the structure of the skeleton, and epileptic seizures may occur. In some cases, this form of ichthyosis is combined with hypogonadism.
Heredity
Women who want to get pregnant should know that ichthyosis has an autoimmune-dominant pattern of inheritance.
This means:
- if in a couple both parents are carriers of the gene that causes ichthyosis, but do not get sick themselves, then 25% is the probability that their children will get ichthyosis, 25% will not get sick, 50% will not get sick, but will be carriers of the gene;
- if in a couple one parent suffers from ichthyosis, while the other does not, but is a carrier of the gene that causes the disease, then the probability that the children will suffer from ichthyosis is 50:50;
- if both the mother and father of the child suffer from ichthyosis, then their children will also have this pathology;
- If one parent is a carrier of the gene and the other is completely healthy, then the likelihood of having a sick child is very small.
It is worth noting that the birth of children with ichthyosis increases significantly in couples who have a blood connection. If healthy parents gave birth to a healthy child, but over time he developed this pathology, then this may indicate that a spontaneous mutation of a recessive gene has occurred in the child’s body.
Consequences
Congenital ichthyosis is one of the most unpleasant forms of the disease. In such patients, the skin is completely covered with hard plates. Because of this, their skin becomes like a shell. After some time, the plaques on the skin acquire a grayish-yellow color.
In this case, patients may have eversion of the eyelids. Children who have congenital ichthyosis are usually born prematurely, so they have problems with the respiratory system from birth.
Many people with ichthyosis are mentally ill.
Due to weak immunity, they have an increased risk of infection and the development of respiratory failure, as well as liver disease.
That is why it is imperative to treat ichthyosis. A dermatologist deals with the treatment of this pathology. However, if there are concomitant diseases, you may also need the help of an immunologist, nutritionist, neurologist, psychotherapist, ophthalmologist, etc.
Only a doctor will tell patients how to wash with ichthyosis and how to properly care for the body. He will prescribe special creams, ointments and medications that will significantly make the patient’s life easier.
The prognosis for ichthyosis is unfavorable, since metabolic disorders accompanying the pathology will sooner or later cause complications and aggravate the course of the disease.
Prevention of ichthyosis consists of careful monitoring during pregnancy. So, if amniotic fluid is detected in tests, doctors recommend terminating the pregnancy.
Couples who have a very high risk of transmitting the disease to their child are advised to adopt children.
Introduction
Ichthyosis is a descriptive term that denotes various clinical forms of a generalized disorder of keratinization, which manifests itself in chronically occurring severe hardening of large areas of the skin, which is accompanied by xerosis, erythema, cracking, and itching.
This disease is based on genetic disorders that can phenotypically manifest themselves only in the skin (isolated, non-syndromic ichthyosis) or in combination with damage to other organs (syndromic ichthyosis) [1]. Historically, ideas about the etiology, pathogenesis and characteristics of various forms of ichthyosis were formed mainly on the basis of the clinical manifestations of the disease. So, in the 19th century. The “Harlequin fetus” was described, and bullous and non-bullous types of Broca’s ichthyosis were distinguished. Brock proposed the term “congenital ichthyosiform erythroderma.” In 1806, Aliber in his writings mentioned autosomal dominant ichthyosis vulgaris. Further, fundamentally new knowledge regarding ichthyosis appeared only in 1966, when Frost and van Scott clearly described the differences between autosomal dominant “epidermolytic hyperkeratosis” and autosomal recessive “lamellar ichthyosis”. In 1965, Wells and Kerr described X-linked ichthyosis, and in 1970 they identified a separate nosological entity - “steroid sulfatase deficiency.”
Symptoms
Photo: thebeautyinsiders.com
A skin disease such as ichthyosis has its own signs, upon seeing which you should immediately seek medical help and subsequent treatment from a dermatologist. He will conduct an external examination of the skin, then prescribe a diagnosis using tests and choose effective treatment.
The manifestation of any symptoms of ichthyosis depends on the type of disease, since each type has its own characteristics and treatment regimens.
Symptoms depending on the type of disease
Most often, this disease manifests itself in the first months of a child’s life, or in later childhood. Ichthyosis, the symptoms of which vary in the nature of appearance and duration of spread, can be dangerous for the child’s health, and in some cases, for his life.
Symptoms of ichthyosis may include the following:
Ichthyosis vulgaris
A dermatologist can diagnose it in some cases as early as 4 months of age:
- at stage 1, the baby’s skin becomes dry and rough to the touch;
- at stage 2, it begins to become covered with scales, which are whitish in color and fit tightly to each other. The main affected areas are the skin of the arms and legs, and the armpits, elbows and popliteal fossae are not susceptible to the appearance of scales;
- pathological changes affect not only the skin, but also hair, nails, and teeth. Their condition worsens: hair becomes brittle, nails peel off, and caries appears on the teeth;
- Due to decreased immunity, various infections begin to have a negative effect on the body. Such children often have problems in the functioning of the cardiovascular and respiratory systems.
Congenital ichthyosis
You can diagnose it immediately at birth:
- the baby's skin is usually covered with thick horny layers that resemble the skin of a crocodile;
- at birth, the skin is covered with a yellowish film, then it peels off, after which severe redness of the skin occurs throughout the body;
- in severe cases of the disease, blisters may form on the skin;
- in addition to skin lesions, diseases of the endocrine system, central nervous system, dystrophy of nails and hair, as well as eye lesions may be detected.
Acquired ichthyosis
It can be diagnosed due to malignant tumors, metabolic disorders, or long-term use of certain medications. The following signs are present:
- dryness and flaking of the skin;
- hypovitaminosis;
- pathological processes in the kidneys.
Fetal ichthyosis (Harlequin syndrome)
It occurs during the embryonic development of the fetus (at about 4 months), and has the following symptoms at birth:
- severe dry skin, it looks like a shell with large scales;
- eyelids turned outward;
- deformation of parts of the face;
- irregular and disproportionate structure of the arms and legs.
Most often, such children are born dead or die in the first months of life.
Epidermolytic ichthyosis
- the skin is bright red;
- Characterized by the formation of blisters on the skin, which tend to burst, after which a wound surface is formed.
If an infection occurs, an abscess and death of the child may occur.
Ichthyosis, the symptoms of which can appear at any age, is considered a disease that cannot be fully cured; its course can only be maintained during periods of exacerbation. With all types of ichthyosis, the patient suffers from a disorder of the functions of the sweat glands, damage to the body's immune system, and a slowdown in metabolism.
Etiology and pathogenesis
Ichthyosis is a hereditary disease; clinical varieties of ichthyosis are caused by various gene mutations, the biochemical effect of which has not yet been deciphered. In Ichthyosis, disturbances in protein and amino acid metabolism, changes in the activity of certain enzymes (for example, increased activity of oxidative enzymes in the epidermis), disimmunoglobulinemia, etc. are noted. A number of authors attach great importance to vitamin A deficiency, as well as endocrinopathies (insufficiency of the thyroid gland, gonads, adrenal glands). In some cases, ichthyosiform (reminiscent of ichthyosis) skin changes of acquired origin are observed, in relation to which the term “acquired ichthyosis” is sometimes used. These skin changes are usually symptomatic and can be a manifestation of hypovitaminosis, diseases of the hematopoietic system, senile involution of the skin, etc.
Diagnostics
Photo: medaboutme.ru
Ichthyosis is a dermatological disease characterized by the formation of dry scales on the skin similar to fish or reptile scales. The disease got its name for this feature. The disease is usually caused by a genetic hereditary failure. Ichthyosis can develop in a child while still in the womb or be diagnosed later.
Diagnosis of ichthyosis usually occurs by external examination of the patient. During the examination, the doctor should find out the following points:
- Age at which the first symptoms of the disease appeared;
- Did any of their family members suffer from ichthyosis;
- What other skin diseases are present in the patient’s medical history?
Answers to these questions will simplify the diagnosis and help determine the etiology of the disease in each specific case. Since there are different forms of ichthyosis, when making a diagnosis it is important not only to identify the disease, but also its form of manifestation. This is necessary in order to choose the right treatment.
The diagnosis of ichthyosis should be carried out by a dermatologist. He will be able to make a diagnosis based on external signs, and in some cases these signs are enough to distinguish ichthyosis from other similar diseases. During an external examination, the doctor pays attention to the signs of ichthyosis that appear. They may vary depending on the form of the disease. The most common form is ichthyosis vulgaris. It manifests itself in early childhood no later than the age of three. This disease is characterized by the formation of small white or light gray scales on the skin. The scales can affect the entire body or small areas. As a rule, the groin area, the hollows of the armpits, and the bends of the elbows and knees remain untouched.
Over time, the scales may become keratinized and acquire a brown tint. This usually occurs in the absence of timely and effective treatment. In addition, with vulgar ichthyosis, sweating is significantly reduced due to the fact that the sweat glands are underdeveloped. Hair and nails are usually deformed. This is due to a disruption in the synthesis of keratin, which most of the structures of hair and nails are made of.
There is also a sebaceous form of congenital ichthyosis, in which the newborn intensively secretes skin secretion, which then dries up. Due to this, a dense yellowish crust forms on the skin. This type of ichthyosis (unlike the previous one) is curable, but diagnosis can cause some difficulties. Since the crust does not always take on the scaly shape characteristic of classic ichthyosis.
But lamellar congenital ichthyosis does not cause any difficulties in diagnosis. With this type of disease, the child is born with a film that covers his skin. After some time, the film disappears, and scales characteristic of ichthyosis appear underneath it. Unlike the previous one, this form is not curable, but is easier to tolerate than vulgar ichthyosis.
A recessive form of ichthyosis occurs in boys. In this case, shallow cracks form between the scales. The skin resembles that of a snake or crocodile. The scales themselves are very hard and dense, and have a dark tint. Very often this disease is accompanied by diseases such as epilepsy, Down syndrome, cataracts, and underdevelopment of the musculoskeletal system.
In rare cases, patients consult a doctor with an acquired form of ichthyosis. It occurs against the background of various hormonal or gastrointestinal disorders. If, as a result of the diagnosis, it turns out that ichthyosis is of an acquired form, then additional examinations should be prescribed to exclude the presence of tumors that have a malignant form. Acquired ichthyosis often precedes leukemia, sarcoma, or tumors of various organs. The organs of the genitourinary system are most often affected, so special attention should be paid to them during secondary diagnosis.
In addition to the condition of the skin, when diagnosing, the doctor pays attention to the teeth. Very often, patients suffering from ichthyosis have dental caries. However, brittle, curved nails and thin hair can help confirm this assumption.
Also, when diagnosing, you should pay attention to the condition of the eyes. Various forms of conjunctivitis and the rapid development of myopia are concomitant diseases with ichthyosis.
During an external examination, you should pay attention to the feet and palms. The pattern on them is usually more pronounced. And folds can be affected by dryness and flaking. Sometimes it seems as if a small amount of white flour has accumulated in the folds.
Forms of manifestation of ichthyosis may resemble diseases such as:
- Palmar and plantar keratosis - thickening of the layers of skin in the area of the palms and soles, can be visually distinguished from ichthyosis by the area of the lesion and the type of keratinization;
- Lichen pilaris - the skin is first covered with watery papules, which dry out to resemble the scales of ichthyosis. When diagnosing, it is necessary to find out whether there were such papules in place of the scales, accompanied by redness, itching and elevated body temperature.
In addition to the external examination, if differential diagnosis is necessary and other dermatological diseases are excluded, a biopsy of the affected area and histological examination are prescribed. A biopsy can also be ordered during pregnancy; it will show that the skin of the fetus is abnormally thickened. This will serve as evidence that there is a high probability that the child will be born with ichthyosis.
So, the clinical picture of the disease helps dermatologists to easily identify a disease such as ichthyosis. It is quite easy to diagnose, but there is a possibility of other associated diseases. Most often, ichthyosis is observed at an early age or immediately after the birth of a child. But there are cases when ichthyosis is acquired during life and manifests itself after 20 years of age against the background of gastrointestinal disorders or hormonal pathologies.
Fetal ichthyosis
Fetal ichthyosis (syn.: harlequin fetus, colloidal fetus, malignant keratoma) develops at 4-5 months. pregnancy. Inherited autosomal recessively.
Pathohistology
- proliferative hyperkeratosis, acanthosis, lymphocytic infiltrates in the papillary layer of the dermis.
Clinical picture.
The skin of a newborn is covered with a horny shell, consisting of thick horny shields of gray-black color, up to 1 cm thick, smooth or jagged, separated by grooves and cracks. The lips are inactive, the child’s mouth is stretched or so sharply narrowed that it can barely be passed through with a probe. The nose and ears are deformed, the eyelids are turned inside out. The limbs are deformed (club-handed, clubfoot, contractures), hair and nails are absent or dystrophic. Pregnant women often experience premature birth; children with I. can be stillborn, but the majority of such children die a few hours or days after birth as a result of secondary infection, respiratory failure, heart and kidney failure, and inferiority of organs and systems.
Treatment
Photo: gelmintov.net
Ichthyosis is a genetic disease, therefore, answering the question “can ichthyosis be cured?”, doctors claim that this skin disease is completely incurable. The treatment process is aimed mainly at alleviating the patient’s condition and eliminating unfavorable symptoms that occur during exacerbation of the disease. If you notice the very first symptoms, you must immediately consult a dermatologist who will diagnose and prescribe appropriate treatment.
Ichthyosis is treated in different ways: both with medication and with folk remedies. If you decide to start treating ichthyosis using traditional methods, then you must take into account that first you need to consult a doctor who will explain whether these treatment methods can be used for this disease at home.
Drug treatment for ichthyosis
To ensure that the effectiveness of the treatment process is high, the duration of the exacerbation is as short as possible, and the relief of symptoms occurs promptly, the following drugs and ointments can be prescribed by a dermatologist:
- Vitamins - groups C, B, A, E, PP (taken in a course that lasts from 2 to 3 months: 10 drops per day, they will help the patient get rid of hypovitaminosis, tone the body. You can consume not only vitamins purchased in pharmacy, but also contained in food products. Fresh vegetables and fruits fit this description: especially in red and yellow colors. These are grapefruits, oranges, watermelons, pomegranates, peppers, tomatoes, radishes. Fermented milk products - milk, cottage cheese, kefir , sour cream. The basis of the diet is meat - pork, chicken, liver; cheese - processed or feta cheese; nuts - cashews, hazelnuts, peanuts; as well as seafood).
- Lipotropic drugs (they normalize the metabolism of lipids and cholesterol in the body, with their help the release of fat from the liver is accelerated, as a result of this process, fatty infiltration of the liver is reduced. The scales on the skin are softened under the influence of lipotropic drugs. Such drugs are: “Lecithin”, “ Methionine", "Carnitine", "Inositol").
- Immunotherapeutic drugs (correct the body’s immune system, which is most often damaged or weakened. These drugs help restore it and strengthen the body’s protective functions. Such drugs include “U-globulin”, “Viferon”).
- The use of preparations containing iron, calcium, gamma globulin (products containing iron) stimulate the immune system, increase the body's performance, and eliminate fatigue. These include “Aktiferrin”, “Tardiferon”, “Ferrum Lek”. Preparations containing calcium restore the skeletal system, improve brain activity, normalize blood pressure, these include: “Calcemin”, “Calcium gluconate”. Preparations with gamma globulin perform a protective function in the body, preventing viruses and infections from affecting it. These are “Gamma-globulin Human”, “Antihep”, “Biaven”. All drugs that include the elements described above normalize the functional abilities of the body, which has a beneficial effect on the skin).
- Hormonal drugs (prescribed only in cases of severe disease; the treatment regimen and dosage of drugs are selected by the doctor for each patient individually, taking into account the characteristics of his body. Such drugs can be “Thyriodine”, “Insulin”).
- Ointments and creams for external use (their action is aimed at softening the skin and restoring the functionality of the skin. For this disease, a gentle skin care regime is important. Creams must be applied to clean skin after a shower or bath at intervals of 1 or 2 times a day. When choosing ointments, you need to know your body for allergic reactions. The most commonly used for ichthyosis are “Aekol-2”, “Mustela”, “Unna”).
Treatment of ichthyosis using physiotherapeutic methods
Ichthyosis, which can be treated with the help of specialized baths, has its own characteristics. Therefore, the prescription of all medications and baths should be based on the diagnosis of the body, taking into account age characteristics and an individual approach.
In childhood, a doctor may recommend baths with potassium permanganate as therapeutic skin care. After the bath, the child’s skin is lubricated with baby cream containing vitamin A. For adults, baths containing starch and salt are recommended (salt is taken in the proportion of 300 grams per 200 liters of water, the water temperature does not exceed 38 degrees, the procedure is carried out in no more than 25 minutes at intervals less than 2 times a week.The course of therapeutic baths ranges from 8 to 10). Carbon dioxide and sulfide baths have a beneficial effect on tissue metabolism and improve the functionality of the endocrine glands. For those who often relax in dispensaries and health resorts, peat and silt mud are perfect.
Today, mid-wave ultraviolet radiation is popular in the treatment of ichthyosis. With its help, the human body produces vitamin D, stimulates the immune system, normalizes metabolism and replenishes the body with vitamins A and C.
In addition, heliotherapy is widely used in the treatment of ichthyosis - exposure to the skin with sunlight. As a result, vitamin D is also produced and the immune system is restored. It is held only during certain daytime hours: morning from 8.00 to 11.00 and in the evening from 16.00 to 18.00.
If you are wondering: is ichthyosis completely curable? The answer of dermatologists is obvious - only the support of significant functions of the body and alleviation of symptoms is possible. By adhering to all the advice and recommendations of your doctor, you will be able to maintain your body’s condition at the proper level!
Ichthyosis is unilateral
Ichthyosis is unilateral (syn.: unilateral ichthyosiform erythroderma Rossmann). The type of inheritance is unknown.
Pathohistology:
proliferative hyperkeratosis, moderate acanthosis, perivascular inflammatory infiltrates in the papillary layer of the dermis.
Clinical picture.
Patol, a process in the form of erythema with progressive hyperkeratosis covers half of the face, torso, upper limb on the same side; usually combined with bone deformities (vestigial limbs) and cystic changes in the kidney on the side of the skin lesion, as well as with brain disorders detected using electroencephalography.
Medicines
Photo: gp.by
The method of treatment prescribed for ichthyosis will depend on several factors:
- Type of disease;
- Severity;
- Patient's age.
Depending on the combination of these factors, outpatient or inpatient treatment is selected. In this case, the treatment regimen is made up of a combination of the following methods:
- Taking vitamin complexes. A sufficient amount of vitamins consumed help soften the scales, providing a lipotropic effect. It is imperative to take vitamins A, C, E, PP and B vitamins. The dosage of these vitamins should be from 100 to 120% of the daily value for this age.
- Taking immunomodulatory drugs is necessary to restore a weakened immune system. Therapy includes drugs containing calcium and iron and gamma globulin. Medicines for ichthyosis include these substances as the main active ingredients.
- Ichthyosis often manifests itself against the background of thyroid dysfunction. To restore hormonal levels, a series of tests are performed to obtain information about the state of hormones, then medications are prescribed that regulate the amount of necessary hormones towards the norm. Changing hormonal levels in a positive direction reduces the symptoms of the disease. When hormonal therapy is prescribed for breastfed children, the nursing mother must take similar medications.
- Taking baths to apply drugs directly to the affected areas of the skin. Baths can be taken general or local, depending on what percentage of the body is affected by ichthyosis. Drugs such as potassium permanganate, sodium chloride, urea, as well as starch, silt, peat and aromatic retinoids are added to the water. Baths are prescribed to almost all patients as part of complex therapy. They are very effective, since the drug penetrates deeply into the skin through steamed skin cells and has a therapeutic effect. Which of the listed drugs should be added to baths will be determined by the doctor individually for each specific case.
- In combination with baths, local treatment with creams and ointments is effective. The affected areas of the skin need special hydration and nutrition; creams for ichthyosis will help accomplish this task. Creams and ointments can also be additionally fortified and often contain retinol or tocopherol acetate. Ointments have a regenerating effect; if necessary, wound healing and anti-inflammatory ointments are added. In complex therapy, ointments containing D-Panthenol as the main active ingredient are used.
- Also, patients suffering from ichthyosis are prescribed various types of physiotherapeutic procedures: Thalassotherapy is a combination of various drugs of marine origin. It includes swimming in the sea, mud therapy using medicinal sea mud, bathing with sea salt, and seaweed compresses. The therapeutic effect is due to the high content of iodine, salts and minerals that have a beneficial effect on the skin.
- Ultraviolet irradiation and heliotherapy. In mild forms of ichthyosis and appropriate climatic conditions, patients are advised to take short-term sunbathing; in other cases, special devices for ultraviolet irradiation are used, and the procedure is carried out in a hospital setting. It has an antiseptic and regenerating effect.
Ichthyosis is an incurable disease (with rare exceptions), but the methods listed will help reduce symptoms and reduce the risk of complications. The doctor will individually select a complex that includes several of the listed techniques to achieve maximum results.
Ichthyosis spiny
Spiny ichthyosis is a rare form of I., inherited in an autosomal dominant manner. The term “spinous ichthyosis” has been used for many years as the name for various verrucous spiny linear formations, and therefore the terms “epidermal nevus”, “bullous ichthyosiform hyperkeratosis”, etc. have been used as synonyms, which has led to confusion in terminology. This is explained by the wedge, the similarity of the autosomal dominant disease with verrucous epidermal (warty) nevus.
Pathohistology:
hyperkeratosis, granulosis, disorganization of the granular layer and vacuolization of a specific type of cell of the granular and spinous layers due to intra- and intercellular edema, acanthosis, papillomatosis.
Clinical picture.
At birth, only pronounced erythema appears (without peeling or blistering). Over the course of several weeks, the erythema turns pale, diffuse peeling appears, followed by the development of massive warty horny layers in the form of pointed spines and needles protruding 5-10 mm above the skin level. Areas of increased horn formation have an S- and V-shaped linear shape, dirty gray or brown-black color. The nail plates can be thickened, up to onychogryphosis (see Nails). Sometimes this form of I. in boys is combined with mental retardation (imbecility) and epilepsy.
Differentiate with verrucous nevus on the basis of histol, pictures.
Folk remedies
Photo: eco-boom.com
Treatment of ichthyosis at home
Many people diagnosed with ichthyosis ask the question: “How to treat the disease at home?”
In addition to drug therapy, experts recommend performing general strengthening procedures: sunbathing, sea water procedures (if it is not possible to go to the sea, then swimming in a bath with sea salt can replace it). Baths with the addition of glycerin, borax, and soda (100 g per procedure) will be useful. For this to give any result, it is necessary to conduct about 20 sessions.
Regarding the various ointments and herbs that are used in the treatment of ichthyosis at home, you need to be extremely careful and if you intend to use folk remedies, you should consult your doctor. After all, traditional treatment for ichthyosis may not only not help, but also harm the patient. But with the right approach and the right combination with traditional medicine, the effect will be positive.
To reduce unpleasant pain, soothe, moisturize and soften the skin, you can use ointments with an infusion of medicinal herbs, for this you need to mix:
- 200 g St. John's wort oil;
- 50 g each of pine resin and beeswax;
- 10 g each of crushed chalk and crushed celandine;
- 20 g propolis;
- 100 g homemade butter.
Simmer the mixture in a metal saucepan over low heat for 2.5 - 3 hours. And then put it in a dry and dark place for 12 hours. Then boil again and strain through cheesecloth. After this, the product is ready for use; it should be applied to rough areas of the skin 2-3 times a day for 1-2 months, depending on the severity of ichthyosis.
Among the medicinal herbs, you can use: aralia, rowan leaves, tansy, sea buckthorn, plantain, leuzea, peony, all these plants will definitely not cause harm when used. After preparing an infusion of these herbs, its zest can be used to rub dead skin.
To cure ichthyosis at home, you need to strengthen the patient’s immune system, and for this you need to consume as much iron as possible, which is found in certain foods and vitamins.
To summarize all of the above, the disease ichthyosis cannot be completely cured, but when combined with proper traditional medicine and traditional treatment, the area of damage and the severity of the disease can be significantly reduced. It should be remembered that any use of any drug must be accompanied by permission from the doctor.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Forecast
The prognosis for recovery from ichthyosis is usually unfavorable: significant regression of symptoms is observed in isolated cases. The disease is lifelong, occurs in waves with episodes of exacerbations and remissions, and progresses under the influence of aggressive factors.
An unfavorable prognosis for life is observed with fetal ichthyosis: newborns usually die during the first days or weeks of life.
The favorable prognosis decreases in the presence of multiple concomitant pathologies of internal organs and the extent of the lesion.
Prevention
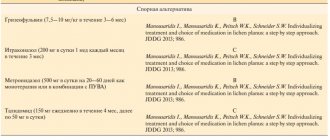
Some patients are prone to recurrent fungal infections. These people may benefit from periodic oral courses of a systemic antifungal agent (terbinafine).
Prevention methods aimed at improving barrier function are very important. They are simple and clear:
- providing humidified , temperature-controlled environment;
- daily bathing using mild detergents;
- use of emollients (petroleum jelly-based products).
It should be remembered that exposure to sunlight worsens the condition by damaging dry skin. However, dead epidermal cells peel off much better when tanned while swimming.