Hyperemia is excessive filling of blood vessels with blood in any part of the peripheral circulatory system as a result of increased inflow of arterial blood or insufficient outflow of venous blood.
Source: otvetprost.com
When arterial vessels dilate, resistance to blood flow decreases, blood pressure increases in small-caliber vessels, the number of functioning capillaries increases, the release of the liquid portion of blood from venules and capillaries into tissue crevices and/or body cavities (transudation) increases, while the volume of the tissue or organ increases, and local temperatures rise.
With venous stagnation, there is a slowdown in blood flow in the microvessels, an increase in blood pressure in them, increased fluid transudation with the subsequent development of edema. Due to the weakening of blood flow, the local temperature decreases, and the blood containing reduced hemoglobin gives the affected area a cyanotic hue.
Short-term hyperemia, as a rule, does not have pronounced negative consequences. If it lasts for a long time, the nutrition of the vascular wall, and then the surrounding tissues, may be disrupted, with the subsequent development of the inflammatory process.
What is hyperemia?
Hyperemia is an excessive overflow of the blood vessels of any organ or part of the body with blood, in which characteristic redness appears in those places, such as the skin.
The main mechanism for the appearance of hyperemia is an increased influx of arterial blood or obstructed outflow of venous blood. In this regard, hyperemia is divided into two main types - arterial (active, in which the flow of blood occurs) and venous (passive, in which the outflow of venous blood is hampered). We will return to a more detailed classification later, but now let's look at the causes of hyperemia.
Hyperemia often occurs in women who spend a lot of time in high heels.
Hyperemia - ICD
ICD-9: 780.99.
Circulatory disorders. Hyperemia - plethora. Stagnation. Ischemia - anemia.
Details General characteristics of circulatory disorders:
1) circulatory disorders cannot be considered in isolation from disorders of lymph circulation and the state of the blood system, since these systems are structurally and functionally connected
2) disturbances in blood and lymph circulation lead to disruption of tissue and cellular metabolism, which means damage to the cell structure, development of dystrophy or necrosis.
Disorders of blood and lymph circulation arise not only as a result of disruption of the circulatory and lymphatic systems, but also of the neurohumoral regulation of the heart, structural damage at any level - the heart, blood vessels, microvasculature, lymphatic vessels, thoracic duct. With a disorder in the regulation of the activity of the heart, the development of a pathological process in it, general disorders arise, and with a disorder in the regulation of the function of the vascular bed in a particular area, as well as its structural breakdown, local disturbances of blood and lymph circulation occur.
Causes of hyperemia
The main causes of blood overflow of blood vessels, or hyperemia, which we actually already said, are:
- Increased arterial blood flow;
- Obstructed outflow of venous blood.
Factors that contribute to a rush of blood (arterial hyperemia) may be:
- Friction of a body part with another surface, object, clothing (for example, tight shoes or underwear);
- Impact on the body of increased or decreased ambient temperature;
- Increased or high body temperature;
- Exposure to body parts or organs of acids, alkalis;
- Entry into the body of foreign proteins and microorganisms, and its poisoning with toxins produced by pathological microflora, especially infection;
- Emotional experiences (stress, feelings of shame, joy, anger);
- Increased heart rate;
- Low atmospheric pressure;
- Accelerated lymph circulation;
- Use of substances that affect blood flow (caffeine, alcohol, drugs, medications, smoking and others);
- Animal and insect bites (mosquito, wasp or bee bite, ant, snake);
- Allergies to food, synthetic fabrics, detergents, etc.
Read also Calcium (Ca) - role in the body, application, daily requirement, sources of calcium
Factors that contribute to obstruction of blood outflow (venous hyperemia) may be:
- Squeezing or narrowing of large vein trunks, which is usually caused by scars, hernias, tumors, prolapsed kidneys, pregnancy, tight watch straps, jewelry;
- Prolonged “abnormal” body position, especially sitting or in an upright position, prolonged stay of the limbs without movement;
- Disturbances in the functioning of the heart (weakening of its pumping activity);
- Walking in high heels.
How is arterial hyperemia classified?
There are two types of this disease: physiological and pathological. In the first case, the causes of arterial hyperemia are physical exertion, emotional stress and eating the wrong foods, for example, too spicy dishes.
Physiological hyperemia can be of two types:
- Working increases blood flow in the body and the functions of certain organs. For example, during the digestion process, the pancreas becomes hyperemic.
- Reactive physiological hyperemia can develop in the kidneys, brain, muscle tissue and skin. A similar phenomenon is observed with a temporary restriction of blood flow with its subsequent sharp resumption.
Pathological hyperemia deserves special attention, as it can be a sign of certain ailments. It develops against the background of certain stimuli. Their role can be played not only by nerve cells, but also by various substances produced by the human body. Arterial hyperemia can develop against the background of a lack of oxygen, with excessive production of serotonin, histamine and with an increase in blood acidity. External irritants can act upon injury, burns, or excess ultraviolet radiation.
People who do not want to deal with arterial hyperemia need to monitor their health. Most often, the cause of the development of pathology is physical and chemical factors, as well as an increase in the load on internal organs. Psycho-emotional stress should also be avoided, which is also a provoking factor in the development of hyperemia.
Symptoms of hyperemia
Signs of hyperemia largely depend on its type.
The main signs of arterial hyperemia:
- Redness of the skin at the site of blood flow;
- The hyperemic area increases in volume and swells;
- Dilatation of arterial vessels;
- Acceleration of blood flow in vessels;
- In the hyperemic area, blood pressure increases;
- The difference in the amount of oxygen in the arteries and veins decreases;
- Pulsation in those vessels where this was not previously the case;
- Accelerated lymph formation and increased lymph flow;
- At the site of hyperemia, tissue temperature rises.
The main signs of venous hyperemia:
- The color of the skin at the site of hyperemia becomes bluish or dark blue;
- The body temperature in a given place decreases;
- The hyperemic area increases in volume and swells.
Other symptoms of hyperemia include:
- Rapid breathing;
- Increased heart rate;
- Redness of the mucous membranes;
- Swelling;
- Bleeding;
- Inhibition of the activity of organs and systems.
Complications of hyperemia
Among the complications of hyperemia are:
- Brain swelling;
- Hydrocephalus;
- Death.
When the skin turns red
Most often, we observe facial hyperemia during the manifestation of strong emotions. Such plethora is characteristic of shy, easily excitable, sensitive and vulnerable people. But it is considered a physiological phenomenon, which is not subject to any treatment, unless it is recommended to treat the nervous system, since such patients are usually diagnosed with neurocirculatory dystonia . However, it all depends on the strength of emotions, because there are those that can make even a calm person lose their temper. Anger, indignation, extreme indignation can easily make you blush.
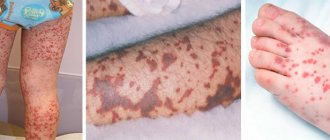
We most often associate skin hyperemia with an allergic reaction , where it is usually acute. First, you can observe redness on the face, which quickly spreads to the entire body, covering the skin on the abdomen, arms and legs. This is already pathological hyperemia.
Thus, excluding physiological hyperemia, other types of plethora indicate pathology, which can be very diverse.
Types of hyperemia
The classification of hyperemia includes the following types of this condition:
According to the development mechanism:
Active hyperemia (arterial) – increased blood flow. Can be divided into:
- neurotonic hyperemia (due to irritation of the nerves that dilate blood vessels);
- neuroparalytic hyperemia (with paralysis of the nerves that constrict blood vessels);
Read also Colds, acute respiratory viral infections and acute respiratory infections. How are these diseases different?
Passive hyperemia (venous) – difficulty in the outflow of venous blood.
Mixed form – both variants of development of this condition are observed.
By etiology:
- Physical;
- Mechanical;
- Chemical;
- Biological;
- Emotional.
By localization:
- Skin hyperemia;
- Hyperemia of the brain;
- Hyperemia of the lungs;
- Hyperemia of the mucous membrane;
- Hyperemia of the eyes (conjunctiva);
- Collateral hyperemia (develops when the main artery is blocked).
With the flow:
- Acute hyperemia;
- Chronic hyperemia.
Venous hyperemia: differences from the arterial form, danger in pathology
Venous hyperemia is more understandably called “stagnant” or “passive”. For it you need:
You can also read: Acute venous insufficiency
- mechanical obstruction, compression of blood outflow pathways through the main veins by a tumor, scar tissue degeneration, pregnant uterus, strangulated hernia;
- decreased strength of heart contractions;
- reducing the suction role of the chest and diaphragm in case of wounds and injuries, enlarged abdomen;
- impaired valve mechanism of the veins for pumping blood and maintaining an upright position (varicose veins);
- increased viscosity and blood clotting, significantly complicating circulation;
- tendency to low blood pressure or acute shock;
- thrombosis or embolism of the venous bed.
The following signs are typical for venous hyperemia:
- bluish color of the skin and mucous membranes in visible areas (limbs, face);
- decrease in temperature in the affected organ and tissues;
- swelling of surrounding tissues.
The pathological mechanism causes a sharp drop in blood flow speed. Fluid enters the interstitial space. Swelling is usually well expressed. The result is tissue hypoxia - oxygen starvation.
Low-mobility blood with platelet aggregations creates a threat of thrombosis and embolization of internal organs. Oxygen deficiency stops metabolism and helps stop the elimination of toxins. Against this background, the addition of infection causes gangrene. And blood platelets form conglomerates of cells. Along with fibrin, the veins begin to block with thrombotic masses, which further increase stagnation.
Venous hyperemia of the brain causes chronic oxygen deficiency of cells with the development of irreversible impairments of intelligence, memory, and mental activity.
Examination of the fundus using an ophthalmoscope is of diagnostic importance.
In clinical conditions, we can talk about the predominant role of some type of hyperemia, since they are associated and cause a general disturbance of microcirculation.
One example of hyperemia in an inflammatory disease is the manifestation of conjunctivitis, you can learn about this in this article.
To clarify, ultrasound and Doppler ultrasound methods are used. They make it possible to identify congestion of internal organs and record its cause.
Developed venous hyperemia is characterized by a corolla of dilated vessels located around the optic nerve nipple
Diagnosis of hyperemia
Diagnosis of hyperemia includes a comprehensive examination of the body, because this condition is not a disease but a symptom, so the research is aimed at detecting possible diseases.
Hyperemia often accompanies diseases such as diseases of the respiratory system (sore throat, pharyngitis, laryngitis), eyes (conjunctivitis), cardiovascular system (ischemia, thrombosis, thrombophlebitis, embolism) and skin (dermatitis, eczema), allergies.
Among the methods for studying the body during hyperemia are:
- History, general examination of the patient;
- Electrocardiography (ECG);
- Computed tomography (CT);
- Ultrasound examination (ultrasound);
- General blood analysis.
Treatment of hyperemia
Treatment of hyperemia includes the following recommendations:
1. Consult a doctor (generalist, dermatologist);
2. Eliminate the influence on the body of the factor that caused the hyperemia;
3. Wash hyperemic (affected) areas of the skin with warm water, but wipe the body in this area only with a soft cloth;
4. The doctor may prescribe drugs aimed at improving blood circulation and microcirculation: Vazaprostan, Cordafen, Curantil, Persantine, Reomacrodex.
5. For stress and emotional distress, sedatives (calming agents) are prescribed: “Valerian”, “Tenoten”.
6. In the case of skin diseases, the affected area is usually treated with special solutions, depending on the specific disease and its cause.
7. The presence of infectious diseases includes the use, depending on the pathogen, of antibacterial, antiviral or antifungal drugs;
8. To cleanse the body of toxins produced by pathogenic microflora (staphylococci, streptococci, pneumococci and others), detoxification therapy is prescribed - Atoxil, Enterosgel and other means.
Read also: Foods that lower blood pressure
9. In case of severe itching, which, when scratched, could cause a rush of blood and swelling, you can take an antihistamine - Suprastin, Claritin.
10. In case of cerebral edema, it is necessary to observe bed and semi-bed rest, rest, and when lying down, the head should be elevated.
11. Eat light, easily digestible foods high in vitamins and microelements (salads, fresh vegetables and fruits, buckwheat, light soups).
12. The doctor may also prescribe a massage course.
13. Walking barefoot on wet grass has a beneficial effect on the body.
14. Sometimes the doctor prescribes procedures such as body rubdown, contrast shower, steam baths, leg wraps, stimulating compress on the stomach and others.
What should you not do if you have hyperemia?
1. To wash or treat the hyperemic area, do not use products that dry the skin - soap, alcohol and others.
2. Do not apply protective creams or ointments to the affected areas.
3. Avoid factors that could potentially cause redness, which we have already discussed in the paragraph “causes of hyperemia” - overheating or hypothermia of the body, chapping, eating spicy food or alcoholic beverages, wearing tight clothing, and others.
Anemia (ischemia)
Anemia is the reduced blood supply to a tissue, organ, or part of the body as a result of insufficient blood flow. In tissue during ischemia, not only hypoxia develops, but also a deficiency of metabolites used by the cell in the process of glycolysis, which activates under conditions of decreased oxygen delivery, which explains the accelerated development of damage.
By prevalence, anemia can be divided into:
-general (anemia)
A disease of the hematopoietic system and is characterized by insufficient levels of red blood cells and hemoglobin.
-local
Tissue changes that occur during anemia are associated with hypoxia or anoxia (oxygen starvation). Depending on the cause of ischemia, the moment of suddenness of its occurrence, the duration of hypoxia and the degree of sensitivity of the tissue to it during ischemia, either subtle changes occur at the level of ultrastructures, or gross destructive changes, up to a heart attack.
Cell damage is also observed when blood flow is restored - reperfusion syndrome
, which includes three components:
1) calcium overload
Reperfusion of ischemic cells that have lost the ability to synthesize sufficient levels of ATP leads to loss of control over ion exchange. An intracellular increase in calcium triggers apoptosis or activates enzymes that disrupt cell membrane structures.
2) formation of reactive oxygen species
Ischemia induces the generation of reactive oxygen species such as superoxide, peroxide, and hydroxyl radical. Free radicals cause a cascade of damage to cell membranes, proteins and chromosomes.
3) development of inflammation
Also, reactive oxygen species activate the inflammatory cascade.
For acute anemia
dystrophic and necrobiotic changes occur.
In this case, glycogen disappears from the tissue, a decrease in the activity of redox enzymes and destruction of mitochondria. Acute ischemia should be considered as a pre-infarction condition. With prolonged anemia,
atrophy of parenchymal elements and sclerosis develop.
Coloring
: for diagnosis, various tetrazolium salts and potassium tellurite are used, which are reduced outside the ischemic areas and color the tissue gray or black, while the ischemic areas are not colored.
Depending on the reasons and conditions
occurrences are distinguished:
a) angiospastic anemia
Occurs as a result of artery spasm due to the action of any irritants. For example, painful stimulation can cause spasm of the arteries and anemia in certain areas of the body. Angiospastic ischemia appears both with negative emotional affects (“angiospasm of unreacted emotions”) and with exposure to low temperatures.
Angiospasm underlies the veno-arterial effect: with an increase in venous pressure, arteriolar spasm develops.
b) obstructive anemia
It develops as a result of the closure of the lumen of the artery by a thrombus (often resulting in vasospasm) or embolus, as a result of the proliferation of connective tissue in the lumen of the artery during inflammation of its wall (obliterating endarteritis), narrowing of the lumen of the artery by an atherosclerotic plaque.
c) compression anemia
Appears when an artery is compressed by a tumor, effusion, tourniquet, or ligature.
d) ischemia as a result of blood redistribution
Observed in cases of hyperemia after anemia. For example, cerebral ischemia when fluid is removed from the abdominal cavity, where a large mass of blood rushes.
Anemia due to arterial spasm is usually short-lived and does not cause any particular distress. However, with prolonged spasms, dystrophy and heart attack may develop. Acute obstructive anemia is especially dangerous, as it often leads to a heart attack. Long-term anemia sooner or later leads to atrophy and sclerosis.
Prevention of hyperemia
Prevention of hyperemia includes compliance with the following rules and recommendations:
— Avoid hypothermia, frostbite or overheating of the body;
— Do not leave untreated diseases to chance, especially cardiovascular, respiratory, digestive and other systems, skin diseases;
— Wear comfortable clothes and shoes, preferably made from natural fabrics;
— When working with aggressive substances (detergents, etc.), be sure to use protective equipment;
— Stop drinking alcohol and smoking;
- Try to move more;
— Observe the rules of personal hygiene;
— Follow the regime – work/rest/sleep;
- Avoid stress;
— Try to eat foods enriched with vitamins and microelements.