Duodeno-gastric reflux is a very unpleasant problem, which is accompanied by feelings of discomfort, pain, burning in the stomach and other unpleasant symptoms. Moreover, this situation is not always pathological. According to statistics, GHD occurs in approximately 15% of people who do not have problems with the digestive system. The reasons for this are unsystematic eating disorders, heavy physical activity, and stress.
Expert opinion
Sevastyanov Roman
General practitioner, hepatologist, gastroenterologist, highest qualification category. Site Expert
We can talk about the disease only in cases where reflux occurs regularly and the patient experiences discomfort for a long period of time. In this case, heartburn may be a symptom of serious gastrointestinal diseases. Therefore, if a burning sensation occurs, you should consult a doctor and undergo an examination, especially if this situation occurs frequently.
General information
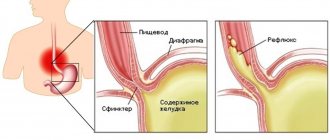
Duodeno-gastric reflux (syn. reflux gastritis , biliary reflux , alkaline gastritis , biliary gastritis ) is a pathological process of retrograde flow of bile contents of the duodenal intestine into the stomach, which can be accompanied by clinical symptoms, histological signs and endoscopic changes of reactive (chemical) gastritis.
The term "refluxus" means "reverse flow". Under physiological conditions, bile from the duodenum should not enter the anatomically overlying parts of the digestive canal, therefore the bile reflex is considered a pathological phenomenon. DGR occurs as a result of excessive flow of bile from the duodenum due to insufficiency of the pylorus, which acts as a barrier to the retrograde flow of bile or due to a violation (reduction) of anterograde peristalsis of the stomach and duodenum. Modern scientific research indicates an increase in the number of diseases caused by the presence of pathological duodenogastric reflux in patients. At the same time, the high prevalence of GHD (in 46-52% of cases) and the frequent combination with chronic gastritis , functional dyspepsia , peptic , GERD , stomach cancer , Barrett's esophagus , sphincter of Oddi dysfunction , duodenostasis , postcholecystectomy syndrome , etc. complicates their course and therapy. GHD is quite common after surgery (in 16% of cases after cholecystectomy and in almost 55% of cases after surgery for duodenal ulcers).
In addition, duodenal reflux can cause the development of metaplasia of the esophageal epithelium, severe esophagitis and squamous cell carcinoma of the esophagus against the background of metaplasia. It should be noted that gastroduodenal reflux in its “pure” form (positioned as an isolated diagnosis) is relatively rare (10-15%) and is mainly diagnosed against the background of other diseases. That is, in most cases, GHD is a syndrome accompanying a number of diseases of the upper gastrointestinal tract.
GHD occurs due to excessive flow of bile from the duodenum due to insufficiency of the pylorus, which acts as a barrier to the retrograde flow of bile or due to a violation (reduction) of anterograde peristalsis of the stomach and duodenum.
Thus, duodenal pathological reflux complicates the course of various organic/functional diseases of the gastrointestinal tract, which necessitates its timely diagnosis, correct clinical interpretation and adequate drug correction.
Prognosis for patients
In general, the disease has a benign course and a favorable prognosis if diagnosed in the early stages of development and subjected to rational therapy.
Neglected cases lead to the development of more serious complications, which significantly worsen a person’s quality of life. These include: gastroesophageal reflux disease, toxic-chemical gastritis C, adenocarcinoma, etc.
Pathogenesis
The pathogenetic mechanisms of development of GDR are based on:
- failure of the sphincter apparatus, which allows the contents of the duodenal intestine to freely reach the stomach through the pyloric/lower esophageal sphincters;
- antroduodenal dysmotility (disorder of coordination between the pyloric/antral parts of the stomach and duodenal intestine), which leads to disruption of control over the direction of flow of duodenal contents;
- elimination of the antireflux barrier after surgery (partial gastrectomy ).
With the development of pathological GHD due to dysfunction of the sphincters, bile retrogradely, as part of the refluxate, enters from the duodenum into the higher located stomach. Components of duodenal contents, represented by bile acids, lysolecithin and trypsin , have an aggressive damaging effect on the gastric mucosa. Taurine conjugated bile acids and lysolecithin have the most pronounced effect, especially at acidic pH, which determines their synergy with hydrochloric acid in the development of gastritis . Trypsin and non-conjugated bile acids have a pronounced toxic effect at slightly alkaline and neutral pH, while the toxicity of non-conjugated bile acids is provided predominantly by ionized forms that can easily penetrate the coolant.
Long-term exposure of the coolant to bile acids contained in bile causes necrobiotic and dystrophic changes in the surface epithelium and leads to the condition of reflux gastritis (gastritis C).
In the presence of Helicobacter pylori, the damaging effect of the refluxant on the coolant is enhanced. The formation of DGR contributes to disruption of the motility of various parts of the gastrointestinal tract and the function of the sphincters, which leads to disruption of the digestive conveyor, has a negative effect on membrane/cavity digestion and absorption of food ingredients, and changes the water balance. The aggressive influence initially manifests itself in the form of increasing atrophy, dysplasia and metaplasia of the coolant, which form the risk of developing gastrocarcinogenesis. The gradual aggressive effect of bile with pancreatic juice contributes to the fact that superficial gastritis progresses and mucosal erosions transform into erosive and ulcerative lesions of the coolant.
Drug treatment
To achieve a positive therapeutic result, it is necessary to take medications prescribed by a doctor. Such agents have different actions. This is protecting the stomach, reducing the level of acids in gastric juice and bile, restoring damaged areas of the mucous membranes of the gastrointestinal tract, preventing the development of complications of GHD, and eliminating pain.
| Name | Description | Dosage | Price |
| Motilium | The drug facilitates the movement of food from the stomach to the intestines. This allows you to reduce the aggressive effect of gastric juice on the walls of the organ. | 1 tablet 3 times a day 15-20 minutes before meals. Duration – up to 28 days. | 450 rub. |
| Almagel | Neutralizes hydrochloric acid in gastric juice, as well as aggressive bile enzymes, protects the walls of the organ from negative effects. | 1 tbsp. l 3 times a day after meals. | 200 rub. |
| Esomeprazole | The drug reduces the production of gastric juice, thereby reducing the degree of its effect on the walls of the digestive organs. | 40 MG 1 time per day. The duration of treatment is 1 month. If the symptoms do not disappear, a repeat course is recommended. In this case, the dosage is reduced by 2 times. | 1600 rub. |
| De-nol | A protective drug that coats the walls of the stomach. The film that appears after taking the product neutralizes the effects of aggressive substances. | 4 times a day before meals, and also 1 time before going to bed. The duration of treatment depends on the severity of symptoms. | 300 rub. |
| Lactofiltrum | The drug has an adsorbing effect, neutralizes harmful substances that negatively affect the walls of the digestive organs, and promotes their elimination. | Take 3-4 times between meals. Duration of treatment is 1-2 weeks. | 250-400 rub. (depending on package size). |
| Ursofalk | The product converts acidic elements, making them less dangerous and toxic to mucous membranes. | Take once a day (in the evening), the course of treatment is about 2 weeks. | 180 rub. |
Causes
The main reasons for the formation of DGR include:
- Congenital/acquired functional deficiency (weakening of the closing function) of the pyloric sphincter.
- Hyperkinetic type (with increased motility) of duodenal peristalsis.
- Inconsistency (discoordination) of the physiological cycles of relaxation/contraction of both the stomach and the DP-gut (migrating motor complex).
- Duodenal hypertension (increased pressure in the lumen of the duodenum), caused by splanchnoptosis (prolapse of internal organs), lumbar lordosis , hernias /malignant neoplasms.
- Long-term inflammation of the duodenum (chronic duodenitis , duodenal ulcer , gastroduodenitis ).
- Lack/absence of hormones ( gastrin ).
- Helminthic infestation (giardiasis).
- Anomalies in the development of the duodenal intestine.
Risk factors for developing duodenogastric reflux include:
- irregular food intake and poor quality nutrition (overeating, dry food, fatty and spicy foods that cause hypersecretion of bile);
- smoking and alcohol abuse;
- old age (after 60 years);
- long-term use of antispasmodics and NSAIDs;
- operations for resection of part of the stomach, cholecystectomy (removal of the gallbladder), anastomosis of the intestine and stomach;
- biliary dyskinesia , cholecystitis ;
- pancreatitis;
- diabetes mellitus , obesity .
Gastroduodenitis
When classifying this related disease, it is customary to distinguish the following three signs:
- Etiological factors and the degree of their predominance;
- Prevalence rate;
- Acidity level.
So, based on the prevailing etiological factors, it is customary to distinguish:
- Primary or exogenous gastroduodenitis;
- Gastroduodenitis of secondary or endogenous type.
According to the degree of prevalence or localization of the disease:
By acidity levels:
- With normal secretory functions;
- With reduced secret functions;
- With enhanced secret functions.
Also, when considering this disease, it is advisable to consider a disorder such as duodenogastric reflux. It is expressed in the reflux of masses from the duodenum into the intestine. The cause of this disease is a disruption of the pylorus and its closure functions. Thus, when entering the intestines, the contents of the duodenum become an irritant and cause type C gastritis or chemical-toxic gastritis.
Symptoms
Symptoms of duodeno-gastric reflux are not specific. As a rule, the disease manifests itself with a predominance of dyspeptic symptoms - nausea, heartburn, air/sour belching, bitterness in the mouth and vomiting bile. Periodically appearing pain in the upper abdomen, intensifying after eating, is cramping in nature and can be provoked by stressful situations, physical activity, or appear after surgery for gastrectomy, cholecystectomy, and with developed duodenal obstruction. Since GHD in its “pure” form is rare and is diagnosed mainly against the background of other gastrointestinal diseases, especially gastroduodenal pathology, the clinical symptoms of reflux are influenced by the symptoms of the underlying disease, which to a certain extent masks the symptoms of GHD.
Physiotherapy
Numerous physiotherapeutic methods help eliminate the symptoms of the disease, restore muscle tissue and the gastric mucosa. For the treatment of GHD the following are used:
- Impact of dynamic currents. Helps restore stomach muscle tone, accelerates the healing process of the mucous membrane, and normalizes the nutrition of stomach tissue.
- Ultrasound. Relieves discomfort, pain, inflammation of the mucous membranes
- UHF reduces the acidity of gastric juice, regulates the process of its production
- Exposure to microwaves. This method is indicated for severe pain. The procedure helps normalize gastric motility, reduces the amount of gastric juice produced, and eliminates inflammatory processes.
Tests and diagnostics
The diagnosis is established on the basis of clinical symptoms and instrumental research methods, among which the most effective are:
- Daily pH-metry - allows you to assess the height of reflux and the profile of intragastric pH.
- Ultrasound diagnostics (echography with water load): with GHD, the retrograde movement of gas and liquid bubbles (corresponding to the reflux of duodenal contents into the stomach) from the pylorus to the body of the stomach is periodically recorded on echograms.
- Transillumination hemomotodynamic monitoring. The difference in motor wave amplitude in the antrum of the stomach and the duodenal bulb is used as a GDR parameter.
- Fibrogastroduodenoscopy (swelling of the coolant, focal hyperemia, pyloric dehiscence).
- X-ray of the stomach (regurgitation of barium from the duodenum into the stomach is noted).
- Fiberoptic spectrophotometry.
If bile reflux is suspected, differential diagnosis is made with acid gastroesophageal reflux and peptic ulcers of the stomach.
What happens in the digestive tract during duodenogastric reflux?
Under the influence of various pathological factors, the smooth digestive process in the stomach and duodenum is disrupted.
When the contents of the duodenum enter the stomach cavity, the mucous membrane of the latter is damaged under the influence of aggressive substances. Enzymes and acids synthesized by the liver and pancreas are able to dissolve the protective mucous layer lining the stomach from the inside, and the gastric epithelium becomes vulnerable to the effects of hydrochloric acid. Inflammation occurs, which with regular duodenogastric reflux becomes chronic. In some cases, duodenogastric reflux can provoke the development of gastroesophageal reflux disease or be combined with it.
Diet
Diet for bile in the stomach
- Efficacy: therapeutic effect after 10 days
- Timing: constantly
- Cost of products: 1400-1500 rubles. in Week
Nutrition correction is a mandatory element of complex therapy. A diet is prescribed for bile in the stomach. Dietary nutrition is aimed at normalizing the motility of the gastroduodenal organs. The main nutritional requirements for the patient are: small frequent meals, adherence to a meal regimen, exclusion from the diet of spicy and salty foods, canned food, marinades, fatty, smoked and fried foods and dishes, wholemeal bread that reduce the rate of gastric emptying. The consumption of various vegetables and legumes rich in fiber (radishes, legumes, turnips, radishes, asparagus) and fruits with rough skin (gooseberries, grapes, dates, currants), as well as coarse cereals (pearl barley, barley, millet, corn) is limited. Limit the consumption of sugar, honey and jam, chocolate. The diet should be based on low-fat boiled, easily digestible foods: light soups, porridges, chicken meat without rough crust, boiled fish and vegetables/vegetable purees, fruit/oatmeal jelly.
Patients with GHD should avoid physical activity and heavy lifting after eating, which increases intra-abdominal pressure. It is equally important to prevent flatulence / constipation . However, since GHD occurs predominantly against the background of other gastrointestinal diseases, a diet for the underlying disease may be prescribed, for example, Diet No. 5 , Diet for gastric ulcer , Diet for gastritis , Diet for gastroduodenitis , etc.
Set of exercises
Starting position (IP), lying on your back. Abdominal breathing: while inhaling deeply, push out the abdominal wall, and while exhaling, pull it in as much as possible. Gradually increase the number of repetitions and range of motion.
- I.P. Same. Slowly raise your straight legs from the floor to 45 degrees. After 10 seconds, lower it.
- I.P. Same. Exercise bike. Bend your legs at the knees and hip joints and imitate riding a bicycle.
- Get on your knees: bend back, forward, to the sides.
Depending on the patient’s physical condition (weight, fitness), age, concomitant diseases, with the permission of the attending physician, more complex exercises are included in the complex.
Diadynamic currents
They are used to stimulate the muscle fibers of the anterior abdominal wall. In addition, they have a pain-relieving effect on the digestive organs.
Prevention
Prevention of GHD consists of:
- Timely treatment of gastrointestinal diseases (especially gastroduodenal pathology).
- Correction of body weight.
- Maintaining the correct diet to ensure physiologically normal gastrointestinal motility.
- Quitting smoking and alcohol abuse.
- Normalization of physical activity and psycho-emotional sphere. Elimination of factors that provoke reflux (lifting weights, exercises with strong abdominal tension, avoiding being in a horizontal position after eating, working in an inclined position).
- Exclusion/avoidance of long-term use of medications that worsen bile rheology and gallbladder motility (antibiotics, expectorants, sedatives, NSAIDs, estrogens, antispasmodics, β-blockers, hypnotics, calcium channel blockers).
How to treat duodeno-gastric reflux?
The treatment regimen for DRG is complex and only a qualified physician can do it. A problem discovered during diagnostic examinations can be eliminated in a short time with the help of the correct selection of a treatment regimen, which will include drug treatment, physiotherapeutic procedures and normalization of the diet. The influence of traditional medicine cannot be ruled out.
The goal of complex physiotherapeutic treatment is to restore the elastic state of the abdominal muscles. This direction includes not only physical exercises, but also procedures (electric myostimulator for the abdominal muscles).
Drug treatment has several objectives: to reduce the irritation of pancreatic juice on the gastric mucosa and restore intestinal motility to pass food unilaterally.
List of sources
- Zvyagintseva T.D., Chernobay A.I. Functional disorders of the motor-evacuation function of the digestive tract and their pathogenetic correction // News of medicine and pharmacy. – 2009.– No. 294. pp. 7–11.
- Zvyagintseva T.D., Chernobay A.I. Duodenogastric reflux in the practice of a gastroenterologist: obvious dangers and hidden threats // Medical newspaper “Health of Ukraine”. 2012.—No. 1. P.11.
- Trukhan D.I., Filimonov S.N. Differential diagnosis of the main gastroenterological syndromes and symptoms. M.: Practical Medicine, 2021. 168 p.
- Trukhan D.I. Rational pharmacotherapy in gastroenterology // Directory of a polyclinic doctor. 2012. No. 10. pp. 18–24.
- Bagnenko G.F., Nazarov E.V., Kabanov M.Yu. Methods of pharmacological correction of motor-evacuation disorders of the stomach and duodenum. // Rus. honey. magazine. Diseases of the digestive system. –2004. – T. 1. – P. 19-23.
Operation
Surgical treatment is used when conservative methods of treatment do not provide the desired result or are ineffective due to the characteristics of the disease. So, when the pylorus gapes, plastic surgery is used, the purpose of which is to plastically reduce it.
Using laparoscopic equipment, the anterior part of the pylorus is placed deep into the duodenal bulb, thus forming a functionally active prepyloric pocket. This pocket takes over the contractile and peristaltic functions of the damaged pylorus.
Which products will be beneficial and which will be harmful?
Symptoms of the disease almost always occur after eating. But it is not enough to simply give up foods that cause heaviness in the stomach or heartburn. A therapeutic diet involves a gentle effect on the digestive system and at the same time contains all the beneficial substances necessary for the body. Here is a short list of foods that are allowed to be consumed:
Replacing your usual food with pureed cereals and pureed soups will help reduce the amount of bile secreted.
- ground porridge (rice, pearl barley, buckwheat, oatmeal);
- puree soups with weak broth;
- steam omelette;
- fish, always lean;
- fresh whole milk;
- low-fat cottage cheese, casseroles based on it;
- lean meat, preferably in the form of souffle, steamed meatballs or cutlets;
- pureed vegetables;
- butter and vegetable oils in small quantities;
- herbal teas;
- dried fruits compote;
- yesterday's bread.
It is advisable to consume the above products in the form of purees. Cook food by steaming, in the oven, or boiling it in water. Thus, it does not irritate the mucous membrane, does not contribute to increased acidity and the release of bile.
A therapeutic diet involves a gentle effect on the digestive system
Some products are recommended to completely eliminate or reduce their consumption. We list the products that are not recommended for patients with duodenogastric reflux. Sometimes their use is acceptable, but is strictly prohibited during an exacerbation:
- sour fruits, especially citrus fruits;
- spicy;
- smoked meats;
- marinades;
- roast;
- sauces;
- spices;
- rich broths;
- honey;
- jam;
- vegetables that cause fermentation in the intestines (for example, cabbage);
- dairy products;
- fresh bread;
- alcohol;
- carbonated drinks;
- coffee, strong tea.
You should avoid junk food during an exacerbation period.
These products are more difficult to digest, promote the secretion of digestive juices, and coffee completely stops the processes occurring in the stomach. You should avoid such food during an exacerbation period. Before returning any foods to your diet, you should consult a gastroenterologist.