Share with friends:
How is GERD treated? The World Journal of Gastrointestinal Pharmacology and Therapeutics states that "effective treatment of GERD may include lifestyle modification, drug therapy, and surgical therapy." If you are one of the many who suffer from symptoms of GERD (or acid reflux), such as difficulty swallowing, digesting or breathing, you will be glad to know that there are many effective natural remedies. These include GERD diet, stress reduction, and exercise. They can help bring you relief without the risks associated with long-term medication use.
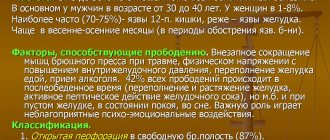
Between 20% and 44% of the total population in industrialized countries suffer from GERD. Many experts believe that the alarmingly high prevalence of GERD is a direct result of eating modern, highly processed foods. Up to 40% of people experience symptoms associated with GERD at least monthly. About 10% - 20% experience symptoms of GERD almost daily. To make matters worse, up to 15% of patients with GERD may eventually develop Barrett's esophagus . Severe tissue damage and scarring of the esophagus causes Barrett's esophagus syndrome. Research shows that the prevalence of GERD is significantly higher in Western countries than in Asian countries. The prevalence there is less than 5%.
According to recent research, many people develop GERD not only because they left acid reflux symptoms untreated. For almost the last 80 years, acid reflux has been considered an early stage of GERD. Today, experts are turning their attention to another contributing factor: chronically high inflammation as the actual culprit of GERD. Inflammation not only contributes to damage to the tissues of the esophagus. It is also associated with many other forms of digestive disorders.
While this finding is important and changes the way we think about GERD, perhaps we shouldn't be surprised. After all, inflammation is the cause of most diseases .
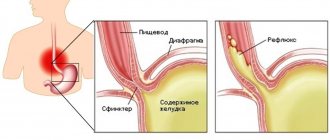
Causes of gastroesophageal reflux
Our body is designed in such a way that the pressure in the stomach cavity is an order of magnitude greater than in the chest cavity. Due to this feature, the phenomenon of food returning back to the upper parts of the digestive tract, in theory, should be constant.
But in practice this does not happen, due to blocking by the esophageal sphincter, which is located at the transition of the esophagus to the stomach. There are a number of factors and reasons that interfere with its proper operation.
1. Factors that cause disruption of the esophageal sphincter. The protective function of the lower sphincter between the stomach and esophagus is regulated and maintained by the tone of its muscular frame.
Scientifically proven:
The maintenance of muscle function is influenced by hormonal factors. It can be noted that hormonal imbalance of the body entails pathological changes and manifestations of the disease.
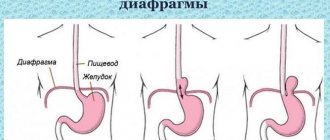
In addition, such factors also include hiatal hernias. It helps compress the area between the esophagus and stomach. Clamping of this part of the organ disrupts the movement of acidic contents from the esophagus.
2. Periodic muscle relaxation. Relaxation is periodic, unrelated, episodes of a sharp decrease in pressure. This phenomenon lasts on average more than 10 seconds. The trigger mechanism is overdistension of the stomach cavity by food intake.
Thus, the causes of this group are overeating, eating food in large portions, poorly processed rough food, and large amounts of liquid at once.
3. Pathological changes in the stomach, which increase the severity of physiological reflux. These include:
- mechanical obstruction, which can be caused by cicatricial stenosis and narrowing, tumor formations, diaphragmatic hernias, congenital defects and developmental anomalies of the gastrointestinal tract.
- changes in the regulation of the central and peripheral nervous system. Occurs after surgery to dissect the vagus nerve, with diabetes mellitus, diabetic neuropathy, after viral and bacterial infections.
- excessive expansion of the walls of the organ due to overeating, aerophagia.
Provoking factors
The main provocateurs are:
- weakening of the permeability valve in the lower region of the esophagus;
- pressure in the lower abdomen (pregnancy, excess weight);
- hernia (displacement of organs);
- gluttony;
- quick snacks on the go;
- ulcer;
- taking antidepressants;
- alcoholism in the chronic stage;
- duodenal ulcer;
- consumption of heavy foods (fast food).
The presence of ulcers in the stomach can trigger the development of GERD
Gastritis and stomach ulcers can also be influencing factors.
Gastroesophageal reflux - symptoms and treatment
Clinical manifestations are very numerous and may coincide with the clinical manifestations of other diseases, thereby misleading the doctor. The main symptoms of the pathology are associated with impaired motor function of the upper gastrointestinal tract.
In addition, the disease can manifest itself in atypical extraesophageal forms. The earliest and most common sign of pathology is:
1. Heartburn. Patients note that they experience a burning sensation in the area of the esophagus or behind the sternum. The symptom may appear after non-compliance with diet, physical activity, drinking alcohol, smoking, carbonated water, spicy and fried foods. Depending on how often heartburn occurs and how long it lasts, degrees of the disease are distinguished:
- mild – the symptom appears less than twice a week;
- average – more than three times a week;
- severe – the symptom appears daily.
2. Belching occurs in every second person with this disease. It is provoked by eating, drinking highly carbonated drinks.
3. Regurgitation of food. A symptom that does not occur often, but also indicates a pathology of the esophageal sphincter. Usually there is a return of liquid food. May appear when the body bends forward.
4. Dysphagia – difficulty passing a bolus of food through the esophagus. This symptom often causes patients to refuse meals, after which rapid weight loss occurs. appears as the disease progresses.
5. Odynophagia – painful sensations when eating.
The patient feels how food passes in the projection of the chest. A symptom complex may appear with severe inflammation of the mucous membrane of the organ.
6. Heaviness in the area of the organ of a burning or pulling nature. Occurs after eating or when a person is lying down.
As noted earlier, gastroesophageal reflux disease GERD may present with symptoms and signs of extraintestinal manifestations. These include:
- frequent dry cough that cannot be treated with antitussive drugs;
- sudden hoarseness of voice;
- nasal congestion and discharge not associated with colds;
- uncontrollable headache.
Classification of the disease:
- Non-erosive - the mucous membrane of the esophagus is involved in the process. The lesion is characterized by redness of the membrane and affects areas of small area and thickness.
- Erosive - erosions appear in the thickness of the organ, which tend to merge and can be complicated by bleeding.
- Barrett's esophagus is the extreme and most severe form of the disease, with total damage to all layers of the organ.
Symptoms of GERD
Heartburn is the main symptom of GERD.
All symptoms of GERD can be divided into esophageal and extra-esophageal. Esophageal symptoms are, as the name suggests, manifestations caused directly by irritation and inflammation of the esophagus:
- heartburn - a burning sensation behind the sternum, as if “rising” from the stomach to the throat;
- belching sour, stomach contents appearing in the mouth,
- discomfort when swallowing - a feeling of a “stuck lump”;
- pain when swallowing (usually a sign of ulcer or erosion of the esophagus).
In children, frequent vomiting may be a symptom of GERD.
Non-esophageal symptoms are manifestations from other organs:
- attacks of coughing or choking in the evening or at night after a heavy meal;
- bronchial asthma, and the patient’s condition does not improve despite adequate therapy;
- pharyngitis and laryngitis: sore throat, hoarseness, coughing;
- erosion of tooth enamel, aphthous stomatitis;
- arrhythmia.
Doctors also suggest that one of the non-esophageal manifestations of GERD may be frequent ear infections.
Diagnosis of the disease
To clarify and determine the diagnosis, various research methods are used. First of all, the doctor pays attention to the patient’s complaints, analyzes them, and then prescribes the necessary manipulation.
- In order not to injure or cause unnecessary discomfort and inconvenience to the patient, the diagnostic search begins with a therapeutic test. The essence of this method is that if there are corresponding complaints, the patient is prescribed to take a weekly course of proton pump inhibitors, for example, omeprazole. If after taking this drug there are no more clinical manifestations, such as heartburn, belching, pain in the epigastric area, then the doctor may suggest a diagnosis of GERD. This method is good because sometimes with other studies, in particular endoscopic, it is not always possible to identify pathology.
- The “golden” standard examination for all patients with the above complaints is pH-metry of the stomach and esophagus. It provides data on the duration and severity of reflux changes.
- A more informative diagnostic method is endoscopic. With its help, you can obtain confirmation of the presence of the disease and assess its severity.
Depending on the endoscopic picture, it is customary all over the world to distinguish the stages of reflux disease. There are 4 degrees in total:
GERD degree 1 - characterized by the absence of damage to the mucous layer of the esophagus in the presence of complaints and clinical symptoms in the patient. Otherwise, this degree is called endoscopically “negative”.
GERD stage 2 – esophagitis. At this degree, the endoscopist describes the picture of isolated shallow lesions of the mucous membrane. The patient experiences typical complaints.
GERD stage 3 - erosive esophagitis. It manifests itself as multiple erosions in the wall of the organ of various diameters and depths.
GERD stage 4 – peptic ulcer of the esophagus. The most formidable and severe form of the disease. It can lead to serious complications, such as bleeding, perforation of the organ wall, and malignancy.
Complications of GERD grade 4:
- Perforation or rupture of the organ wall. Most often, a breakthrough occurs towards the mediastinal organs, which can lead to sepsis, respiratory arrest, circulatory arrest and a threat to life.
- Bleeding from ulcers. They can be both obvious and hidden. Hidden ones are the most dangerous because they cannot be quickly recognized. This makes treatment of the complication difficult. Hidden bleeding poses a threat to the life and health of the patient.
- Stenosis, in other words, narrowing of the lumen of the esophagus. Food passes through such an area very difficult, as a result of which a person may completely refuse to eat.
- Barrett's esophagus is a serious complication, as the risk of developing adenocarcinoma, a malignant tumor of the organ, increases.
How and with what to treat gastroesophageal reflux
Important goals of therapy are: eliminating the symptoms of pathology, improving the quality of life of patients, restoring performance, preventing and treating complications. There are 2 forms of treatment for the disease: conservative and surgical.
Conservative treatment includes:
- teaching the patient the correct normalized daily routine and adherence to a therapeutic diet;
- prescribing the necessary pharmacological agents: antacids, prokinetics, antisecretory agents, H2 receptor blockers, depending on the form and stage of the disease.
Drug therapy
Antacid line of drugs. They help neutralize the reflux of stomach contents into the esophagus, thereby reducing the risk of inflammatory reactions. This group includes various drugs.
Maalox can be in the form of lozenges or syrup. In case of GERD, doctors recommend liquid forms for better effect. In addition to this medicine, phosphalugel, magalfil and others are prescribed in practice.
The most convenient dosage form for use is gels. Usually the drugs are prescribed 3 times a day after meals. An important rule for taking this group of medications is to relieve each attack of heartburn with these medications.
Heartburn makes it worse, so it must be eliminated
Antisecretory drugs. The goal is to eliminate the damaging effect of acidic gastric contents on the mucous membrane of the esophagus.
These medications include omeprazole, lansoprazole, and esomeprazole. They are prescribed in 100% of cases of illness. Helps reduce acidity. They are taken 2 times a day.
An important and indispensable group for GERD are prokinetics. They have an anti-reflux effect. Helps strengthen the muscle frame of the lower esophageal sphincter.
These include: metoclopramide. Its dosage forms are injections and tablet forms. In the absence of strictures and dysphagia, tablets are prescribed. If there are complications of GERD, then injections are prescribed. Domperidone is also prescribed.
Surgical treatment is resorted to in case of severe and serious complications. The edges of ulcerative defects are excised, erosive surfaces and bleeding areas are sutured. Eliminate strictures and scar changes to improve food passage.
Traditional effective treatment for GERD. What problems may arise
Most doctors typically prescribe several categories of GERD medications to help relieve patients' symptoms. They mainly work by reducing the level of hydrochloric acid, which blocks the effects of acid erosion in the esophagus. However, this does not mean that they address the underlying problem causing the symptoms (inflammation, poor diet, etc.). Medications for GERD include:
- Antacids. For example, activated carbon, Maalox, Maalox and Rolaids
- H2 acid blockers, such as Tagamet, Pepcid, Axid and Zantac
- Proton pump inhibitors (PPIs) such as Prilosec, Prevacid and Nexium.
- Although rarely required, antireflux surgery is sometimes performed.
Once you start using medications to effectively treat GERD, such as STIs, your doctor will likely recommend taking them for many years. Unfortunately, chronic use of PPIs can disrupt microbiome . This impairs gut health, alters the immune system, and increases the risk of serious infections such as Clostridium difficile. Long-term use of PPIs can even change the pH levels in the stomach. These changes can block the body's natural ability to absorb key nutrients and alter the acid-base ratio.
Treatment of gastroesophageal reflux with folk remedies
Many patients are very skeptical about the treatment of GERD with folk remedies and methods. However, their effect should not be underestimated. If you choose the right herbal medicine, it will bring great results in treating the disease.
Sea buckthorn, nettle leaves, aloe, chamomile infusions, and propolis have healing properties.
Aloe juice has anti-inflammatory and healing effects. This plant grows in almost every home.
The phytorecipe is very simple:
Squeeze out the juice of the leaves. One teaspoon of this juice is mixed with half a teaspoon of honey. In such proportions, you can infuse a certain amount of infusion and consume it after meals in the amount of 1 teaspoon.
Nettle leaves have hemostatic properties and promote the healing of erosions and ulcers. Also a simple recipe. You can use a pharmacy infusion or prepare it yourself. Collect the leaves of the plant, wash thoroughly and dry.
Then chop, pour boiling water in the proportion of 2 tablespoons of the plant per glass of water. Infuse, strain, drink throughout the day as required. Course 2-3 weeks. You can add 1 teaspoon of sugar to the prepared solution.
Many sources describe the healing effect of celery, or rather its juice. Drink 1 tablespoon of freshly squeezed juice before meals.
Chamomile decoction has anti-inflammatory, analgesic, healing and soothing properties. Brew the herbal mixture with boiling water, infuse and drink in small portions throughout the day.
Diet for gastroesophageal reflux disease
Every patient must follow a diet and proper daily routine, work and rest, as this is the basis and key to successful treatment.
- After eating, take a vertical position for an hour - sitting upright or standing. Under no circumstances should you lie down, this will aggravate the reflux. Avoid physical exercise and exercise, especially bending over, for 2 hours after eating;
- do not wear tight and uncomfortable clothes, especially those that can tighten the chest and abdominal areas
- It is advisable to sleep in a position with the head of the bed raised, in severe cases - in a half-sitting position;
- avoid overeating. Food consumption should be rationed and formed in small portions;
- extreme food intake 4 hours before bedtime;
- exclude irritating foods from the diet: fats, coffee, alcohol, soda, spicy foods, citrus fruits;
- complete cessation of smoking;
- do not gain excess weight;
- When following a diet, it is best to cook low-fat, bland, absolutely non-spicy food in boiled, steamed, half-raw form.