Vaginitis (another name for colpitis) is an infectious disease in which the inner mucous membrane of the vagina (or vagina) becomes inflamed. This is different from vulvitis, where the vulva becomes inflamed.
Most often, colpitis occurs in girls and women of childbearing age (18-45 years). This is one of the most common gynecological diseases.
Not every woman knows what vaginitis is, just like vulvitis. However, many people face it. Without realizing it, girls allow the infection to develop freely. This is mainly due to promiscuous sex life and insufficient adherence to the rules of intimate hygiene. It is inattention to one’s own body that most often becomes the reason why aerobic vaginitis occurs in women.
Types of disease
But not only pathogenic microflora (chlamydia, mycoplasma, gonococci, trichomonas, ureaplasma, viruses, fungi) can act as a pathogen that gives impetus to the appearance and development of vaginitis. If an imbalance in the vaginal environment is caused by the uncontrolled proliferation of microorganisms familiar to it (staphylococci, streptococci, enterococci, candida, gardnerella, Pseudomonas aeruginosa and Escherichia coli), then this opportunistic microflora becomes the causative agent. The first variant of the disease ( specific vaginitis ) is of exogenous (external) origin: the infection is brought into the vagina from the external environment. The second option ( nonspecific vaginitis ) is distinguished by its endogenous (internal) nature: the pathogen belongs to the internal environment of the body.
It is quite difficult to carry out treatment if nonspecific and chronic vaginitis are combined in one case. Then the main goal of long-term therapy will be, firstly, the restoration of normal vaginal microflora - and secondly, preventing the upward progression of the infection and suppressing the inflammatory process in order to minimize the number of relapses in the future.
The chronic form of vaginitis threatens with serious consequences:
- menstrual irregularities;
- inflammation of the female organs;
- inflammation of the ovaries, fallopian tubes;
- inflammation of the uterus;
- threat of infertility.
Causes and risk factors of the disease
In the clinic, a distinction is made between the concepts of “specific” and “nonspecific” inflammation of the vaginal mucosa. The first group occurs after certain bacteria enter the genital tract, causing a characteristic clinical picture and requiring a certain type of treatment. The most common specific vaginitis is caused by:
- trichomonas;
- gonococci;
- mycoplasma;
- ureaplasma;
- fungi of the genus “Candida”;
- chlamydia;
- herpes and human papilloma viruses.
All these infections are included in the group of sexually transmitted diseases. Infection of the vagina occurs during sexual intercourse from an infected partner (clinically he may be healthy).
A nonspecific process occurs due to the activation of opportunistic vaginal flora, which is present in the genital tract of every woman without causing any clinical symptoms. This flora includes staphylococci, streptococci, Haemophilus influenzae, Escherichia coli and other bacteria. They can cause clinical vaginitis in certain conditions that are risk factors:
- with mechanical damage to the vaginal mucosa (due to surgical interventions, childbirth, abortion);
- uncontrolled use of antibiotics, suppressing the normal flora of the vagina;
- insufficient blood supply to the vaginal mucosa, which is an age-related characteristic of the body (atrophic vaginitis);
- hormonal imbalance in diseases of the ovaries, adrenal glands, menopause;
- allergies to condoms, intimate gels and creams, tampons or suppositories;
- failure to maintain personal hygiene.
Consequences of untreated vaginitis
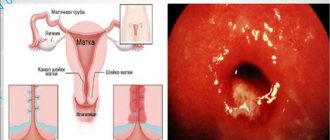
If the disease is not completely treated, then this threatens to spread inflammation to the cervical canal, uterus and ovaries. The infection can affect not only the reproductive system, but also the urinary system.
Sometimes vaginitis develops in childhood. This threatens the development of synechiae, the appearance of ulcers, polyps and scars. In girls under 10 years of age, the vaginal mucosa is very thin, so the disease must be treated with special care. Prescriptions should be given by a pediatric gynecologist.
Author of the article:
Lapikova Valentina Vladimirovna |
Gynecologist, reproductive specialist Education: Diploma in Obstetrics and Gynecology received from the Russian State Medical University of the Federal Agency for Health and Social Development (2010). In 2013, she completed her postgraduate studies at NIMU named after. N.I. Pirogova. Our authors
Types of vaginitis
According to the duration of the inflammatory process, it is divided into several types:
- acute vaginitis.
The inflammatory process develops quickly, more often after unprotected sexual intercourse; manifests itself with violent symptoms, but with a correctly prescribed treatment regimen, it is cured within two weeks;
- subacute vaginitis
– develops against the background of acute inflammation, in the absence of treatment or an incorrectly selected antibiotic therapy regimen. Symptoms become less severe, but continue to occur for more than two weeks;
- chronic vaginitis
diagnosed in cases where symptoms of inflammation persist for more than two months. It is also a consequence of improper treatment or, more often, the result of impaired immunity.
Causes of vaginitis
The vagina is represented by a muscular tube, which is lined from the inside with multilayered epithelium. The upper layer of the epidermis contains a lot of glycogen. They feed on bacteria that are normally always present in the vagina. Beneficial flora include Dederlein bacilli and lactic bacteria.
These microbes break down glycogen and release lactic acid. This way the vagina will be protected on both sides. Dederlein's rods line its epithelium with a dense layer, and lactic acid bacteria produce an acidic secretion. Pathogenic flora cannot reproduce in it. Another reliable factor in protecting the vagina is its ability to self-cleanse. The cells of the organ secrete mucus, which flows down the walls of the vagina and comes out. Along with it, desquamated epithelial particles and dead microbes leave it.
The level of sex hormones determines the level of glycogen in the vaginal cells. Estrogens stimulate its accumulation, and progesterones slow it down. Most progesterone is contained in the blood before the next menstruation. It is not surprising that it is during this period that women more often turn to a gynecologist with a complaint of acute vaginitis, or a relapse of the chronic form of the disease.
The following factors can provoke the development of the disease:
- Vaginal injuries received during childbirth. Because of this, its walls lose the ability to close. The opening in the vagina always remains open. A similar situation can occur after surgery on the genitals.
- Hormonal imbalance in the body: previous childbirth, pregnancy, abortion. Many women experience vaginitis during postmenopause.
- Stress, experiencing strong emotions, serious illnesses and infectious processes in the body can provoke a decrease in immunity.
- Violation of hygiene rules. Pathogenic flora quickly increases its numbers in menstrual blood and other vaginal secretions.
- Diabetes. This process causes excess glycogen deposition in the vaginal walls, causing itching and poor nutrition.
- Vaginitis can be caused by bacteria that cause sexually transmitted infections. Infection occurs through unprotected sexual intercourse.
Gonorrheal vaginitis
Infectious vaginitis in women caused by gonococcus openly manifests itself in 50% of cases. In other women, the infection has a latent course. The incubation period ranges from 3 to 7 days, that is, the first symptoms after sexual contact with a partner may appear only after a week. The characteristic specific symptoms of the disease are as follows:
- purulent vaginal discharge that is white-yellow or greenish in color;
- severe pain, swelling and hyperemia of the mucous membrane. They are noticeable even without special examination;
- frequent false urge to urinate, resulting from gonorrheal inflammation of the urethra.
This species is characterized by the frequent transition of the disease to a chronic form, which is associated with the resistance of bacteria to common antibiotics.
Vaginitis during pregnancy
Vaginitis in pregnant women is not uncommon: the disease is diagnosed in 65% of pregnant women. The disease requires careful treatment, as it can harm not only the mother’s body, but also the child.
The cause of the onset and development of the disease is usually bacteria, since the female immune system is subject to heavy load during gestation. The same can be said about hormonal levels. Because of this, the number of some microorganisms in the vagina becomes insufficient, while others become excessive.
Trichomonas vaginitis
Sometimes the incubation period lasts up to one month. The absence of a regular sexual partner significantly complicates the search and elimination of the primary source of infection. The acute process is manifested by characteristic symptoms:
- Vaginal discharge: foamy, yellow, gray or greenish in color. A specific sign of infection is the presence of gas bubbles in the secreted secretion;
- the smell of discharge is sweetish and unpleasant;
- a constant burning sensation that gets worse after urination or during sex.
This type of vaginitis can become chronic. The reason for this is the fact that the overwhelming number of trichomonas vaginitis is caused by a mixed infection, for which it is difficult to choose the optimal antibiotic therapy regimen.
Symptoms of vaginitis
Depending on the cause that led to the development of vaginitis, its symptoms will vary. However, the disease extremely rarely leads to a deterioration in a woman’s general well-being. Body temperature does not exceed subfebrile levels. If it rises to high values, and intense pain occurs in the vaginal area, then this indicates a severe inflammatory process spreading to the uterus and fatty tissue.
Bacterial vaginitis
This inflammation is caused by opportunistic aerobic bacteria. Such microbes do not require oxygen in order to reproduce. Normally, they are always present on the surface of the skin, but their number is small. When a woman's body is weakened, these bacteria become more numerous. They are able to penetrate the vagina and begin to actively multiply there. In this case, the patient develops purulent discharge, which has a yellow-green color and an unpleasant odor.
During an examination of the organ, the doctor visualizes areas of redness and swollen walls. They are covered with purulent mucus. The smear will reveal epithelial cells that are surrounded by a dense layer of bacteria. The number of Dederlein sticks has been reduced. Sometimes they are missing. The disease often becomes chronic. Over the years, a woman will notice a slight yellowish discharge.
Trichomonas vaginitis
Vaginitis caused by Trichomonas develops several days after sexual intercourse without a condom (provided that the partner was infected). Sometimes it takes 3 days, and sometimes a month, until the first symptoms of the disease appear. As soon as there are a lot of bacteria in the vagina, corresponding clinical signs will appear.
The discharge is foamy. They give off an unpleasant odor. Their color may be whitish or yellow. A woman experiences itching in the perineum and pain in the lower abdomen.
Trichomonas have flagella with which they can move. If the disease is not treated, the bacteria will spread to the uterus, ovaries and even the abdominal cavity. Symptoms of the disease will increase in intensity. The pain will become unbearable. Body temperature will rise to feverish levels. Menstruation becomes irregular.
When examining the vagina, the doctor visualizes inflamed and red walls that are covered with foamy discharge. A latent course of the disease is less common. In this case, vaginitis reveals itself only as a slight inflammation of the epithelium of the organ.
Gonorrheal vaginitis
Gonococci are transmitted sexually. Inflammation develops 3 days after unprotected intimacy. The woman feels pain and burning in the vaginal area, the discharge becomes purulent. White films may be seen in them. They are represented by sections of the epithelium of the mucous membrane, which begins to peel off during gonorrheal vaginitis.
The walls of the vagina are swollen and brightly colored. They have the appearance of crimson papillae. When the disease is severe, films will be visible on the surface of the organ. If you remove them, erosions are visible underneath them, which bleed and do not heal.
Candidal vaginitis
This vaginitis is caused by fungi of the genus Candida. They are found in a smear in every fifth woman. Inflammation develops only in those patients whose immunity fails. The impetus for the manifestation of the disease is metabolic disruptions and hormonal imbalance.
The first symptom of candidal vaginitis is vaginal dryness and itching. The external genitalia become swollen, which indicates developing vulvovaginitis. After a few days, the woman notices that the nature of the discharge is changing. They contain curdled clots that resemble grains of cottage cheese. The mucus gives off a sour smell. Sometimes there is a lot of discharge, and sometimes there is none.
This type of vaginitis often develops before the next menstruation or during pregnancy. Often the disease becomes chronic.
Atrophic vaginitis
This vaginitis is a companion of women who have entered the menopausal period. Patients complain of intense itching. The vagina becomes dry, the discharge has no odor, and there is very little of it.
The doctor visualizes the pale vaginal mucosa, which has a yellowish appearance. Bruises are visible on its surface. The disease may be accompanied by the formation of adhesions.
Chronic vaginitis
Chronic vaginitis is characterized by periods of exacerbation and calm. Signs of inflammation are weak, discharge is insignificant. The disease has been bothering the woman for several years.
Chronic inflammation leads to pathological changes in the vaginal wall. It becomes dense, rough and loses elasticity.
Candidal vaginitis
Among women, this type of vaginitis is the most common. Acute fungal inflammation is characterized by white discharge of a cheesy nature and has a sour odor. Itching, pain and irritation intensify after sex and thermal procedures, sometimes becoming unbearably painful.
Despite the known cause of the disease and a wide range of antifungal drugs, the pathogen is still resistant to treatment; then the disease enters the chronic stage, manifesting itself as unexpressed symptoms that intensify after sexual intercourse or during menstruation.
How to treat colpitis?
An important task in the treatment of chronic vaginitis is to identify the causes that provoke relapses of the disease. If these factors are not eliminated, the disease will return, expanding the area of inflammation.
In order to get rid of vaginitis forever, it may take more than one month of complex therapy using anti-inflammatory, immunomodulatory drugs, medicinal herbs and vitamin-mineral complexes.
Drug treatment
Based on the results of laboratory tests, the doctor prescribes appropriate medications. In the treatment of chronic vaginitis of specific etiology, the following is used:
- antibacterial drugs of general and local action (Amoxiclav, Terzhinan) – stop the spread of bacterial foci, stopping (eliminating) inflammatory processes in the body;
- antifungal agents (Livarol, Candid-B6) - topical suppositories and creams help cope with the fungal pathogen.
Taking medications without first consulting a doctor is strictly prohibited. Inadequate therapy can aggravate the already severe course of the disease.
The nonspecific inflammatory process is eliminated with the help of general strengthening and restorative agents:
- local probiotics (Laktonorm, Vagilak) - to normalize the microflora of the female genital organs;
- vitamin complexes.
Drugs for the treatment of chronic colpitis - photo gallery
Amoxiclav is a broad-spectrum antibiotic.
Terzhinan – vaginal tablets with local antibacterial effect
Livarol - antifungal suppositories
Candide B6 - vaginal tablets with broad antifungal action
Lactonorm – vaginal capsules for normalizing vaginal microflora
How to cure a disease using traditional methods
For prolonged vaginitis, doctors often recommend local preventive measures to disinfect and reduce the symptoms of the disease. Douching with infusions and decoctions of medicinal herbs is well suited for this. The duration of therapy is determined by the attending physician based on the characteristics of the course of vaginitis. The following recipes are considered effective:
- Infusion of plantain and chamomile:
- mix 1 tbsp. l. dry chamomile inflorescences with a spoonful of plantain leaves;
- pour 0.5 liters of boiling water;
- let it brew for an hour;
- cool, strain and use as a douche in doses recommended by your doctor.
- St. John's wort decoction:
- add a tablespoon of chopped St. John's wort per liter of water;
- simmer over low heat for half an hour;
- After the decoction for douching has cooled, it must be filtered.
- Infusion of medicinal herbs:
- mix calendula, sage and chamomile in equal parts in a glass of boiling water;
- hold in a water bath for 15–20 minutes;
- After straining, the infusion is ready for use.
Traditional recipes can only be used on the recommendation of a doctor and taking into account individual reactions to medicinal herbs.
Medicinal herbs for local treatment of vaginitis - photo gallery
Plantain has healing properties
Chamomile has a mild antiseptic effect
St. John's wort is a natural antibiotic and antiseptic.
An infusion of calendula, sage and chamomile has an anti-inflammatory effect
Atrophic vaginitis
The irreversible aging process of a woman’s body also affects the health of her external genitalia. With the onset of menopause, blood circulation in the vaginal mucosa significantly worsens. The number of feeding vessels is significantly reduced, in contrast to which an abundant capillary network develops as a compensatory mechanism. This leads to a complex of clinical symptoms called “atrophic vaginitis.” Its manifestations:
- decrease in vaginal secretion, manifested by pathological dryness of the genital tract and increased susceptibility to sexually transmitted infections;
- bleeding after sexual relations caused by damage to thin-walled capillaries located close to the surface of the vaginal mucosa;
- Dyspareunia is painful sexual intercourse caused by insufficient blood supply and deficiency of vaginal secretions.
Atrophic vaginitis has a slow, gradually progressive course. It is one of the signs marking the end of the reproductive period of a woman’s life.
The mechanism of development of vaginitis
Vaginitis is always characterized by inflammation, but it is not always caused by pathogenic microorganisms. Sometimes the disorder develops when the vaginal walls are injured. This can happen through inaccurate douching, during rough sexual intercourse, or when using personal hygiene products that have an aggressive composition. Sometimes vaginitis develops as a result of allergization of the body. It can occur due to lubricants, contraceptives, or tampons.
The infection can enter the vagina from the external environment, that is, through the ascending route. In this case, bacteria are introduced into the body from the labia, urethra or anus. The second way of spreading the infection is downward. In this case, bacteria enter the vagina from a source of chronic infection that exists in the body. Such a focus can be tonsils, carious teeth, inflamed kidneys. Bacteria reach the vagina through the bloodstream.
Destroyed cells of the vaginal mucosa will produce certain biological substances. They lead to vasodilation, causing blood to stagnate. Leukocytes and plasma leak from the walls of the capillaries. This leads to swelling at the local level.
Since the vaginal mucosa is penetrated by nerve endings, its swelling provokes their irritation. This leads to discomfort. It manifests itself as pain and itching.
Epithelial glands, in response to irritation, begin to produce more mucus in order to wash away pathogenic flora from the surface of the vaginal walls. When leukocytes die en masse, the discharge becomes purulent. Capillaries break down, so blood may be visible in the mucus. If the cause of inflammation is infectious agents, the discharge acquires an unpleasant odor. It indicates a specific inflammation.
Nonspecific vaginitis
Disturbance of the normal microflora of the vagina leads to the activation of opportunistic bacteria, which are present in the genital tract, but do not cause clinical symptoms. Features of this type of disease:
- the onset of the disease is characterized by the presence of one of the predisposing factors: childbirth, abortion, surgery, hormonal changes, etc.;
- vaginal discharge is liquid and watery, without pathological impurities or unpleasant odor. The latter can be added in cases of prolonged process, lack of treatment and insufficient hygiene;
- Nonspecific vaginitis is not characterized by pain and impairment of general condition. It occurs in the form of a local inflammatory process.
How to identify and treat vaginitis
Diagnosis can be made based on consultation, gynecological examination and examination. The doctor will see an inflamed, reddened vaginal mucosa and a coating of discharge on the walls. To clarify the diagnosis you will need:
- study of smear microflora;
- bacteriological culture of secretions - determines the type of infectious agent and sensitivity to groups of antibiotics;
- Ultrasound - prescribed for chronic vaginitis to determine the area of spread of the inflammatory process.
Based on the test results, the doctor will prescribe a course of treatment for vaginitis. Applicable:
- antibacterial, antifungal, anti-inflammatory drugs in the form of ointments, tablets, suppositories, antibiotics;
- ointments with anesthetics to reduce unpleasant symptoms;
- drugs for restoring vaginal microflora, immunomodulators.
Additionally, a break from sexual activity and a diet are recommended: exclusion of sweet foods and alcohol. If the disease is infectious, a course of antibacterial treatment for vaginitis will also be required for the sexual partner, who could become a carrier of the infection. After completion of treatment, repeat tests are performed to exclude relapses.
The inflammation is successfully treated. For recovery, it is important, upon noticing the first signs of vaginitis, to consult a doctor and not self-medicate.
Diagnostics
The clinical picture and clarification of the disease history significantly simplify the laboratory diagnosis of the disease. The main diagnostic task is to find the causative agent in order to prescribe specific treatment later. There are three main methods for determining microorganisms:
- bacterioscopy – visualization of vaginal secretions under a multiple magnification microscope. The technique is widespread due to its practicality, ease of use and low cost. The disadvantage of the study is low specificity. In many cases, the method allows you to see microorganisms, but does not make it possible to accurately differentiate them;
- a bacteriological method known to many as “seeding”. Vaginal secretions are placed in special conditions on a nutrient medium where microorganisms grow. The procedure has a fairly high specificity, but it often takes up to 7 days to complete. In conditions of progressive disease, such a long wait-and-see approach is unacceptable;
- PCR is a highly informative diagnostic method that allows you to quickly identify the causative agent of the disease. Disadvantages - high cost. Conducting a blind study, simply identifying all the most common sexually transmitted infections, is not a cheap pleasure. The technique is justified by a competent approach, in which selective testing is carried out only for certain infections, justified by the clinical picture of the disease.
Diagnostic methods
Diagnosis of the chronic form of vaginitis is complicated by long periods of remission, when a gynecological examination is not as effective as in the acute course of the disease.
The gynecologist makes a diagnosis based on:
- information received from the patient;
- external manifestations of chronic inflammation;
Laboratory examination of vaginal microflora is necessary to confirm the diagnosis
- smear of vaginal flora (helps identify the presence and type of pathogen);
- laboratory tests of urine and blood (indicate the degree of inflammation and the general condition of the body).
Treatment of vaginitis
Therapeutic tactics are determined by the gynecologist, based on the results of the clinical picture, objective examination and specific diagnostic methods.
From the point of view of selectivity, it is much easier to treat specific vaginitis, for which antibacterial, antifungal or antiviral agents are used, to which the pathogen is known to be sensitive.
The main means of treating specific vaginitis:
- trichomoniasis - drugs that are effective against single-cell microorganisms are used (metronidazole, tinidazole, ornidazole). For an acute form of the disease, a 7-day course of treatment is sufficient, for a chronic form – a 10-day course. The drugs can be taken as tablets or, more commonly, vaginal suppositories;
- gonococcal infection - use antibacterial drugs of the penicillin series, cephalosporins and fluoroquinolones (ceftriaxone, cefixime, penicillin, ofloxacin and others). The greatest effectiveness of treatment is observed with intravenous or intramuscular administration of drugs;
- chlamydia and mycoplasma infection - antibiotics of the doxycycline group, fluoroquinolones and macrolides (erythromycin, josamycin, levofloxacin, moxifloxacin). The course of treatment for uncomplicated forms of the disease does not exceed 10 days. The route of drug administration is oral;
- Candidiasis is effectively treated with antifungal drugs. In the acute form of the disease, fluconazole is prescribed at a dose of 150 mcg (1 tablet) once or two doses (200 mcg each) of itraconazole. Chronic and recurrent forms require a 7-day and sometimes two-week course of treatment.
A more difficult task is the treatment of nonspecific vaginitis, which should pursue the goals of exterminating pathogenic microorganisms and enriching the woman’s genital tract with benign bacteria. This often requires a long course of multicomponent therapy:
- drugs effective against anaerobic bacteria (metronidazole, tinidazole, ornidazole);
- antibiotics of the lincosamide group, covering a wide range of opportunistic microorganisms. Drugs such as clindamycin, dalacin and others can be prescribed in the form of tablets, suppositories and vaginal creams;
- antiseptics. An important component of the treatment of nonspecific vaginitis is intimate hygiene using antiseptic drugs. Chlorhexidine and other antiseptics can be used as vaginal suppositories or douches;
- vaginal suppositories containing “beneficial microorganisms”.
An additional component of the treatment of nonspecific vaginitis is the elimination of the “risk factor”. It includes vitamin therapy, correction of hormonal imbalances, taking antiallergic drugs, etc.
Prevention of vaginitis
Intimate hygiene products against vaginitis
Preventive measures to help avoid colpitis include timely treatment of diseases, regular visits to the doctor and a smear test for flora. This will allow you to monitor the state of the microflora and take timely measures to normalize it.
It is also useful to follow a diet in the prevention of colpitis. To generally strengthen the immune system, you should completely give up bad habits, engage in active sports, monitor the quality of your diet and take vitamins if necessary, for example, in the spring and winter, when vitamin deficiency is most pronounced.
It is necessary to carry out hygiene procedures daily: take a shower and wash yourself. It is not recommended to use ordinary soap (even baby soap) or shower gel, as these products can upset the balance of microflora in the vagina. Instead, it is better to use special intimate hygiene products that have a suitable pH. Washing gels for intimate hygiene Ginocomfort were created by specialists of the pharmaceutical company VERTEX; these gels have all the necessary documents and quality certificates.
It is not recommended to overuse panty liners. Use these hygiene products only when necessary, observing replacement periods. You should individually select pads and tampons for critical days, take hygienic measures when changing them, and monitor the duration of use.
To prevent a disease such as vaginitis, women should have more underwear made from natural materials than from synthetic ones. After all, natural materials (cotton, linen, silk) allow air to pass through much better, allowing the intimate area to “breathe.”
It is also recommended to avoid tight and tight panties in favor of looser underwear.
Complications
From the vagina, the infection along the ascending path can reach the cervix, into the uterus itself and cause infection of the tubes and ovaries. Late detection, inadequate treatment and lack of measures to prevent relapse can result in complications. The most common complications include:
- inflammation of the cervix, its inner lining and fallopian tubes. This group of complications is especially dangerous during pregnancy. Rising to the ovum, the infection can provoke miscarriage, premature birth, or due to infection of the amniotic fluid, severe pathology in the newborn. This complication can also cause postpartum endometritis, which, in severe cases, requires removal of the uterus;
- urinary tract infection. The urethra in women has a short, wide lumen and opens at the vestibule of the vagina. These factors contribute to the fairly easy penetration of bacteria into the cavity of the bladder, ureters and kidneys, causing inflammation of these organs;
- Severe cases of complicated vaginitis, if left untreated, result in bacteremia (“blood poisoning”) and a septic state. Mortality in such a situation exceeds the number of favorable outcomes of the disease.
Vaginitis in pregnant women
Yeast colpitis during pregnancy is the most common of all types. Serious hormonal changes lead to changes in microflora and the development of the disease. The course of the disease is quite severe: candidal colpitis during pregnancy is expressed by severe swelling of the mucous membrane, perineal pain, intense discharge with pus and odor.
It is necessary to treat vaginitis during pregnancy in women without delay; the consequences for the child and the expectant mother are very serious:
- intrauterine fetal infection;
- miscarriage or termination of pregnancy for medical reasons;
- placental inflammation, fetoplacental insufficiency;
- perineal ruptures during childbirth;
- sepsis.
Consequences
Any vaginitis, regardless of what type of disease it is, what form it occurs, must be treated, even if the manifestations of the pathogens are insignificant. The infection has two ways of spreading: to the internal female genital organs, as well as to the kidneys and urinary tract. Chronic vaginitis is extremely dangerous for its consequences in the field of a woman’s reproductive health, since it can lead to:
- inflammatory processes in the uterus, fallopian tubes, ovaries (even spread to the pelvic organs);
- cervical erosion;
- infertility (inflammatory processes lead to the formation of adhesions, obstruction of the tubes, and this prevents conception, bearing and birth of children);
- ectopic pregnancy;
- spontaneous abortions;
- premature birth;
- infection of the fetus;
- transmission of infections to newborns;
- sexual disharmony;
- increasing the risk of sexually transmitted diseases or HIV infection.
Prevention measures
The main preventive measure to prevent the development of chronic vaginitis is timely, comprehensive treatment of the primary inflammatory process of the vagina.
The following recommendations will also help reduce risks:
- maintaining adequate intimate hygiene;
- intelligibility in sexual relations;
- use of barrier contraceptives;
- refusal of scented tampons, pads and other hygiene products;
- protection of the genital organs from injury;
- wearing suitable underwear made from natural fabrics;
- diet and normalization of lifestyle.
Disease prevention
Prevention of vaginitis includes:
- suppression of transmission routes of pathogenic bacteria - use of condoms during casual sexual contacts, Miramistin for douching after sex with a new partner;
- maintaining personal hygiene - using soft products to care for the perineum, moderate douching only when necessary, changing pads during menstruation at least once every 4 hours;
- correction of hormonal levels in case of ovarian pathology or during menopause.
Vaginitis is dangerous only for pregnant women if it is severe and often recurs. In this case, the infection can penetrate the membranes and infect the baby. Timely and adequate treatment is necessary to prevent such an outcome of colpitis.