Almost every resident of Russia can find a record of DTP or ADS on their vaccination certificate. These vaccines make a huge difference – they protect people from an early age against diphtheria. Before the introduction of their mass production, this acute infectious disease was one of the most common causes of child mortality in the world. Due to the lack of human immunity, corynebacteria toxins quickly affected various organs, leading to their failure, the development of shock and death.
Fortunately, in the modern world, diphtheria in children and adults has a completely different prognosis and course. Vaccination has radically changed the situation, significantly reducing the prevalence of the disease. Developed medications and medical tactics make it possible to successfully cope with diphtheria in 96% of cases. Diagnosis of the disease is also not difficult, since the mechanism of development and the cause of this pathology are precisely known.
A little about bacteria
The causative agent of diphtheria is Corynebacteria diptheriae. It is quite stable (survives drying and low temperatures) and is well preserved in apartment conditions. To get rid of it, you will need to boil water for about 1 minute, and treat household items or walls with disinfectants (bleach, phenol, chloramines, etc.) for at least 10 minutes. There are many forms, but the symptoms and treatment of diphtheria do not depend on it.
Causes of diphtheria
Diphtheria is an acute anthroponotic infectious disease with an airborne transmission mechanism, characterized by damage to the oropharynx and respiratory tract with the development of fibrinous inflammation at the site of pathogen invasion, as well as toxic damage to the cardiovascular, nervous systems and kidneys.
Mention of diseases resembling diphtheria is contained in the works of Hippocrates in the 5th century. BC e. In 1820-1860. The French physician P. Bretonnet described various clinical forms of “deadly throat ulcer”, he also proposed the name of the disease - “diphtheria”, and his student A. Trousseau later replaced it with the term that is still used today - “diphtheria”.
The causative agent of diphtheria was first discovered by E. Klebs in 1883. In 1884, F. Loeffler isolated a pure culture of the pathogen, and in 1894, E. Behring proposed antitoxic diphtheria serum for the treatment of patients. In 1923, G. Ramon received diphtheria toxoid, which began to be used for routine vaccination against diphtheria. Immunization of children against diphtheria, which has been carried out since the 30s of the 20th century, made it possible to practically eliminate this disease by the mid-1970s. The disease was recorded in isolated cases, but periodically it made itself known in various, even developed, countries.
The situation related to the spread of diphtheria indicates that vaccine-preventable infections remain controlled only if immunoprophylaxis methods are used; Failure to comply with the vaccination schedule and unjustified refusal immediately lead to the activation of the epidemic process.
The causative agent Corynebacterium diphtheriae belongs to the genus Corynebacterium, family Corynebacteriaceae, is aerobic, does not form spores and capsules. Morphologically, it is a gram-positive rod with thickenings at the ends (club-shaped - Babes-Ernst bodies), which in smears is located at an angle to each other like the Latin letter V. According to their biological properties, corynebacteria diphtheria is divided into three biovars:
- mitis (40 serovars),
- gravis (14 serovars),
- intermedius (4 serovars).
Each of these variants has toxigenic and nontoxigenic strains; the latter do not cause disease, but can be transformed into toxigenic ones (toxin synthesis determined by the tox gene). The main pathogenicity factor of the pathogen is exotoxin. Diphtheria toxin has all the properties of exotoxins: pronounced tropism for target cells (mucous membranes, myocardium, nervous system, and slightly less so for the kidneys), thermolability, the ability to stimulate a specific immune response and be neutralized by antitoxic serum. It is one of the strongest toxins in nature, second only to botulinum and tetanus. Consists of two fractions (A and B). Fraction B (thermostable) promotes the binding of the toxin to the receptor and the penetration of fraction A into the tissue. In turn, fraction A (thermolabile) provides a cytotoxic effect.
The diphtheria bacillus is stable in the environment - in diphtheria films, on household items, in corpses for about 2 weeks, in water - up to 3 weeks, but it dies almost instantly when boiled and within 2-3 minutes under the influence of conventional disinfectants
The source of infection for diphtheria is patients of any clinical form, as well as bacteria carriers. Bacterial discharge in the patient begins at the end of the incubation period and continues until the oropharynx is completely sanitized; in some cases, secondary carriage may form.
During diphtheria outbreaks, up to 10% of healthy individuals can be primary carriers. The main transmission mechanism is airborne droplets, less often contact (for skin diphtheria). The causes of diphtheria in a particular person are determined by the intensity of antitoxic immunity, the contagiousness index varies from 10 to 15%. The seasonality of the disease is characteristic - autumn-winter period. Immunity is persistent antitoxic, not antibacterial; repeated cases of the disease are possible, as well as the occurrence of infection in vaccinated individuals; in both cases, the course of the disease is usually mild.
It is generally accepted that diphtheria toxin is the primary factor leading to various pathological changes in the human body; bacteremia is not typical for this disease. Severe diphtheria occurs only in the absence or low titers of antitoxic antibodies. At the site of introduction and reproduction of the pathogen, under the influence of diphtheria toxin and other additional damage factors (hyaluronidase, neuraminidase), a local inflammatory reaction occurs.
The first manifestations are swelling and/or catarrh of the mucous membrane of the tonsils, while neuraminidase reduces pain sensitivity. Subsequently, the toxin penetrates the cells of the mucous membrane, where it forms foci of local necrosis. Subsequently, under the action of thrombokinase, the conversion of fibrinogen into fibrin is activated, resulting in the formation of characteristic fibrin films. In areas covered with multilayered squamous epithelium (tonsils, oropharynx, nose, genitals, eyes), the fibrin film penetrates the entire thickness of the mucous membrane and is firmly fixed to it; in this case, the pathological process can spread beyond the tonsils. This layering is defined as the diphtheritic type of fibrinous inflammation. These films are very difficult to remove from the surface, and due to the intense absorption of the toxin underneath them, the clinical characteristics of the disease are dominated by symptoms of intoxication. On the contrary, in areas covered with single-layer cylindrical epithelium (larynx, trachea, bronchi), the development of the so-called lobar type of fibrinous inflammation is characteristic. Such films are loosely connected and are easily removed, intoxication syndrome is not expressed, but the danger of their tearing off and obstructing the respiratory tract is very high; In addition, if the torn film gets on the tracheal bifurcation, instant death occurs from cardiac arrest due to visceral reflexes.
Sometimes with diphtheria, activation of secondary microflora (streptococci, staphylococci, etc.) occurs, which changes and masks the local clinical manifestations of the disease. Through the lymphatic tract, from the site of formation, the toxin and other biologically active substances move deep into the tissues, causing enlargement of regional lymph nodes, the occurrence of toxic lymphadenitis and swelling of adjacent tissues, which can spread to the submandibular area, neck, chest and beyond. It is believed that with diphtheria, damage to any cells of the body is possible, especially with a high concentration of the toxin. Most often, the so-called target cells are damaged: cardiomyocytes, oligodendrogliocytes, lymphocytes, endothelial cells of the arterial bed, platelets, granulocytes. The process of binding the toxin to receptors occurs in two stages:
- the first is reverse, lasts 8-12 hours;
- the second is irreversible and ends within 30-60 minutes with the formation of a transport system for the A-fragment and penetration of the toxin into the cell cytoplasm, which makes it inaccessible to the action of the antitoxic serum.
A significant weakening of protein synthesis in cell culture in the presence of diphtheria toxin was established. The cell experiences energy “hunger”. The consequence of this is the activation of carbohydrate metabolism, accompanied by a significant intensification of glycolysis (glycolytic “explosion”). The myocardium, unlike skeletal muscles, has a relatively low potential for the activity of glycolytic enzymes, so this compensation mechanism is quickly depleted. Developing hypoxia deepens the specific effect of the toxin.
The above processes occur when diphtheria toxin acts on any cell and cause damage to various organs and systems. The exception is the brain, thyroid gland, as well as cartilage, bones, ligaments, the cells of which are characterized by a very low level of metabolism. This is due to the fact that diphtheria toxin does not pass through their protective barriers.
According to ICD-10, diphtheria is divided into the following clinical forms according to the localization of the pathological local process:
- diphtheria of the pharynx (diphtheria membranous tonsillitis, tonsillar diphtheria),
- nasopharyngeal diphtheria,
- diphtheria of the larynx (diphtheria laryngotracheitis),
- skin diphtheria,
- other diphtheria (anterior nose, eyes, genitals, etc.),
- diphtheria not specified,
In the clinical classification, the following variants of diphtheria are distinguished:
on the spread of the pathological process:
- localized - the process does not extend beyond one anatomical formation,
- widespread - the process spreads to adjacent anatomical formations,
- combined - a combination of lesions of different locations;
according to the nature of the local lesion:
- catarrhal - swelling with a cyanotic tint, which is dominated by hyperemia,
- islet - against the background of edema and cyanosis, films are found in the form of islands of various sizes that are not connected to each other,
- membranous - the affected areas are covered with dense gray films that are almost not removed or leave a bleeding surface after removal.
One of the clinical forms of diphtheria is bacterial carriage:
Bacterial carriage is classified according to its form:
- convalescent - in those who have recovered from diphtheria,
- carriage in healthy individuals;
Based on duration, bacterial carriage is divided into:
- short-term - the pathogen is released for up to 2 weeks,
- average duration - from 2 weeks to 1 month,
- protracted - more than 1 month,
- chronic - from 6 months to several years.
The incubation period of the disease lasts 2-10 days. The main criterion of severity is the degree of toxicosis. The criteria for its determination are the same for diphtheria of the tonsils and pharynx, but are somewhat different for other forms - diphtheria of the anterior part of the nose, diphtheria laryngotracheitis and diphtheria of other localizations. The subclinical course is often diagnosed as carriage of C. diphtheriae. Clinical manifestations (both local and general) are practically absent. The sore throat does not bother me. The patient's health is not affected. This variant of the course can be detected during bacteriological examination, which is carried out during outbreaks of the disease.
Mild diphtheria is characterized by minor toxicosis:
- general weakness is moderate,
- body temperature may remain normal or subfebrile throughout the illness,
- there are no hemodynamic disturbances,
- skin without changes,
- local changes - predominantly catarrhal, in some cases - island, rarely a localized film form of diphtheria of the tonsils and/or nasopharynx occurs,
- swelling of the tonsils and uvula is moderate,
- submandibular lymph nodes may be enlarged,
- sore throat is absent or insignificant,
- myocardial damage can also occur in these forms in the later stages; its characteristic feature is a benign course.
The course of moderate diphtheria is characterized by:
- diphtheria of the tonsils and diphtheria nasopharyngitis - the most common localization at this severity level,
- begins acutely, moderate toxicosis is characteristic,
- general weakness, fatigue, body aches, headache,
- body temperature usually reaches 38-38.5 ° C, but may remain subfebrile,
- sore throat is often moderate and is not a leading symptom,
- pallor of the skin, slight cyanosis of the lips and mucous membranes,
- in the oropharynx, a fibrin layer develops on the tonsils, which can spread to the soft palate, uvula, as well as to neighboring anatomical areas (combined form),
- the submandibular lymph nodes are palpable, enlarged and somewhat painful,
- slight swelling may appear in the submandibular area,
- the course is often complicated by myocarditis and/or polyneuritis.
Severe progression can occur with localized forms, but more often with widespread and combined forms. Characteristic signs of the disease are:
- acute onset, high body temperature in the first days, subsequently decreasing to low-grade and/or even normal against the background of a significant deterioration of the condition,
- headache, body aches, difficulty breathing, insomnia, significant general weakness, lack of appetite, sometimes vomiting,
- sore throat is often a secondary symptom; the feeling of a “lump in the throat”, difficulty swallowing is more disturbing,
- pronounced pallor of the skin, cyanosis of the lips, nasolabial triangle, nail phalanges,
- cyanosis and pronounced swelling are detected on the tonsils and throat,
- the mucous membrane of the throat may be completely covered with a dirty gray coating,
- the tonsils close, excluding the view of the oropharynx,
- deafness of heart sounds, tachycardia, sometimes arrhythmia, bradycardia or even embryocardia,
- even with slight physical exertion, shortness of breath occurs, gradually disappears at rest,
- swelling of the neck of various localizations - from the submandibular region to the collarbones and below,
- The posterior cervical and submandibular lymph nodes are enlarged; it is not always possible to clearly palpate them due to swelling of the subcutaneous fatty tissue.
The disease progresses rapidly. Blood pressure decreases, shortness of breath persists even at rest. Almost always, early myocarditis manifests itself with disturbances in the conduction of the heart rhythm and manifestations of circulatory failure. Polyneuritis appears at the end of the 1st week of illness. Quite often kidney damage occurs.
The hypertoxic course of diphtheria is characterized by symptoms similar to the severe course, but developing rapidly:
- already on the 1st-3rd day from the onset of the disease, death from infectious-toxic shock may occur,
- local manifestations sometimes lag significantly behind the general toxic ones,
- hemorrhages may appear on the mucous membrane of the soft and hard palate, the films become black, which is a dangerous sign and indicates the development of disseminated intravascular coagulation syndrome,
- hemorrhagic impregnation of fibrin layers, significant swelling of the neck, hemorrhage on the skin and hemorrhages in various internal organs.
Diphtheria of the tonsils and diphtheria pharyngitis have a number of common features, which makes it possible to distinguish them from other diseases, including diphtheria with a different localization of the primary focus. The diagnosis is possible with a combination of 2-3 symptoms listed below:
- the onset of the disease is usually acute;
- in all cases, except subclinical, there is a general intoxication syndrome, the severity of which does not always correlate with local changes, especially in the first days of the disease;
- there are layers on the tonsils or other lymphoid formations in the oropharynx that have a fibrin, film-like character;
- sore throat is moderate, often does not correspond to the nature of local changes;
- the voice often takes on a nasal tone;
- swelling of the mucous membrane of the oropharynx and cyanosis prevail over hyperemia;
- the submandibular and cervical lymph nodes are not always enlarged, when clicked they are enlarged - moderately painful on palpation;
- swelling of the subcutaneous fatty tissue of the submandibular region is possible from minor (swelling is localized in the submandibular region) to widespread (reaches the collarbones and below);
- the swelling is dense, painless, the skin over it is not changed (except for hemorrhagic variants), can be asymmetrical and one-sided;
- there is no pronounced antitoxic effect from antibacterial therapy, but rapid improvement is noted within a few hours after the administration of PDS.
This is inherent in all forms of diphtheria of any localization and severity. Diphtheria of the larynx and trachea (laryngotracheal diphtheria, diphtheria croup) as an independent form in adults is registered quite rarely, usually developing in combination with diphtheria of the tonsils and/or nasopharynx.
There are localized (only the larynx is affected) and widespread forms (in addition to the larynx, the trachea and even the bronchi are affected). With laryngotracheal diphtheria, the general intoxication syndrome is expressed quite moderately due to less absorption of the toxin. The severity of the condition is due to the development of severe hypoxia due to obstruction of the airways and obstruction by films; the lower the level of the pathological process (bronchi and even bronchioles), the more pronounced the signs of ARF. Diphtheria of the larynx has a milder course in adults than in children. This is due to the anatomical features of the child’s body. Therefore, the classic triad of diphtheria croup is characteristic of children - a hoarse voice, a rough barking cough and loud stenotic breathing. These manifestations may not be present in adults. Diphtheria croup sequentially passes through three stages in its development:
- Stage I - catarrhal, when during laryngoscopy only swelling and cyanosis/hyperemia of the laryngeal mucosa are detected; at this stage, the general condition of the patient is slightly disturbed - slight general weakness, lack of appetite, body temperature may remain normal or subfebrile; clinical symptoms increase gradually - within a few hours a wet cough and hoarseness appear, within a day the cough becomes barking;
- Stage II - stenotic, difficulty occurs when inhaling air, breathing becomes loud, retraction of the intercostal spaces appears; the voice is aphonic, the cough is silent, patients are restless, cannot find a comfortable position in bed, cyanosis of the lips, tip of the nose, and fingers increases; heart sounds are muffled, tachycardia increases; Blood pressure may decrease slightly, the duration of this period varies from several hours to 2-3 days;
- Stage III - asphyxial, characterized by signs of increasing ARF; breathing is frequent, shallow, arrhythmic, cyanosis increases; patients try to take a more comfortable position for breathing, the pulse is frequent, arrhythmic, blood pressure decreases; The central nervous system suffers from significant hypoxia, which is manifested by confusion, then loss of consciousness, convulsions and death.
If the pathological process spreads to the tracheobronchial tree, clinical symptoms can increase very quickly. From the moment the first signs of the disease appear until death from asphyxia, it takes from several hours to 2-3 days.
The presence of films in the trachea poses a particular threat. The patient's motor agitation and cough contribute to the rejection of the films. Once at the bifurcation of the trachea, they cause sudden death.
Diphtheria of the anterior nasal region is a fairly rare clinical variant. According to the nature of the pathological process, it is divided into the following forms:
- catarrhal,
- catarrhal-ulcerative,
- membranous.
Diphtheria of other localizations - eyes, skin, wounds, external genitalia - is almost always secondary. Among the combined variants of diphtheria, the most common are:
- diphtheria of the tonsils and posterior wall of the pharynx (diphtheria of the oropharynx);
- diphtheria of the tonsils and anterior parts of the nose;
- diphtheria of the tonsils and larynx.
The severity of the combined variants is an order of magnitude higher than the isolated form.
Frequently asked questions from patients (or their parents)
Will a child who has had diphtheria get it again?
The probability of recurrent disease is no more than 5%. And even if this happens, the child will suffer a mild form of diphtheria.
Is it necessary to remove the film that forms in the child’s mouth?
Absolutely not. After adequate treatment with antitoxin, it will separate on its own, and new mucous will take its place. If a person removes it independently, a wound will form, which will soon be closed again with this film.
Why do some unvaccinated children develop the toxic form, while others develop only the common form?
This is determined by the state of the child’s immunity. If it is well developed and the child has not suffered from other infectious diseases in the near past, the likelihood of developing a common form is greater.
The vaccination is quite expensive, and they write on the Internet that it is ineffective - is it worth getting it at all?
Clinical studies by WHO and Russian infectious disease specialists have proven the effectiveness of DTP and ADS vaccines. This vaccination has an average cost of 600-800 rubles in Russia, which can become a problem for the family budget (especially large families). However, a child's coffin costs much more than DTP. And the likelihood that parents of a child without a vaccine will need it increases significantly.
Does the diphtheria vaccine have side effects?
Numerous studies have proven the possibility of only 4 side effects:
- Fever (37-38oC);
- Weaknesses;
- Redness at the injection site;
- The appearance of slight swelling (after injection).
How to treat diphtheria?
All patients with diphtheria, regardless of its clinical form and severity, are subject to mandatory hospitalization in an infectious diseases hospital in the near future. The following are hospitalized in the infectious diseases intensive care unit:
- patients with severe hypertoxicity;
- patients with diphtheria croup.
The main treatment for diphtheria patients is anti-diphtheria serum (ADS). However, it only neutralizes the toxin that circulates in the blood and does not affect the toxin already contained within the cells. The frequency of complications and consequences of the disease largely depend on the timely introduction of PDS.
PDS should be administered immediately upon admission of the patient in compliance with generally accepted rules regarding the administration of heterogeneous sera. There is a dependence of the dose on the severity of the disease:
- light 30,000 - 40,000 IU,
- moderate severity 50,000 - 80,000 IU,
- heavy 90,000 - 120,000 IU,
- very heavy 120,000 - 150,000 IU.
The greatest effect from the introduction of PDS is observed in the first three days from the onset of the disease. Patients with mild and moderate PDS are prescribed intramuscularly, with severe and very severe cases - mainly intravenously in an isotonic solution in combination with glucocorticosteroids at a frequency of 8-12 drops per minute. If necessary, PDS is re-administered after 8-12 hours. This is carried out if there is no antitoxic effect from the first injection.
Then you should use a serum from a different series, but prescribe it in the same dosage. The advisability of introducing the PDS for the third time is more questionable. When administered, PDS circulates in the blood for up to 12-14 days. If the dose is chosen adequately, it is quite enough to neutralize the effect of the toxin. It should be remembered that the toxin circulates in the blood for up to 12 hours.
The toxin formation itself continues as long as the local pathological process persists. Repeated multiple injections of PDS increase the likelihood of allergic reactions. Regardless of the time of admission of the patient to the hospital, PDS is administered if there are changes in the mucous membrane of the oropharynx and taking into account the degree of intoxication.
In case of late hospitalization (during the period of convalescence, when toxicosis and local changes are absent), PDS is not indicated, since it has only an antitoxic effect and does not affect the diphtheria bacillus.
Antitoxic specific therapy must be combined with antibacterial agents. Effective etiotropic therapy is represented by drugs for the treatment of diphtheria such as benzylpenicillin, azithromycin, clarithromycin. The course of treatment should continue until the local process is eliminated, but not less than 5-7 days.
Pathogenetic therapy is aimed at reducing general intoxication manifestations, normalizing homeostasis and activity of the cardiovascular system, as well as preventing complications. There are no strict pathogenetic treatment regimens. To stabilize the electrolyte and acid-base states, predominantly polyionic solutions are prescribed intravenously under the control of the concentration of blood electrolytes (Adesol, Trisel, 5% glucose solution and other solutions). Hydration must be maintained at a sufficient level - up to 2500 ml per day. In case of myocarditis and/or kidney damage, the amount of fluid should be reduced to 1000-1500 ml per day.
In severe cases of diphtheria, the use of protease inhibitors in general therapeutic doses is justified. Drugs that improve the rheological properties of blood and microcirculation are also prescribed. The goal of therapy for diphtheria myocarditis is to ensure adequate hemodynamics. Nonsteroidal anti-inflammatory drugs and glucocorticosteroids are indicated. It is inappropriate to prescribe cardiac glycosides in the near future.
In severe myocarditis, in addition to metabolic therapy, the use of sympathomimetic amines and beta blockers is justified. Treatment of chronic heart failure is carried out by prescribing diuretics (primarily saluretics), which reduce the load on the myocardium. It is better to treat myocarditis together with a cardiologist.
For croup, patients receive distraction therapy: steam inhalations, NSAIDs, sedatives.
For grade II-III stenosis, intubation or even tracheotomy with transfer to artificial ventilation is necessary.
If the nervous system is damaged, neostigmine, B vitamins, and nootropics are additionally prescribed.
During the period of convalescence, massage and exercise therapy are appropriate.
Kidney damage does not require specific therapy.
Clinic
The incubation period lasts from 2 to 10 days . The entrance gate determines the clinical form of diphtheria: diphtheria of the nose, diphtheria of the pharynx, diphtheria of the larynx, diphtheria of the trachea and bronchi, external genitalia, skin (in newborns - umbilical diphtheria). Diphtheria of the pharynx occurs in 90-95% of cases.
According to the nature of the process, they distinguish
- typical (membranous);
- atypical (catarrhal, hypertoxic/hemorrhagic) diphtheria.
Diphtheria of the pharynx can occur in the form of:
- localized
- widespread
- subtoxic,
- toxic form.
The localized form of pharyngeal diphtheria is characterized by the location of plaque only on the tonsils. The patient complains of general malaise, headache, increased body temperature, and slight pain when swallowing.
What diseases can it be associated with?
Complications of diphtheria can occur during any period of the disease, but each period is characterized by certain complications. The timing of their appearance has prognostic significance.
Myocarditis is a common complication of diphtheria. It develops both in the early stages (from the 1st week of illness to the middle of the 2nd week) and in the late stages (from the middle of the 2nd to the 6th week). The higher the degree of toxicosis, the greater the likelihood of diphtheria myocarditis. The earlier myocarditis develops, the more difficult its course and the more severe the consequences; it is the main cause of death in patients with diphtheria.
Damage to the nervous system also occurs in the early (1-2 weeks) and late (up to 4-6 weeks) periods. It manifests itself more often as motor rather than sensory disorders. In the early stages, lesions of the cranial nerves occur. Paresis of the soft palate appears, the voice becomes nasal. Patients are unable to swallow liquid food. There is no gag reflex. Damage to other pairs of cranial nerves can cause paralysis of accommodation, ptosis, and sometimes facial nerve paresis and other disorders. The process can be one- or two-way. Later, flaccid paralysis occurs, such as mono- or polyneuritis. Clinical manifestations depend on the location of the lesion. Damage to the muscles of the laryngeal and oral parts of the throat and limbs is more often observed. Rarely, the diaphragm muscles are affected and paralysis occurs. Diphtheria paresis and paralysis are of a reverse nature, their duration is up to 2-6 months or more.
Kidney damage is caused by the direct action of diphtheria toxin (toxic nephrosis); its severity is minimal and does not lead to the development of acute renal failure and other fatal consequences. Manifested by microhematuria, leukocyturia, cylindruria, proteinuria. AKI in diphtheria is caused by secondary factors: hypovolemia and disseminated intravascular coagulation syndrome on days 5-20 of the disease; multiple organ failure and iatrogenic causes (administration of excessive doses of PDS, administration of aminoglycosides).
ITS is a severe complication of diphtheria, but is extremely rare. Occurs on the 1st-3rd day of the disease and corresponds to the clinical manifestations of the hypertoxic course of the disease. Moreover, phases of shock (I-III) can replace each other so quickly that it is often impossible to determine a clear boundary between them.
DIC syndrome is part of ITS. DIC syndrome can manifest itself as nosebleeds, hemorrhages on the mucous membranes and skin, hemorrhagic impregnation of plaque, and swelling of the subcutaneous fatty tissue of the neck. The appearance of DIC syndrome is a dangerous sign and significantly worsens the prognosis.
The main causes of death in diphtheria are heart damage, asphyxia in diphtheria of the respiratory tract, disseminated intravascular coagulation with the development of acute renal failure or acute respiratory distress syndrome, and the addition of secondary bacterial flora.
Diagnostics
In addition to collecting complaints and describing the development of the disease, it is necessary to examine the patient. You should pay attention to the pain of the lymph nodes and the presence of swelling of the neck.
How to determine neck swelling? To do this, press the skin with your finger for 5-7 seconds and release. If a dimple remains in this place, which gradually disappears, this is a reliable sign of edema.
Standards of medical care (MES) provide for the mandatory conduct of the following studies:
- Complete blood count - to detect signs of bacterial inflammation (ESR more than 20, increased neutrophils);
- A general urine test is used to rule out kidney complications. Pathological signs: presence of protein more than 0.3; more than 2 red blood cells, the presence of renal epithelium (more than 5) or casts;
- Taking a swab from the throat and nose for bacteriological examination is a necessary procedure to confirm the diagnosis of Diphtheria. It does not require preparation of the patient and takes no more than 10 minutes. The results will be ready in no more than five days;
- ECG - assessment of heart function is necessary in order not to miss the onset of complications of diphtheria in the form of heart failure.
- Blood biochemistry (ALT, AST, Bilirubin, Urea, Creatinine) - the first three parameters are necessary to assess liver function, the last two - kidney function.
| Biochemical indicator | Norm |
| AST | up to 45 IU/l (significant with an increase of 2-3 times) |
| ALT | up to 40 IU/l (significant with an increase of 2-3 times) |
| Bilirubin (total) | 5.1 – 17 µmol/l |
| Urea | 2.8-7.5 mmol/l |
| Creatinine |
|
All other examinations are prescribed by the doctor individually, depending on the complexity of the diagnosis or the occurrence of complications in the patient.
Treatment of diphtheria at home
All patients with diphtheria, regardless of its clinical form and severity, are subject to mandatory hospitalization in an infectious diseases hospital in the near future.
For moderate cases, bed rest is indicated, and for severe and hypertoxic cases, strict bed rest for a period of at least 2 weeks. Further, the regimen depends on the patient’s condition, the presence and nature of complications. Patients require constant monitoring. The patient is fed according to the norms of table No. 2. Only in case of diphtheria of the larynx due to difficulty swallowing, food of liquid or semi-liquid consistency should be given in small portions every 3-4 hours. In case of significant sore throat and signs of swallowing impairment, tube feeding is used. It is important to maintain a full drinking regime - hydration must be maintained at a level of up to 2500 ml per day, but in case of myocarditis and/or kidney damage, the amount of fluid should be reduced to 1000-1500 ml per day.
Prevention
Preventing the development of dangerous forms of the disease is quite simple - for this you need to be vaccinated against diphtheria in a timely manner (see the vaccination calendar for children). Currently, combined vaccines are used - DTP or ADS, which provide optimal effect with a minimum of side effects.
How to vaccinate correctly?
DTP is administered to the child three times: at 3, 4.5 and 6 months. The interval cannot be shortened, but it can be slightly increased (for example, after an illness). After the vaccine, the child should be observed for 30 minutes to exclude allergic reactions. DTP should not be given to children who have had whooping cough or are allergic to it. In this case, the ADS vaccine is used.
Read about behavior after vaccinations.
Maintaining good immunity
Diphtheria is a disease that is easier to prevent than to treat. Timely actions by parents to create good immunity in the child will help him avoid acute infection in the future.
Nonspecific measures to prevent diphtheria include maintaining good immunity. To do this, you can use hardening (not earlier than 5 years), moderate physical activity, good nutrition (including vitamins, minerals and other nutrients in the diet), fresh air.
What drugs are used to treat diphtheria?
Etiotropic treatment with antibacterial drugs:
- azithromycin - 0.5 g 2 times a day;
- benzylpenicillin - 1 million units 6 times a day intramuscularly;
- Clarithromycin - 0.5 g 2 times a day.
To restore metabolic processes:
- 5% glucose solution,
- Adesol,
- Trisol.
Diphtheria toxoid
A number of scientists (G. Ramon, M. Mukhamedov, N. Kudryavtseva and M. Zaluzhnaya) when treating diphtheria recommended administering diphtheria toxoid to the patient simultaneously with anti-diphtheria serum. The administration of toxoid stimulates the active production of toxoid by the patient's body according to the type of revaccination. In vaccinated patients, this treatment quickly achieves a positive result.
Diphtheria toxoid is administered in the acute period of the disease in a dose of 0.5 - 1.0 ml. The first injection is given first. After 5-6 days, a second injection is given. A month later - the third.
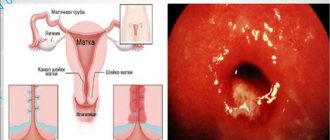
Rice. 5. The photo shows diphtheria-tetanus toxoid.
Treatment of diphtheria with traditional methods
The use of folk remedies for the treatment of diphtheria is assessed with skepticism. This is exactly what should not be used as part of self-medication. The first signs of diphtheria should be a reason to immediately seek professional help from a physician. The administration of anti-diphtheria serum and pharmaceutical drugs as part of drug treatment can destroy the causative agent of the disease, and folk remedies can only be used at the recovery stage. It is best to discuss specific recipes for herbal and fruit infusions with your doctor; he will probably recommend recipes based on the following components:
- lemon, cranberry and lingonberry juices;
- raspberry and currant fruit drinks;
- decoctions of coltsfoot, oregano, linden, calendula;
- tinctures of propolis, eucalyptus, Rhodiola rosea root.
Epidemiology
The source of infection is a patient or a carrier of a toxigenic strain of the pathogen. It can infect others from the last day of the incubation period until complete recovery.
The number of carriers is hundreds of times greater than the number of cases, which is explained by differences in tissue histocompatibility types, for example, according to the HLA system.
Thus, not all infected people get diphtheria.
There is some seasonality in the incidence of diphtheria in the autumn-winter period. Transmission routes are airborne droplets and airborne dust. Infection can occur through shared toys, underwear, etc.
The possibility of alimentary transmission (through milk and dairy products) cannot be ruled out.
Older children and adults who have lost immunity after vaccination are most likely to get diphtheria.
Treatment of diphtheria during pregnancy
Diphtheria during pregnancy is a very rare phenomenon due to mass vaccination. Specific prevention includes routine vaccination and revaccination of the population in accordance with the National Vaccination Calendar. It is carried out with vaccines containing adsorbed diphtheria toxoid (DPT, AKDG1-M, AD-M).
The disease itself, which occurs during pregnancy, is characterized by an unfavorable prognosis. In case of a mild course of the disease, the question of the advisability of continuing pregnancy is decided individually after additional examinations. Infection in the first trimester usually becomes an indication for termination of pregnancy. If infection occurs in the third trimester, the possibility of continuing the pregnancy can be considered if timely medical care was provided to the woman and obstetric support takes place.
Self-medication of diphtheria during pregnancy, as at any other time, is unacceptable.
What it is?
Diphtheria is an acute infectious disease that is caused by a specific pathogen (infectious agent) and is characterized by damage to the upper respiratory tract, skin, cardiovascular and nervous systems. Much less often, diphtheria can affect other organs and tissues.
The disease is characterized by an extremely aggressive course (benign forms are rare), which without timely and adequate treatment can lead to irreversible damage to many organs, the development of toxic shock and even the death of the patient.
Treatment of other diseases starting with the letter - d
| Treatment of DIC syndrome |
| Treatment of dermatitis |
| Treatment of dermatomyositis |
| Treatment of dermatophytosis |
| Treatment of diabetic nephropathy |
| Treatment of diarrhea |
| Treatment of bladder diverticula |
| Treatment of biliary dyskinesia |
| Treatment of dysphagia |
| Treatment of dysphonia |
| Treatment of benign prostatic hyperplasia |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.