Thyroid peroxidase (thyroid peroxidase, TPO) is a key enzyme in the biosynthesis of thyroid hormones.
Thyroid peroxidase is a type I glycosylated transmembrane protein produced in the thyroid gland. Its synthesis occurs on polyribosomes, glycosylation of the protein core of the molecule occurs in the endoplasmic reticulum, and the maturation of the enzyme ends in the Golgi complex. A significant part of the enzyme is found on the perinuclear membrane, in the endoplasmic reticulum and intracellular vesicles. Mature thyroid peroxidase is transported to the apical pole of thyrocytes.
Thyroid peroxidase is an enzyme actively involved in the synthesis of thyroid hormones.
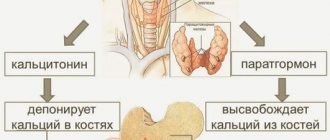
Thyroid peroxidase catalyzes the iodination of tyrosine residues of thyroglobulin (a protein produced by the follicular cells of the thyroid gland) and the fusion of iodotyrosines in the synthesis of the hormones T3 (triiodothyronine) and T4 (thyroxine). Triiodothyronine and thyroxine, in turn, are important for the regulation of metabolism in the body.
Reactions carried out by thyroid peroxidase require iodine, hydrogen peroxide and thyroglobulin. Reduction or complete absence of thyroid peroxidase activity is one of the causes of congenital hypothyroidism.
A significant increase in antibodies to thyroid peroxidase is observed in autoimmune thyroiditis (values can exceed 1000 U/l).
Thyroid peroxidase is one of the main antigens in autoimmune diseases of the thyroid gland. In pathologies such as Hashimoto's thyroiditis and Graves' disease (occurring with thyrotoxicosis), there is a loss of immunological tolerance to TPO. Specific markers of these diseases are antibodies to thyroid peroxidase (AT-TPO, antibodies to the antigen of the microsomal fraction of thyrocytes).
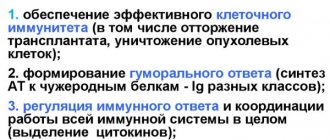
Antibodies to thyroid peroxidase are produced predominantly by B lymphocytes that infiltrate the thyroid gland; the level of antibodies reflects the severity of lymphoid infiltration. The prevalence of TPO antibodies among individuals without thyroid dysfunction is approximately 26%.
What do antibodies to thyroid peroxidase show?
Thyroid peroxidase (TPO) is a special enzyme produced by thyroid tissue, one of the basic antigens in the human body. The main function is the synthesis of thyroxine and triiodothyronine. The TPO test is a marker of autoimmune diseases and thyroid diseases.
Antibodies to thyroid peroxidase determine the severity of the protective reaction to one’s own cells. If the production of the TPO enzyme is impaired, the immune system recognizes the antibodies as harmful. In the fight against thyroid peroxidase, hormone synthesis decreases, hypothyroidism, thyroiditis and other autoimmune diseases develop.
Indications for testing
List of indications for anti-TPO testing:
- chronic thyroiditis (Hashimoto type);
- diagnosis of thyroid function disorders;
- euthyroid goiter;
- screening of pregnant women in the first trimester to identify the risk of thyroid dysfunction;
- establishing the cause of miscarriage and infertility;
- diagnosing rheumatoid arthritis, systemic lupus erythematosus and other autoimmune pathologies;
- disruption of the production of hormones TSH, T3, T4.
Important!
In newborns, the indication for testing is the presence of antibodies to TPO in the mother during pregnancy.
Diagnostics are also used to assess the normal functioning of the thyroid gland before starting therapy with interferons, amiodarone and lithium-based drugs.
Who is diagnosed?
If thyroid antibodies are elevated, this leads to serious changes in the functioning of the entire endocrine system. T3 and T4 are involved in metabolism, the speed of which determines the functioning of the nervous, cardiovascular and other systems. Enzyme immunoassay is prescribed for:
- systemic autoimmune diseases;
- thyroid tumors;
- reproductive dysfunction in women;
- suspected autoimmune inflammation of the gland.
Increased or decreased concentrations of thyroid hormones affect the well-being of patients. An antibody test is carried out for characteristic symptoms of thyroid pathologies:
- causeless weight gain or loss;
- dry skin;
- puffiness of the face;
- chronic constipation;
- drowsiness;
- bulging eyes;
- decreased performance;
- swelling of the lower extremities;
- emotional instability;
- tachycardia;
- neck deformity;
- insomnia;
- lethargy or overexcitement.
Enzyme immunoassay is performed in the differential diagnosis of endocrine diseases and in the treatment of children born to women with thyroid diseases. The study of antibodies to thyroglobulin is used for monitoring in the treatment of thyroid cancer.
Preparing for a blood test
In preparation for donating blood, it is necessary to perform a number of activities:
- You should not take any medications on the day of blood donation;
- do not chew chewing gum;
- blood is donated on an empty stomach before 11.00 am;
- no smoking.
A blood test is taken in the morning on an empty stomach.
If there have been surgical interventions recently or there have been infectious diseases, the test result may be inaccurate.
When preparing for the test, it is important to stabilize the emotional background and avoid stressful situations. Immediately on the day of the analysis, you can drink clean still water.
Technique
The most modern and effective method for detecting antibodies in blood serum is immunofluorescence analysis. With the help of such a laboratory test, it is possible to determine the type and titer (activity) of immunoglobulins, as well as to determine how much the pathology has developed. The research includes the following stages:
- the laboratory assistant takes biological material from the patient;
- a few drops of the resulting blood are dripped onto a special plate with wells containing purified antigens of the suspected pathogen;
- then the laboratory assistant adds a special reagent to the wells;
- Taking into account the staining, the doctor draws conclusions about the result of the analysis.
The study itself can be of 2 types:
- quality. Prescribed to confirm the presence or absence of the desired antigen;
- quantitative. This type of analysis is considered more complex and shows the concentration of antibodies in the serum being studied. It can be used to assess how quickly the infection is developing.
Regardless of the type of analysis, deciphering the results takes from 1 to 3 days.
Upon contact with the reagent, antibodies change color, indicating a positive reaction.
AT-TPO norm in women and men
Indicators may vary depending on age, the norm is the same for men and women.
Results of biochemical analysis for AT-TPO
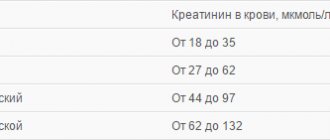
Table of values:
| Age | Normal values (units/ml) | |
| Less than 50 years old | 0-34,9 | |
| From 50 years and older | 1-99,9 | |
| During pregnancy | 0-12 weeks – up to 25 units/ml | 13-40 weeks – 30-56 units/ml |
An increase of 20 units/ml or less means a variant of the norm, does not require correction with drugs, dynamic monitoring and observation of the patient is prescribed. An increase in the value by more than 20–25 units/ml is a sign of pathology and requires clarification of the cause.
Decoding the results and when to see a doctor
Test results will be reported as IU/ml or units/ml. According to the table of normal indicators given earlier, it is not difficult to independently understand whether the level of antibodies is elevated. But the problem is that studies can be conducted in different ways, so it is not recommended to decipher the test results yourself. You need to contact an endocrinologist, and he will make an accurate diagnosis.
If the patient’s body has a deficiency of T4 and T3 and at the same time a high AT-TPO level is registered, then this indicates pathological processes in the thyroid gland or other internal organ. In some situations, an increased antibody level is a temporary phenomenon and does not require treatment, but normalization of the antibody balance. It is impossible to determine such nuances on your own.
The endocrinologist considers each situation individually, taking into account other features of the patient’s health condition and his medical history. If he finds it difficult to make a final diagnosis, the endocrinologist refers the patient to a consultation with specialists and additional examinations.
If there are high fluctuations in antibodies during pregnancy, a woman should visit an endocrinologist and obstetrician-gynecologist to monitor the state of the antibody. As a rule, the first testing is carried out before the 12th week of pregnancy, and then every trimester.
In some situations, if the AT-TPO level is elevated, the doctor may only prescribe a corrective diet. In another case, with the same data, more serious therapeutic measures may be required.
Reasons for deviations from the norm
Increased levels of antibodies to thyroid hormone occur in 7% of people. Children and women encounter it more often, especially during menopause.
AT-TPO is increased - what does this mean?
The main reason for an increase in the level of TPO antibodies is diseases caused by improper functioning of the thyroid gland:
- de Crevin's syndrome - a subacute type of thyroiditis;
- idiopathic hypothyroidism;
- Hashimoto's disease – chronic phase of thyroiditis;
- Graves' disease - diffuse goiter;
- nodular toxic goiter;
- autoimmune thyroiditis;
- dysfunction of the thyroid gland after childbirth;
- pathology of non-thyroid autoimmune form;
- hyperthyroidism;
- carcinoma (cancer) of the thyroid gland.
Increased hormone levels are caused by improper functioning of the thyroid gland.
An increase in antibody levels may be associated with diseases not related to the functioning of the thyroid gland:
- rheumatism;
- diabetes;
- renal failure;
- irradiation;
- endocrine system injury.
By deciphering the result, you can determine whether the disease is manifesting itself or is already in the acute phase:
- indicators are 20–30 units higher than normal – the initial stage of autoimmune disorders, diabetes, vasculitis, rheumatoid arthritis;
- more than 1000 units – thyroiditis, goiter.
An increase in the rate by 5–10 units/ml is provoked by surgical manipulations on the thyroid gland, emotional stress, mental disorders, respiratory problems, physiotherapy in the neck area, and inflammatory foci.
Why is AT-TPO lowered?
During normal functioning of the thyroid gland, antibodies to TPO should not be detected at all. But there are variations in the interpretation of the reference values of the norm.
Indicators may be reduced due to an error in the test, in which case it must be retaken
Reduced performance may be due to the following reasons:
- a harbinger of an autoimmune disease;
- the norm for a particular person, which is determined by genetic inheritance;
- test errors.
Indicators below normal (a decrease of 10 units/ml or less) occur in 10% of completely healthy people and are a variant of the physiological norm for a particular person and do not require correction with medications.
How to determine
The main indicator of autoimmune thyroid disease is the so-called AT titer . It allows you to determine the presence of pathology at the most basic level. The antibody level tests themselves are included in the so-called thyroid screening panel. This means that the patient must be tested for TSH, triiodothyronine (total and free), and thyroxine.
Antibodies to thyroid peroxidase are highly elevated in women after childbirth. If this happens, then, as a rule, 8-10 months after the birth of the child, antibody levels return to normal. However, during pregnancy, tests are sometimes required, since ATs can pass through the hematoplacental barrier and negatively affect the health of the fetus.
In order to evaluate the AT-TPO indicators, a venous blood test is performed. As a rule, it is always taken immediately after surgery on the thyroid gland (for example, when it is removed) or after a serious infectious disease. If inflammatory processes occur in the patient’s body, the research results may be distorted.
If, based on the results of the research, it is possible to find out that the patient has too high a level of AT-TPO, then he is referred for an ultrasound and a biopsy.
What to do to correct thyroid hormone?
Reducing the antibody titer in itself is not advisable. Correction of thyroid-type diseases that lead to increased enzyme levels. After treatment, the concentration will decrease on its own.
Medicines
In the treatment of pathologies that cause an increase in the level of AT-TPO, the following is used:
- Graves' disease - Propicil, Thiamazole, Tyrosol, Atenolol. Analogues and antagonists of thyroid hormones, antithyroid drugs block thyroid peroxidase, the transition of iodine to the active type. Peripheral transformations of the thyroid gland are inhibited. Eliminate or reduce the manifestations of thyrotoxicosis and the risk of goiter.
- AIT (autoimmune thyroiditis). With the development of hypothyroidism (the last stage of the disease), treatment is carried out with drugs based on levothyroxine - Euthyrox, L-thyroxine. Hormone-containing drugs for systemic use in diseases of the thyroid gland belong to the group of steroid drugs. Synthetic levothyroxine has the same effects as hormones produced by the human thyroid gland.
- Thyroid cancer. They use drugs for intravenous and intramuscular administration: Myomycin, Bleomycin, Caprelsa. Antitumor agents act on the tumor systemically and suppress the development of neoplasms.
Propycil is prescribed for Besedova disease
To increase antibody levels, medications are not used.
Treatment with folk remedies
Folk remedies can complement basic hormonal therapy in the treatment of thyroid diseases.
Remedies against hypothyroidism:
- Prepare a tincture of May lily of the valley . Place dried flowers in a bottle 2/3 of the way up, add 15 percent alcohol, leave for 7 days in a warm place, shaking regularly. Then use every day before meals, starting with 5 drops, increasing to half a teaspoon over two weeks. Course – 3 months.
- Take 100 g of dry seaweed, chop it, pour in the same amount of boiling water . When the mixture has cooled, add 120 g of low-fat cottage cheese, 6 pieces of walnuts minced, 2 tbsp. l. fat sour cream. Mix everything, close the lid tightly and refrigerate. This mixture must be eaten during the day in 2-3 doses. Use every other day for 1 month.
- Squeeze the juice from beets, potatoes, carrots, take equal parts of the juice with a volume of 200 ml . Take 50 ml 3 times a day before meals for 40–50 days.
For hypothyroidism, prepare a tincture of lily of the valley
In the treatment of thyroiditis use:
- Take 2 tbsp. l. dry crushed lemongrass leaves, pour 100 ml of 70% alcohol . Leave for 14 days in a dark place, shake the contents of the bottle periodically. Then strain and take 20 drops 1 hour before meals, diluting with water. The course of treatment is up to 30 days.
- Take 100 g of sea buckthorn fruit, 175 g of celery, half a lemon. Squeeze the juice from this raw material, mix, divide into 2 parts and drink in the morning and evening half an hour before meals. The treatment is long-term, at least 1 year, during which you need to take seven-day breaks every 2 months.
For hyperthyroidism - excessive production of thyroid hormones by the thyroid gland - use:
- Take 30 g of white mistletoe, calendula flowers, yarrow, wild rosemary and celandine, 50 g of thyme, rose hips, peony leaves, 60 g of cinquefoil . Grind the ingredients, mix, then 0.5 tsp. Brew the mixture in half a liter of boiling water, wait 30 minutes. Drink 100 ml a few minutes before meals for 2 months.
- Mix the dried ingredients - hawthorn flowers, sweet clover, sparrow . Take 1 part of this mixture and add 5 parts of zyuznik herb. 1 tbsp. l. pour 200 ml of boiling water, then boil the infusion for 20 minutes over low heat, leave for 1 hour, pour boiled water to 200 ml. Half an hour before each meal, take 70 ml for 2 months.
Traditional recipes for improving the functioning of the thyroid gland are selected individually by the attending physician. They cannot be basic therapy, but only complement the main treatment.