C-reactive protein (CRP) is a blood plasma protein that belongs to the acute phase of inflammation. It is involved in the processes of neutralization and elimination of various infectious agents, and is also a stimulator of the development of the inflammatory response as a mechanism of defense of the body. C-reactive protein on the surface of a foreign cell combines with specific molecules, proteins released from tissues damaged by bacterial toxins.
During normal functioning of the body, a certain (minimal) amount of C-reactive protein constantly circulates in the blood. This protein is produced primarily by the liver, as well as the inner lining of the arteries. When foreign microorganisms (bacteria) enter the body or as a result of the death of one’s own tissues, its concentration increases significantly. C-reactive protein levels increase hundreds of times as a result of severe trauma, severe inflammatory reactions, bacterial infections, major surgery, or in the presence of malignancy.
What does a C-reactive protein test show? A CRP blood test indicates the activity of reactive protein and the presence of an inflammatory process in the body.
At the Yusupov Hospital, patients are provided with effective, qualified medical care. Doctors are interested in the speedy recovery of patients and the complete restoration of lost functions. The rheumatologists of the department achieve significant positive changes in the physical condition of patients who have serious diseases, this applies to rheumatoid processes, in which the level of C-reactive protein increases. In the Yusupov Hospital's own laboratory, you can take any tests, such as C-reactive protein, and get quick results.
DRR for Covid-19
The level of C-reactive protein during coronavirus is one of the key laboratory indicators that require medical monitoring in moderate and severe forms of infection. It must also be determined in patients in critical condition.
It is C-reactive protein (C is our letter C) that is the main marker of lung damage, growing as the severity of the infectious process and the scale of inflammatory changes increase.
The level of CRP must be determined in case of difficulty breathing, when the number of breaths is ≥ 22/min, and saturation
Saturation is measured with a special device - a pulse oximeter.
Important blood indicators for coronavirus
Any disease is accompanied by changes in the blood. They are both quantitative (the concentration of individual cells in the blood changes) and qualitative (changes affect the blood cells themselves). When a blood test is done for coronavirus in a person, the indicators taken into account by doctors may differ depending on the patient’s condition and the presence of chronic diseases. However, in order to assess the patient’s condition caused directly by the presence of COVID-19 in the body, attention is often paid to the following parameters:
- leukocyte formula;
- hemoglobin level;
- presence of blood clotting factors;
- oxygen saturation in the blood.
Norm
The normal value of C-reactive protein does not exceed 5 mg/l. This is a universal value that does not depend on age or gender. In newborns it should not rise more than 0.15 mg/l.
If CRP is elevated, it means that inflammation is developing in the body, the intensity of which is indicated by the degree of this increase.
Thanks to many years of clinical research and the introduction of high-tech techniques, scientists have derived another parameter - the so-called “basic CRP value”. Its level makes it possible to assess how high the risk of damage to the cardiovascular system is in a person.
Note that this risk can be determined even in the absence of an inflammatory reaction. The norm for the basic value of CRP is ≤ 1 mg/l.
For the most accurate results, it is recommended to take the C-reactive protein test in the same laboratory, since different clinics may use different methods:
- ELISA – enzyme-linked immunosorbent assay;
- RID – radial immunodiffusion method;
Nephelometry, based on the intensity of the light flux scattered by suspended particles of matter.
If repeated tests are done using other methods, the interpretation of the results may be inaccurate.
How to diagnose coronavirus
When answering the question of what a general blood test shows for coronavirus, it should be noted that it can only be used to diagnose the presence of an inflammatory process and its severity. The cause of the disease can be identified using serological reactions - enzyme immunoassay for antibodies to covid-19.
When conducting a study, it is possible to identify and also evaluate the amount of specific proteins in the blood - immunoglobulins.
- Immunoglobulins M. They indicate an acute course of coronavirus infection. They begin to be produced from the 7th day of illness and are found in the blood up to 3-4 weeks from the onset of the disease.
- Immunoglobulins class G. They begin to be produced after 14 days of coronavirus infection and remain in the blood, according to various sources, for 4-6 months. They provide immunity against infection.
If immunoglobulins M are detected in the blood in the absence of G, an acute course of the disease is diagnosed. The presence of antibodies of both classes indicates that the patient has been ill for more than 2 weeks or has entered a period of recovery. The presence of class G antibodies indicates that the subject was ill with coronavirus in the period from 1 to 6 months before the study.
In other infectious diseases, such immunoglobulins are also detected after routine vaccination.
For testing, venous blood is used, which should be taken in the morning on an empty stomach. The result of the study becomes known within 1-2 days.
What blood test shows coronavirus? To confirm the diagnosis, if a high titer of immunoglobulin M is detected, it is necessary to conduct PCR diagnostics. This method allows you to detect genetic material (RNA viruses) in a smear from the nasopharynx and oropharynx and determine whether the patient is a dangerous virus excretor for others. In some patients, the virus is present on the mucous membranes for several days; in others, fragments of microorganisms can be detected within several months.
To diagnose a coronavirus infection, determine the severity of its course, and also assess the general condition of the body, you should undergo a comprehensive study, including a general blood test, biochemistry, coagulogram, serological studies and polymerase chain reaction.
Who is the analysis for?
A test for C-reactive protein is mandatory when a patient is admitted to hospital and Covid-19 is diagnosed as at least moderately severe. The analysis is then repeated as necessary.
The results are interpreted according to the following values:
If a significant decrease in CRP levels is not observed while taking antibiotics, then the risk of death is extremely high.
The production of C-reactive protein begins to increase in the first 5 hours after infection and reaches its peak by 2-3 days of illness.
A more detailed breakdown of the analysis results looks like this (mg/l):
- negative –
- weakly positive – 3-6;
- positive – 6-12;
- strongly positive – >12.
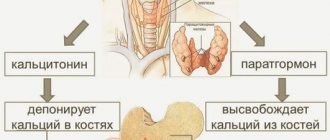
CRP and ESR
In addition to C-reactive protein, the inflammatory process also shows ESR - erythrocyte sedimentation rate. Both of these parameters increase in the early stages of diseases, but there is a significant difference between them.
First, CRP appears and disappears faster than ESR changes. Therefore, at the initial stages of diagnosis it is more informative.
Secondly, with adequate treatment, CRP decreases after about a week, while ESR falls no earlier than after 2-3 weeks.
Thirdly, the ESR indicator is influenced by the time of day, the composition of the blood plasma, the level of red blood cells, and gender (in women the ESR is almost always higher). The SRB parameter does not depend on these factors.
Therefore, analysis of C-reactive protein is a more accurate method of assessing the intensity of the inflammatory process than ESR. Therefore, it is carried out to establish a diagnosis, identify acute and chronic inflammation, as well as their activity. In addition, the results of this analysis allow us to evaluate the effectiveness of the therapy.
If CRP >60 mg/l or its increase threefold on days 7-14 of the disease, interleukin inhibitors - Tocilizumab, Sarilumab, Canakinumab - are necessarily prescribed. In severe cases, if a computed tomogram showed 2-3 degrees of lung damage, the following drugs are used:
- Tofacitinib;
- Baricitinib;
- Olokizumab;
- Levilimab.
To prescribe the funds listed in the list, you must comply with 2-3 points from the list below:
- CRP >30 mg/l;
- drop in saturation;
- temperature >38° for 3 days;
- white blood cells (WBS)
- lymphocytes
The level of C-reactive protein in the blood decreases in each patient at a different rate. The following are considered borderline indicators indicating the beginning of recovery:
- SRB
- saturation ≥ 95%;
- normal temperature is 36.6°.
With these parameters, the patient can be discharged from the hospital and transferred to outpatient treatment.
When to send for a biochemical blood test CRP
The doctor sends the patient a biochemical blood test for CRP in the following cases:
- Preventive examination of elderly patients.
- Determination of the likelihood of cardiovascular complications in patients with diabetes, atherosclerosis, and on hemodialysis.
- Examination of patients with hypertension, coronary heart disease to prevent possible complications: sudden cardiac death, stroke, myocardial infarction.
- Identification of complications after coronary bypass surgery.
- Assessing the risk of restenosis, recurrent myocardial infarction, and death after angioplasty in patients with acute coronary syndrome or exertional angina.
- Monitoring the effectiveness of prevention and treatment of cardiovascular complications using statins and acetylsalicylic acid (aspirin) in patients with cardiac problems.
- Collagenosis (to determine the effectiveness of therapy and the reactivity of the process).
- Monitoring the effectiveness of treatment of bacterial infections (for example, meningitis, neonatal sepsis) with antibacterial drugs.
- Monitoring the effectiveness of treatment of chronic diseases (amyloidosis).
- Neoplasms.
- Acute infectious diseases.
Features of C-reactive protein in old age
CRP levels in older people may increase due to age-related changes and concomitant diseases. One of the reasons is dementia, in which there is a lot of C-reactive protein.
Senile dementia most often develops with generalized - general - inflammation associated with vascular atherosclerosis, high concentrations of triglycerides (fats) and low-density lipoproteins.
In addition, when biological processes caused by the change of day and night (circadian rhythms) are disrupted and the lack of night sleep in the blood increases the content of substances that cause inflammation. At the same time, the level of C-reactive protein also increases.
An increase in CRP is characteristic of hypertension against the background of vasoconstriction due to cholesterol deposits, as well as obesity. A stroke is often a complication of atherosclerosis, which is accompanied by inflammation of the vascular wall, so immediately after the attack there is a sharp release of C-reactive protein into the blood.
One of the reasons for increased CRP may be periodontal disease - inflammation of the gums. Moreover, the higher its level, the more severe the degree of periodontal disease.
Increased concentrations of CRP accompany inflammatory bowel pathologies associated with poor diet and unhealthy lifestyle, as well as Crohn's disease and ulcerative colitis.
Indications for use
Most often, determination of the amount of reactive protein is prescribed for:
- Calculation of the risks of heart and vascular pathologies.
- After clinical examination of elderly patients.
- Postoperative period.
- Assessing the effectiveness of drug therapy.
- Diagnosis of autoimmune and rheumatic diseases.
- Suspicion of a tumor.
- Infectious diseases.
Laboratory testing of CRP is usually prescribed for acute inflammatory diseases of an infectious nature. It also helps in identifying pathologies of an autoimmune and rheumatic nature. It is prescribed for suspected tumors and cancer.
The role of CRP in the body and possible reasons for the increase
C-reactive protein is a link between antigens and immune cells. When foreign agents enter the body - viruses, bacteria, fragments of damaged cells - the production of CRP starts in the liver. Its task is to recognize the enemy “profile” and activate the immune response.
This mechanism operates in a number of pathologies, including:
- autoimmune – amyloidosis, rheumatism, systemic lupus erythematosus;
- infectious – blood poisoning (sepsis), meningitis, pneumonia, chlamydia, mycoplasma;
- oncological – carcinoma, melanoma, leukemia;
- helminthic infestations – giardiasis, leishmaniasis, toxoplasmosis;
- necrotic - pancreatic necrosis, rejection of a donor organ or tissue, asthma with lung damage, heart attack;
- rupture of the membranes during pregnancy, threatening miscarriage.
The culprit behind the inflammation has been found: the coronavirus S protein
Scientists in molecular biology studied the mechanism of the inflammatory process when Sars-CoV-2 enters the body and identified the special role of protein S. It is severe tissue damage (mainly lung) that is one of the most dangerous complications of coronavirus infection, which can lead to death.
The study found that the main part of the coronavirus S-protein, or its entire molecule, can cause interstitial damage, directly provoking inflammation.
This conclusion was made by a group of scientists led by P. Wark from the University of Newcastle. It included experts from China and Australia. The results of the experiment were published in the bioRxiv electronic library.
It turned out that the Sars-CoV-2 S protein has the ability to change the functioning of cells and force them to synthesize large quantities of signaling molecules that create conditions for inflammatory processes.
Previously, the medical community considered these inflammatory reactions to be the result of an overactive immune system overreacting to the coronavirus. But Wark and his team's discovery suggested that the culprit in the excess immune response was the coronavirus S protein.
Scientists plan to use the information obtained in the treatment of Covid-19 and test a number of drugs for oncology. Perhaps they will be able to neutralize S-protein viral molecules.
Coronavirus S-protein as a basis for vaccines
Another joint group of scientists from the University of Texas and the US National Institute of Allergy and Infectious Diseases, led by D. McLillan, obtained encouraging results. An article in the scientific journal Science describes in detail the three-dimensional structure of the S protein, which is a key element of the “Crown” of Covid-19.
S proteins are located on the surface of virions - viral particles. They extend from it like rays or needles, which is why they are called Spike. It is these proteins that are attacked by antibodies synthesized by the donor organism.
And the coronavirus itself needs S-proteins to infect cells. Their outer surface is almost no different from molecules familiar to cells, which allows the harmful microbe to easily connect with the corresponding receptors on the membranes and penetrate inside. This is precisely the mechanism of interaction of coronavirus proteins with the angiotensin-converting protein ACE 2.
Using cryo-EM - cryogenic electron microscopy - scientists saw the three-dimensional shape of the surface of the S-protein with a resolution of up to 3.5 A and found that the protein changes the spatial arrangement of atoms inside the molecule: when preparing for infection, it has one shape, and after binding to the target cell – another.
McLillan and his colleagues studied the properties of the first molecule, before its transformation, and found that the region of the protein that connects to the ACE 2 enzyme has increased affinity, that is, it can easily and firmly bind to cells, and therefore quickly spread throughout the body.
Knowledge of the precise structure and properties of the S protein allows us to see new opportunities for creating effective vaccines and antibodies. It is possible that a vaccine can even be obtained directly from the coronavirus S-protein, simply by modifying it. And then the formidable infection will finally become a target itself.