Diaskintest® (tuberculosis allergen recombinant in standard dilution) is an innovative intradermal diagnostic test, which is a recombinant protein containing two interconnected antigens - ESAT6 and CFP10, characteristic of pathogenic strains of mycobacterium tuberculosis (Mycobacterium tuberculosis)1. These antigens are absent in the vaccine strain Mycobacterium bovis BCG and in most non-tuberculous mycobacteria, therefore Diaskintest® causes an immune reaction only to Mycobacterium tuberculosis and does not give a reaction associated with BCG vaccination. Thanks to these qualities, Diaskintest® has almost 100% sensitivity and specificity2, minimizing the likelihood of developing false-positive reactions, which are observed in 40–60% of cases when using the traditional intradermal tuberculin test (Mantoux test)3. The technique for performing the Diaskintest and recording the results is identical to the Mantoux test with tuberculin4.
In Russia, the use of Diaskintest was approved in 2009 by Order of the Ministry of Health of the Russian Federation 855 of October 29, 20094
Since 2021, the use of Diaskintest in screening for tuberculosis in children over 7 years of age and adolescents is regulated by Order of the Russian Ministry of Health No. 124n dated March 21, 20215.
Diaskintest is highly sensitive and highly informative: it allows you to exclude false-positive reactions that occur during the Mantoux test in vaccinated individuals (post-vaccination immunity). According to various estimates and in different regions of Russia, the sensitivity of Diaskintest is about 96%.
Diaskintest - what is it
For reference. Diaskintest is a drug that is used to test for immunity to Mycobacterium tuberculosis.
The short name of the drug is also used - Diaskin. The test itself with this drug is also called Diaskintest. The drug is a diagnosticum that contains two antigens that are part of Mycobacterium tuberculosis. Based on these antigens, the human immune system recognizes Koch bacilli and starts the process of their destruction.
For reference. In order for Diaskin to be a pure preparation, without foreign impurities, antigens are specially grown. To do this, the genetic material of Mycobacterium tuberculosis is introduced into the colonies of non-pathogenic bacteria of the human body - Escherichia coli.
E. coli begin to express antigens characteristic of mycobacteria. For the diagnostic test, only two antigens were selected, found in “wild” strains of Koch bacilli, which cause the disease.
A protein extract is prepared from colonies of E. coli. In this case, only two antigens inherent specifically to tuberculous mycobacteria are removed. The diagnosticum is placed in bottles in such a way that 0.1 ml contains one diagnostic dose of antigens.
Result reliability indicators
For reference. Any laboratory research method has two main indicators of reliability: sensitivity and specificity. Both indicators are intensive, that is, they are calculated per 100 people who were tested.
The sensitivity indicator gives an idea of how many people who are immune to mycobacterium tuberculosis will have a negative diaskintest. These are the so-called “false negative results”.
For Diaskintest, the maximum number of such results is 12 per 100 samples. These people will have a negative test, despite the presence of immunity.
For reference. False negative results occur in cases where the immune response was insufficient to cause a reaction to the administered diagnosticum.
The specificity indicator gives an idea of how many people who do not have immunity to Mycobacterium tuberculosis will have a positive diaskintest. These are the so-called “false positive” values.
The maximum number for Diaskintest is 2 per 100 samples. They arise due to the fact that some microorganisms have antigens similar to those of the Koch bacillus. Diaskintest rarely recognizes them as tuberculosis, but sometimes such errors occur.
For reference. The sensitivity and specificity indicators of Diaskintest are better than those of the Mantoux test. This indicates the greater reliability of the method in comparison with other methods of laboratory diagnostics.
Purpose of Diaskintest
Attention. The only purpose of the diaskintest is to determine the presence or absence of immunity to mycobacterium tuberculosis. This method does not diagnose active tuberculosis. This statement is especially true for adults and children who have previously been in contact with Mycobacterium tuberculosis.
The fact is that when it first enters the body, the Koch bacillus causes primary tuberculosis. In the vast majority of children, and the first contact occurs precisely in childhood, primary tuberculosis is asymptomatic or has a flu-like course.
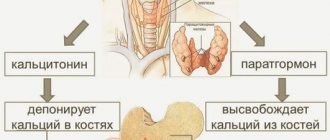
Despite the mild course of the disease, the body reacts to mycobacteria as it does to any other infectious agent. At the same time, specific immune cells are produced - T-lymphocytes. They prevent Koch bacilli from spreading throughout the body and protect a person from re-infection.
For reference. T lymphocytes trained to recognize and destroy Koch bacilli remain in the body for life. At the same time, mycobacteria that are in the area of the primary focus in an inactive state can remain in the body for life. This process is called non-sterile immunity.
The purpose of diaskintest is to identify T-lymphocytes that appear upon contact with mycobacteria.
The principle of action of the drug is very simple - an antigen (also known as an allergen), which is contained in Mycobacterium tuberculosis, is injected intradermally. If there is an inflammatory reaction at the injection site, then the immune system has reacted to tuberculin.
If you react, it means you have immunity to Koch bacilli, the T-lymphocytes have already been trained, and the primary infection has already occurred. This information is most relevant for children.
Diaskintest is performed for adults if they have active tuberculosis. If immunity is intact, there should be no secondary infection.
If a person gets sick with tuberculosis again, it means his immunity has not coped with its task. This can be a consequence of immunodeficiency or infection with overly aggressive strains of tuberculosis.
For reference. In this case, diaskintest is necessary in order to understand whether this patient has immunity to mycobacteria and how much it is reduced. Lack of immunity is a poor prognostic sign.
Questionable situations with tests and their solutions
There are cases when the DST result is negative, but at the same time the mantoux norm is positive. Don’t think that there is 100% no infection. A month later the picture changes dramatically. DST simultaneously with mantou level out into positive ones. The patient begins to be treated. A month later, the picture changes again and the DST becomes negative. With such “wandering” indicators, it is recommended to do PCR diagnostics.
PCR analysis reveals all bacteria hidden in the body. It works at the level of gene changes that occur in the body under the influence of microorganisms. But the PCR procedure costs from 3,000 rubles, in large cities it is even more expensive. The free program does not include examination. Only after the PCR result can we say with certainty whether the patient is sick or healthy.
Here's what experts say about the test:
Whatever the result, it is worth assessing the situation soberly. Even with tuberculosis, with steam care, patients live happily ever after.
Diaskintest is carried out for children as a preventive voluntary-compulsory examination for tuberculosis. Each parent has the right to refuse to have it, however, this will lead to a large number of disputes with the pediatrician and may block the child’s access to some children’s institutions. In addition, refusal to prevent tuberculosis is impractical, since the possible risk of the disease is many times greater than the time spent on the test.
Many parents in wealthy families believe that since their child is not at risk and is well cared for, he cannot become infected with deadly tuberculosis. However, they are cruelly mistaken, which sometimes costs the life of their baby.
The tuberculosis bacterium is an extremely tenacious microorganism that, surviving outside the host for a long time, can enter a healthy person even along with dust if the patient spits sputum on the ground and it dries. Also “popular” is the airborne route of infection with microscopic particles of saliva from patients in the air.
There are a lot of tuberculosis patients, even with modern medicine: tuberculosis is very poorly treated and remains genetically resistant to the drugs with which it has come into contact.
You can become infected with tuberculosis from any random passerby, in public places, especially on public transport or when using common household items. Tuberculosis is transmitted not only by airborne droplets, but also by contact through objects, and it also affects other organs of the body in addition to the lungs: eyes, skin, bones, liver, muscles, etc. Many patients infect other people without even suspecting that themselves are sick, since until the moment when it begins to threaten the patient’s life, this illness can be completely asymptomatic.
The increased survivability of tuberculosis is due to its ability to be preserved for a long time, therefore, a dormant or inactive form of tuberculosis is distinguished, which is present in from thirty to ninety percent of the population, depending on the region, without causing harm, but at the same time can be transmitted from mother to child during pregnancy and can wake up, for example, with a strong drop in immunity. It is this dormant form in the blood that determines manta, which is used to identify a person’s tendency to this disease.
Tuberculosis is an extremely contagious and life-threatening disease that leaves behind many serious complications. Also, consumption is very difficult to treat. It is easiest to defeat tuberculosis in the early stages, when it has no symptoms and is almost undetectable.
Indications and contraindications for the procedure
Diaskintest at school is carried out regularly for all children once a year. Regardless of whether a child has signs of tuberculosis or not, he should be diagnosed.
For reference. This is done in order to identify the turn of the tuberculin test - the moment of infection with Mycobacterium tuberculosis. In this case, there are no indications for the test; it is simply a planned mandatory procedure.
This is done in those countries where Diaskintest has replaced the Mantoux test, including the Russian Federation.
In some cases, there is a need for an unscheduled diaskintest. In children, indications for it are:
- prolonged persistent cough;
- prolonged low-grade fever;
- symptoms of pneumonia in the absence of effect from broad-spectrum antibiotics;
- contact with a patient with tuberculosis (being in an epidemic focus).
Thus, the indication for performing a diaskintest is a suspicion of infection with Mycobacterium tuberculosis. In addition, in those countries where the Mantoux test is still used, Diaskintest is necessary for differential diagnosis between a post-vaccination reaction and primary tuberculosis.
The fact is that Mantoux can be positive both after administration of the BCG vaccine and during infection with mycobacteria. Diaskintest reacts only to “wild” strains.
For reference. If the Mantoux test is positive and the Diaskintest is negative, then the child remains immune after the vaccine.
In adults, it is impossible to detect active tuberculosis using Diaskintest. The result should normally be positive, since all adults in epidemically unfavorable regions are infected with Koch bacilli.
Diaskintest has rather a prognostic value. So, if a patient is diagnosed with tuberculosis and there is a violent reaction to the test, the prognosis is favorable. This means that the immune system has mobilized its forces to fight this infection.
For reference. If tuberculosis is present, but the reaction is weak or absent, then the prognosis is unfavorable. This means that the immune system is suppressed and the body itself cannot cope with the infection.
This rule does not apply to adults who come from epidemic-friendly areas. They may not have immunity to mycobacteria due to lack of contact with sick people.
Attention. In adults, Diaskintest is necessarily used in combination with other methods of diagnosing tuberculosis and is not the primary method.
There are a number of contraindications, in the presence of which Diaskintest is not performed either planned or urgently according to indications.
Test specifics
Tuberculosis is a socially significant disease that is caused by an infectious agent - Koch's bacillus. Most often, tuberculosis affects the lungs, less often other organs (kidneys, skin, bones, eyes).
Tuberculosis can occur in a latent (latent) form, when there are no external visible symptoms of the disease and the diagnosis can be made only based on the result of an immunological test.
Tuberculosis is widespread among the population of different countries. Previously, it was believed that only socially disadvantaged sections of the population were susceptible to tuberculosis. However, observations in recent years indicate the opposite. Anyone can become infected with tuberculosis, regardless of social status and material wealth.
So, the diagnosis of tuberculosis involves:
- bacteriological examination of a smear obtained from sputum;
- X-ray examination of the lungs and other organs;
- fluorographic examination;
- immunological tests (Mantoux test, Diaskintest).
Bacteriological examination of a sputum smear is not always informative, especially in the early stages, and requires compliance with certain rules for the collection and storage of sputum. The result of x-ray and fluorographic examination must be differentiated from other diseases that give a similar x-ray picture.
For example, focal lesions of the lungs due to pneumonia or cancer can easily be confused with foci of tuberculosis. A foreign body in the lungs can also give a similar x-ray picture.
The Mantoux reaction also has a fairly large error. Among all the above methods for diagnosing tuberculosis, the Diaskintest test is by far the most informative and reliable.
The drug is administered exclusively intradermally with a special tuberculin syringe with a thin short needle with an oblique cut. The test is carried out in a medical institution by a specially trained specialist (in the vaccination room of the clinic) in compliance with all the rules of asepsis and antiseptics. The drug is administered against the background of complete health.
Administration of the drug is not allowed in the following cases:
- epilepsy;
- acute or exacerbation of chronic infectious diseases;
- somatic diseases in the acute period;
- extensive skin lesions due to dermatological diseases;
- complicated allergic history.
The test is performed with caution and only in case of urgent need for women during pregnancy and breastfeeding. The test result is assessed by a phthisiatrician or a nurse in a phthisiological or vaccination office.
Frequency of Diaskintest
For reference. Healthy children are supposed to undergo Diaskintest once a year. This is provided that they have received vaccination.
The BCG vaccine is administered to a child at birth and at the age of seven. Vaccinated children are protected against Mycobacterium tuberculosis for several years after the vaccine is administered.
However, there are categories of children who were not given the BCG vaccine for various reasons. Such children are more likely to develop tuberculosis, and the risk of a severe course of the disease is high. For this category of children, Diaskintest is carried out twice a year as planned.
For adults, Diaskintest is not a mandatory screening method. It is important for this population group to undergo fluorographic examination once a year.
Diaskintest is carried out exclusively according to indications when an active form of tuberculosis is suspected.
For reference. If necessary, Diaskintest can be used an unlimited number of times. In this case, you should alternate between the right and left hands and avoid inserting into the same place. It is recommended to repeat the test no more than once every 2-3 months due to the risk of local allergies.
Side effects of Diaskintest
Only rare cases of side effects are known. Their low frequency and low risk of occurrence are associated with the method of drug administration.
The test is carried out intradermally, so the substance does not enter the systemic bloodstream.
For reference. The most common side effect is a nonspecific allergic reaction at the injection site. Allergy is associated with individual intolerance to the components of the drug.
In rare cases, side effects may occur such as:
- headache,
- low-grade fever,
- increased blood pressure,
- increased fatigue.
Even less common are local manifestations in the form of subcutaneous hematomas or pustules. As a rule, adverse reactions are associated with a violation of the test technique. For example, they can occur if an allergic history is not collected, the skin is incorrectly treated with an antiseptic, or the nurse gives a subcutaneous injection instead of an intradermal one, and the drug gets into the blood.
Is Diaskintest dangerous?
There are several myths associated with tuberculin diagnostics. The most unfounded and frightening of them is the danger of contracting tuberculosis due to the administration of the drug. In fact, this is impossible even if the injection technique was violated.
The fact is that Diaskintest is a sterile drug. It contains absolutely no microorganisms.
For reference. In order for an immune reaction to occur, the introduction of mycobacterial antigen proteins is sufficient. In this case, the tuberculosis bacilli themselves are not needed. The drug contains only two antigens, which by themselves cannot cause disease.
Moreover, Diaskintest is administered intradermally. All drugs with this method of administration do not enter the bloodstream. This means that Diaskintest can only cause a local reaction.
The only danger in this case is the occurrence of a nonspecific allergy to a foreign protein. But, as a rule, it is local in nature and does not pose a threat to the body.
Which is better - mantu or diaskintest
For reference. At the moment, there are two main methods for determining immunity to tuberculosis using antigen diagnostics - Diaskintest and Mantoux test. Each of them has its positive and negative sides.
The Mantoux test is performed using a protein extract made from several strains of mycobacteria. The drug used for the test contains proteins that are present in both “wild” and vaccine strains.
The Mantoux test causes an immune reaction both during infection with tuberculosis and after the BCG vaccine. In addition, it may react to the presence of other mycobacteria that do not cause tuberculosis.
Thus, the Mantoux test has less specificity than the Diaskintest. When performing it, it is difficult to distinguish post-vaccination immunity from that acquired during primary tuberculosis. These are the main disadvantages of the Mantoux test.
For reference. Diaskintest is made by growing strains of bacteria that express only two Koch bacilli antigens.
These antigens are found in “wild” strains, but are absent in vaccine strains. Diaskintest causes an immune reaction only in those infected with tuberculosis.
There are no post-vaccination reactions, no cross-reactions with other mycobacteria. All these are the benefits of Diaskin.
The disadvantage is that the antigens of this test do not appear immediately after infection with tuberculosis. That is, when a primary outbreak occurs, the Mantoux test will respond faster than the Diaskintest.
In many countries, Diaskintest is used as the first-line method for diagnosing primary tuberculosis.
Attention. However, it is worth remembering that this method does not recognize immunity that occurs immediately after infection. In addition, the Mantoux test is still used to determine the strength of immunity after the BCG vaccine, which Diaskintest cannot do.
What does the solution consist of?
Diaskintest is injected subcutaneously into the forearm. The body reacts to mycobacterial proteins. The method allows you to determine whether a person is infected with tuberculosis. But this method cannot distinguish whether the patient is a carrier of bacteria or is developing a disease. If the test is positive and there are no symptoms, additional examination methods are prescribed.
Diaskintest includes:
- saline;
- artificial proteins of tuberculosis bacteria CFP10 and ESAT6;
- potassium and sodium salts;
- preservative phenol, in an amount of 0.25 mg, which is a safe dose;
- stabilizer polysorbate 80.
Preparation for the procedure
Diaskintest is a procedure that can almost always be performed without any specific preparation.
Exceptions include several categories of the population.
Attention. First of all, people who suffer from allergies deserve special attention. At least a week before the test, they need to start taking antihistamines in regular dosages.
This will not affect the test result, but will prevent the development of an allergic reaction. If your child has seasonal allergies, the routine test should be postponed until winter.
Another category of children who need to select the time for administering the test according to the calendar are children who have reached the age of vaccination.
Attention. Regardless of what vaccination the child is given, Diaskintest cannot be performed for another month after it. If a child is vaccinated with BCG, Diaskintest cannot be administered less than a month before and earlier than a month after vaccination.
Adults should not drink any alcoholic beverages less than 72 hours before the test. In addition, you should avoid alcohol until the test results are assessed.
Before carrying out the Diaskintest, it is necessary to carry out thermometry. If the result of thermometry is not explained by the possible presence of tuberculosis and an acute respiratory infection cannot be excluded, the diaskintest should be postponed until recovery.
Is it allowed to wet the sample?
After the injection, you must follow some rules to avoid getting an incorrect result. The site where the test for tuberculosis was taken should not be scratched, because there is a high probability of infecting the wound and not getting the correct result.
Wetting Diaskintest is not recommended for people with sensitive skin and prone to allergic reactions.
This may cause a false positive result. You must adhere to this rule until the doctor examines the injection site.
For everyone else, you can wet your forearm after the test, but do not rub it with a washcloth, scrub or other means that can damage the skin. This diagnostic method does not provide for other restrictions on diet and lifestyle.
Which institutions conduct Diaskintest?
Diaskintest is carried out for healthy children in preschool institutions, schools, boarding schools, orphanages, and infant homes. All children attending organized children's groups undergo the procedure according to the preventive examination schedule.
For reference. Diaskintest is performed by specially trained medical personnel in manipulation rooms or a nurse’s office in an institution.
If the child does not attend the listed institutions or missed a general examination, the parents should take him to the local clinic to see the local pediatrician.
Algorithm for conducting diaskintest
The diagnosticum is administered by a specially trained nurse in the manipulation room. She sequentially performs the following actions:
- Checks the bottle with the drug for leaks, expiration date, evaluates the type of contents;
- Draws 0.2 ml of the drug from the bottle into a tuberculin syringe;
- Wipes the palmar surface of the middle third of the forearm with alcohol for antiseptic purposes;
- Injects 0.1 ml of the drug from a syringe into the middle third of the forearm strictly intradermally.
After this, the test itself is completed.
Attention. Results are assessed after 72 hours. The patient’s task is to protect the injection site from friction, contamination and chemicals for three days.
Is it possible to wet Diaskintest?
There is a myth that Diaskintest, like the Mantoux test, cannot be wetted with water.
In fact, after both tests, the papules do not react to water in any way. You can wet them with plain water, you can also take a shower. The main thing is to avoid friction, contact with soap, shower gels, creams and any other chemicals.
Attention. Before assessing the test result, you should not take a bath to avoid interaction with chemicals contained in the water.
You should also avoid visiting the sauna and swimming pool. If chemicals come into contact with the papule or if it is rubbed excessively, nonspecific inflammation may occur. The latter may be mistakenly regarded as a positive reaction to the diagnosticum.
Actions to take if an infection is detected
A positive result of the diaskintest (photo below) is a reason to refer the patient for a consultation with a phthisiatrician. The doctor will give you a referral for a general blood test. If the infection spreads in the blood, there will be a decrease in leukocytes and an increase in ESR. Tuberculosis develops asymptomatically up to 2 years.
During this period, the patient is not contagious, but when immunity declines, the disease becomes open. Therefore, the doctor must promptly determine the stage of development of the disease and prescribe treatment to prevent infection of other people.
Adults need to undergo fluorography to identify lesions in the lungs. For children, X-ray examination is recommended due to the lower radiation dose. If there are no clearly defined foci of inflammation in the images, an MRI of the lungs is required.
Diaskintest results
A reliable result can be obtained no earlier than 72 hours after the test.
To do this, carefully study the injection site of the drug. There may simply be an injection mark, a papule of different sizes, a vesicle or other elements. They can be located on a hyperemic or non-hyperemic background.
The diameter of all found morphological elements is measured with a ruler. The data is entered into an outpatient card or other medical document.
Possible results
The reaction to Diaskintest may vary. There are three main results of Diaskin:
- Negative - there are no traces at the site of drug administration, except for the mark of a syringe injection;
- Doubtful - there is slight redness around the injection site, level with the skin;
- Positive - at the injection site there are elements rising above the surface of the skin.
For reference. A positive result means that the body has responded to the administration of the diagnosticum. But this reaction also varies in severity.
There are several options for a positive result:
- Weak - at the injection site there is a nodule (papule) less than 5 mm in size;
- Moderate – nodule at the injection site from 6 to 9 mm;
- Pronounced – papule size from 10 to 15 mm;
- Hyperergic - the papule exceeds 15 mm in diameter or there is a papule of any diameter with pustules, vesicles, inflammation of the lymphoid system.
Evaluation of results
The absence of a reaction, that is, a negative result, means that there is no immunity to mycobacterium tuberculosis.
This reaction can occur in children who have not yet had primary tuberculosis. In adults, lack of contact with Koch bacilli is very unlikely. A negative result rather indicates immunosuppression.
Such a reaction is possible in HIV-infected people in the AIDS stage, in hematological patients, and in people receiving chemotherapy. At the same time, they may even have active tuberculosis, but a complete lack of reaction to it.
For reference. A questionable result is difficult to interpret. Perhaps immunity is just emerging, maybe it is not there, but the administration technique was violated or the patient exposed the hand to friction, and the reaction is not specific. This result cannot be reliably assessed, so the test is repeated. Repeated diaskintest is done at least after 2 months.
A positive result requires more detailed study. It means that there was contact with mycobacteria, a trace remained in the immune system. The main task is to determine whether there is active tuberculosis at the moment or whether an encounter with Koch bacilli occurred in the past and went unnoticed and the person is healthy.
Attention. In children and adults, positive diaskin has a different interpretation.
Change in reaction by day
The cellular component of immunity is responsible for protection against Mycobacterium tuberculosis. All reactions of this link are slow. This is the so-called “type four hypersensitivity”, also known as delayed hypersensitivity.
The response to the introduction of the allergen develops no earlier than 24 hours after the test.
If we also take into account that the volume of drug administration is very small, on the first day we can only expect the beginning of the development of the process.
For reference. The full reaction will only appear after 48-72 hours. Therefore, the result is assessed after three days. Then the reaction subsides and the papule, if there was one, disappears.
Allergic reactions
A nonspecific allergic reaction may develop to the administration of the drug. It reflects the immune response not to mycobacterial antigens, but simply to a foreign protein.
Attention. This reaction does not provide any information about immunity against Koch bacilli.
Nonspecific allergy occurs almost immediately after administration or after a few hours, accompanied by all signs of inflammation: redness, itching, increased local temperature. The reaction disappears after administration of antihistamines.
Hematoma at the injection site
A hematoma occurs when blood leaks into or under the skin. The mechanism of hematoma formation is early superficial capillary.
For reference. A hematoma cannot indicate the presence or absence of an immune response; as a result of Diaskin, it is not taken into account.
Therapy for lung disease
Treatment of tuberculosis lasts 6-8 months. During this time, depending on the stage of the disease, you must follow the doctor's recommendations. In severe cases, bed rest is required. If you are in average health, you should avoid physical activity and stress. As your condition improves, you can switch to normal mode.
The time it takes for recovery to occur depends on the patient’s immunity, the resistance of the mycobacterium to the prescribed drugs, and concomitant diseases.
First line anti-tuberculosis drugs include:
- Pyrazinamide - promotes lung recovery;
- Rifampicin - prevents infection of healthy tissues;
- Streptomycin – blocks bacterial proteins;
- Ethambutol - destroys Koch's bacillus.
At this stage, combining drugs can stop the development of the disease. The duration of treatment, frequency of administration and dose of medication are determined by a TB specialist based on the form of tuberculosis, previously prescribed treatment and the general condition of the patient.
In severe cases, surgical methods are used. They are necessary for complex forms of the disease and the development of complications. Surgery is resorted to in 25% of all cases of the disease. Lung bleeding is a life-threatening condition and requires immediate intervention.
Depending on the development of the disease, the surgeon removes part of the organ, a lobe, or the entire lung. Possibly, cutting off the destroyed area - cavities.
If left untreated, the mortality rate from tuberculosis reaches 50%. The risk increases in older people, HIV-infected people, and people with diabetes. During treatment, you should not take a break from taking medications.
It is not recommended to independently determine the positive or negative result of the diaskintest from photographs on the Internet. Additionally, during therapy, increased nutrition and vitamin intake are required. In the active stage of the disease, treatment occurs in an anti-tuberculosis dispensary.
Article design: Oleg Lozinsky
Interpretation of a positive result in children and adults
In a child and an adult, a positive result means the presence of an immune response to the introduction of Mycobacterium tuberculosis antigens. However, this should be interpreted differently.
For reference. In children, the first detected positive reaction is called a turn. The turn means that the body first encountered Koch bacilli and infection occurred.
The child has either already suffered primary tuberculosis, after which a persistent immune response remained, or is currently experiencing it. In order to identify the activity of the process, it is necessary to consult a specialist and conduct additional research methods.
For reference. In adults, the result should normally be positive.
The likelihood that a person came of age in an epidemically unfavorable place and did not encounter mycobacteria is very low. It is impossible to distinguish active tuberculosis from inactive tuberculosis using Diaskintest alone.
The strength of the reaction, as a rule, correlates with the activity of the process. The more pronounced the response to the antigen, the greater the chance that a person is currently suffering from tuberculosis, but a consultation with a TB specialist is still needed to make a diagnosis.
From the point of view of prognosis, it is better for a patient with tuberculosis if the immune response is pronounced.
Similar articles:
- What is excretory urography of the kidneys, how is it performed? Excretory urography is a research method. Let's look at the name of the method so that...
- What is FGDS of the stomach? How is FGDS of the stomach performed? In official medical terms, this is gastroscopy...
- Quantiferon test - new in the diagnosis of tuberculosis Quantiferon test for tuberculosis is a tube test using...
- How to carry out a breath test for Helicobacter The breath test allows you to literally within an hour without much discomfort...