TRICHINOSIS
(
trichinellosis
; synonym:
trichinosis, “puffy”
) - helminthiasis from among the nematodes, characterized by fever, muscle pain, facial swelling, skin rashes, eosinophilia, and in severe cases - damage to the myocardium, lungs, and central nervous system.
For the first time, Trichinella larvae were discovered in the muscles of a corpse by an Englishman. medical student J. Paget in 1835. The first observation of human T. with a fatal outcome was described by FA Zenker in 1860.
Geographical distribution
T. is ubiquitous in nature. In the last 20-30 years, the distribution of human T. incidence in the world has changed. The incidence has decreased significantly in Eastern European countries and the USA. Thanks to the improvement of the pig breeding system, T. is practically not registered in Romania, Hungary, and Bulgaria. A stable focus still remains in the east. parts of Poland. Individual diseases and outbreaks are recorded in northern Italy, on the island. Sicily, in France, Spain, the Netherlands. The incidence of trichinosis has increased in Asian countries, on the Pacific Islands, Mexico, and Chile. T.'s diseases began to be recorded in Africa. In Asia, the greatest prevalence of T. is noted in Lebanon; individual diseases are recorded in Iran, Iraq, and India; outbreaks of T. are observed in Indonesia, Thailand, and Laos.
In the USSR, T. has been registered in 65 species of wild animals. By 1978, the incidence of T. in pigs had sharply decreased. The incidence of trichinosis in the BSSR, which was the main focus of T. in our country, has decreased 38 times over the past 15 years. In connection with the development of the territories of the North and East of the country, the number of T. diseases in people who eat wild animal meat increased, so in 1975 in the RSFSR it accounted for up to 96% of all T. diseases, while in 1946-1967 - only 24.4%.
Etiology
The causative agent of T. is the nematode Trichinella spiralis (Owen, 1835). New species of trichinella, T. nativa (Britov, Boev, 1972) and T. nelsoni (Britov, Boev, 1972), identified in 1972 by S. N. Boev and V. A. Britov, were recognized by the International Commission on Trichinosis in 1980 varieties of T. spiralis.
Sexually mature Trichinella (females 1-3 mm long, males 1-2 mm long) live in the mucous membrane of the small intestine. Males die after fertilizing females; females stay in the small intestine for 3-4 weeks, with intense infestations - up to 5-6 weeks. On the 3rd day after invasion, females give birth to larvae, which spread throughout the body with the flow of lymph and blood and, penetrating under the sarcolemma of the striated muscles, settle in them. At 3-4 weeks after invasion, a capsule forms around the larvae. The encapsulated larva has an oval shape, size 0.5 X 0.2-0.6 XX 0.3 mm. The capsule is gradually impregnated with calcium salts, but the larvae remain viable for many years.
Cause of trichinosis
The cause of trichinosis is the consumption of meat contaminated with Trichinella larvae. The species that most often causes disease in humans is Trichinella spiralis
, found in pork meat.
Other Trichinella species, such as T. britovi
and
T. papuae
, can also cause disease.
After a person ingests the parasites, the larvae enter the small intestine, where they mature and reproduce. Their females then release larvae, which travel from the small intestine into the bloodstream and reach the muscles. Once in the muscles, the worms can live for a long period of time.
Epidemiology
The source of pathogens of invasion (see) for humans are pigs, wild boars, brown, black and polar bears, marine mammals (whales, walruses, seals), as well as horses and dogs. Human infection with T. occurs when eating untested raw, salted, smoked or insufficiently heat-treated meat, as well as lard and sausages. Domestic animals become infected by eating meat waste or the corpses of dead animals; wild animals become infected as a result of predation, as well as by eating animal carcasses. Marine animals become infected through water contaminated with the feces of carnivorous birds, which may contain undigested invasive Trichinella larvae.
Depending on the range of hosts, three types of T. foci are distinguished: natural, synanthropic and mixed. In natural foci (see Natural focality), the circulation of Trichinella is supported by food connections between wild animals of different species. In synanthropic foci, circulation of the pathogen occurs between domestic animals (pigs, cats, dogs) and synanthropic rodents (rats, mice). When the connection between natural and synanthropic foci is maintained, mixed, natural-synanthropic foci arise. This is facilitated by free grazing of pigs, feeding of hunting waste to domestic animals, etc.
An increase in the incidence of T. in synanthropic foci usually occurs in the autumn-winter period, which corresponds to the period of slaughter of pigs and procurement of meat products. T.'s diseases are usually group in nature.
Prevalence of trichinosis
Trichinosis in humans belongs to the category of biohelminthiases, as it is caused by parasitic worms - Trichinella. The disease is diagnosed in both animals and humans. The main animal species most often affected by trichinosis are: wolf, fox, bear, badger, wild boar. Domestic pigs are also susceptible to this type of helminthiasis. This usually happens when pigs graze freely, when the meat of dead animals and small rodents becomes available for them to eat.
Reasons for the widespread prevalence of trichinosis:
- The pathogen's good adaptability to high and low temperatures ensured its residence in many climatic zones;
- The human body is extremely susceptible to this disease;
- Group outbreaks of helminthiasis are not uncommon among members of one team or one family who have consumed meat with Trichinella;
- Repeated cases of infection occur due to unstable immunity formed after the initial invasion.
Trichinella are modified, new forms of nematodes that do not form a capsule appear, as well as species that parasitize birds.
Pathogenesis
There are three phases of disease development: enzymatic-toxic, immunological and immunopathological. The enzymatic-toxic phase of the disease is clinically detected only with intensive infection. During the process of penetration into the mucous membrane of the small intestine, the larvae secrete metabolites that have enzymatic, toxic, sensitizing effects, as well as the ability to suppress immune reactions. A specific sensitization of the body occurs. By the end of the 2nd and 3rd weeks, a sufficient amount of antibodies accumulates in the body, the immunosuppressive activity of intestinal trichinella weakens and a violent allergic reaction occurs (immunological phase), accompanied by impaired blood clotting, increased permeability of capillary walls, and tissue edema. Damage to internal organs and damage to c. n.s., systemic vasculitis, developing in the third, immunopathological, phase of the disease, is associated with damage to body cells by the resulting immune complexes (see Immunity).
Pathological anatomy
With moderately intense invasion, by the end of the first week after infection, female Trichinella are found in the small intestine (to a lesser extent in other parts of the gastrointestinal tract), partially immersed in the mucous membrane and hanging into the lumen. In the mucous membrane, there is acute inflammation with hemorrhages and desquamation of the villous epithelium, in the deeper layers of the intestinal wall there is infiltration of lymphoid cells, macrophages and leukocytes with an increasing content of eosinophils. With intense invasion, the inflammatory reaction in the mucous membrane develops in the first days, and sometimes even in the first hours after the invasion, spreading to all parts of the intestines and stomach. In this case, the process in the 2-3rd week can take on an ulcerative-necrotic character with bleeding and even perforation.
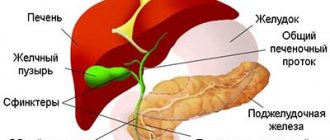
Rice. Microslides of striated muscles in trichinosis: a - encapsulating Trichinella larva (1), surrounded by an inflammatory infiltrate (2), spreading between the muscle fibers; hematoxylin-eosin staining; X200; b — encapsulated Trichinella larvae (dark areas in the area of the poles of the capsules are deposits of calcium salts); hematoxylin-eosin staining; x50.
In the 2nd week, with moderately intense invasion due to the migration of parasites in striated muscle tissue, myocardium, lungs, kidneys, and brain, rod-shaped larvae can be found, surrounded by inflammatory infiltrates containing a significant number of eosinophils, which leads to the development of myocarditis (see .), meningoencephalitis, pneumonia (see), etc. At the 3rd week after such an invasion, the larvae acquire an S-shape; they are surrounded by massive inflammatory infiltrates (Fig., a). The muscle fibers along the periphery of the larvae are thickened, with basophilic sarcoplasm, which has lost its cross-striations. In the myocardium, lungs, brain and other organs, granulomas form around the larvae, in which they undergo lysis and resorption. With intense invasion of the myocardium during these periods, pronounced focal-diffuse inflammatory infiltration and degenerative changes (trichinosis myocarditis) are noted. Similar changes are observed in the lungs and other organs. Systemic vasculitis is possible.
By the end of the 3rd and 4th weeks, with moderately intense and intense invasion, the inflammatory reaction in the wall of the small intestine and in the muscle tissue reaches its maximum development, and a sharp swelling of the mucous membrane of the small intestine is noted. The larvae in the muscles acquire a spiral shape, and a fibrous capsule is formed around them. Subsequently, the internal hyaline layer differentiates in the capsule, and calcium salts are deposited along the poles of the larva or diffusely in the capsule (Fig., b). Its complete calcification occurs after a few years.
5-6 weeks after infection, with intense invasion, inflammatory processes are replaced by dystrophic ones (dystrophic skin changes with hair loss, fatty liver). During recovery, inflammatory changes in organs and tissues, as a rule, disappear without a trace; elimination of changes associated with dystrophic processes occurs slowly - within 6-12 months.
The first signs and symptoms of trichinosis
Trichinosis in humans does not cause visible physical harm to the body. There are no changes in muscle tissue. The proteins that make up the parasite's body are harmful to health. They are very powerful allergens, foreign substances. The severe allergic reaction caused by them leads to damage to blood vessels and joints.
Incubation period of trichinosis. Lasts from 5 to 30 days, more often – 10-25 days. There are no symptoms of the disease. There is a pattern - the more severe the form of helminthiasis, the longer the latent (hidden) period.
High period. A long period of development of symptoms indicates the development of a severe form of trichinosis.
Mild and moderate form - symptoms:
- Hyperthermia. The temperature rises slightly, more than 37°C, the daily amplitude fluctuates within 1°C.
- Swelling on the body and limbs. Its cause is an allergic reaction to the introduction of a foreign protein. A characteristic symptom is a “frog face” in the patient.
- Muscle pain in the upper and lower extremities, muscles of the back, neck, eyes, pharynx, peritoneum. Intense pain begins in the calf muscles, affecting the cervical and chewing muscles. The pain intensifies with palpation and movement. They may begin to bother the patient from 1-3 days of introduction of the parasite into the body. The early appearance of muscle pain is a sign of a severe form of trichinosis.
Skin rash. Has different forms:
- In the form of allergic urticaria - pink blisters of various sizes that turn pale when pressed;
- Itchy blisters raised above the surface of the skin (utricar rash);
- Groups of plaques merging with each other (papular rash).
Complications in severe forms of trichinosis:
- Meningoencephalitis is an inflammation of the membranes of the brain.
- Pneumonia (eosinophilic pneumonia). The disease is caused by an increased concentration of eosinophils, products of an allergic reaction, in the lung tissue. Pleurisy and symptoms of bronchial asthma may develop.
- Myocarditis is inflammation of the myocardium due to allergies and excessive immune response. More often than other complications it causes death in patients.
- Nephritis is inflammation of the kidney tissue.
- Hepatitis is inflammation of the liver.
- Intense pain in the muscles leads to partial or complete impairment of mobility.
Mortality in severe forms of the disease is 10-30% of the total number of patients. The most common period for deaths to occur is 4-8 weeks from the onset of infection. In milder forms, patients recover after 5-6 weeks.
Symptoms of trichinosis depending on the stage of the disease
The manifestation of trichinosis at an early stage of infection depends on the concentration of parasites in the body. Further development of the disease depends on the spread of larvae in the muscles and the state of the patient’s immune system. The most severe complications of helminthiasis are associated with the body’s inadequate response to the introduction of a foreign protein into the body, and not to the activity of Trichinella and its larvae.
| Stage | Time since infection | Symptoms |
| Trichinosis invasion (penetration into the body) | 7 days | Trichinella larvae that enter the body orally are found in the small intestine. They become attached to the mucous membrane, causing inflammation of the intestinal wall. Within 55 days, the development of larvae into sexually mature individuals occurs in the small intestine, their fertilization and the emergence of a new generation of larvae. One female Trichinella produces up to one and a half thousand individuals. Symptoms of the early stage of trichinosis:
|
| Dissemination (spread of larvae throughout the body) | 2-4 week | The larvae begin their migration in the tissues of the body, penetrating into the muscles. They make their way from the intestines through blood and lymphatic vessels. After penetration into the blood, Trichinella larvae become attached to muscle fibers. They develop and grow, releasing allergens into the blood. Intoxication begins in the body, allergic reactions develop.
|
| Encapsulation stage | 6 weeks to 6 months after infection | During this period, tissue regeneration occurs. The larvae reach a size of 0.8 mm and take on a spiral shape. The foreign inclusion (larva) is fenced off by the capsule from the muscle tissue and stops its development. Trichinella toxins do not enter the body, the symptoms of the disease become less intense and gradually cease. The capsule becomes calcified, these salts can destroy the larva. Sometimes the Trichinella larva remains viable for up to 25 years, without affecting a person’s well-being. Symptoms of the regeneration phase:
Symptoms of the disease can be blurred and disguised as other diseases. There are three signs of trichinosis that are always recorded by a doctor after eating contaminated meat:
|
Symptoms of trichinosis in humans may be similar to manifestations of myositis, allergies, or infectious diseases. This picture leads to the fact that the patient does not suspect that he has helminthiasis.
Symptoms of trichinosis in children
To become infected, it is enough for a child to eat a small piece of meat with Trichinella weighing 10-15 g, which has not undergone full heat treatment. The latent period lasts from 5 to 45 days. The shorter this period, the more severe the form of the disease in the child.
- Symptoms at an early stage. Lasts 7-14 days, after recovery there are minor symptoms for 7-10 days.
- Hyperthermia up to 38.5°C:
- Slight puffiness of the face;
- Mild muscle pain;
- Swelling of the eyelids;
- Increase in eosinophil concentration by 10-12%.
- Symptoms are at a moderate stage. The acute period lasts up to 3 weeks, rehabilitation – 2-3 weeks after recovery.
- Hyperthermia up to 40°C, antipyretic drugs reduce it by no more than 1°C;
- Pain in muscles, joints, stomach and throat;
- Skin rash;
- Swelling of the face;
- Results of a general blood test: ESR is increased (above 17 mm/h), leukocytes are increased (up to 8.8·109/l), the concentration of eosinophils is increased to 25-40%.
- Symptoms at a severe stage. He is being treated in the infectious diseases department of the hospital; without therapy, the child may die.
- Hyperthermia up to 41°C;
- Enlarged liver and spleen;
- Central nervous system disorders: delirium, agitation, epileptic seizures;
- Attacks of severe abdominal pain;
- Diarrhea, nausea, vomiting;
- Severe muscle pain complicated by cramps;
- Subcutaneous hemorrhages and rash;
- General blood test indicators: Leukocytes up to 30-40x109/l; ESR up to 50-60 mm/h; eosinophil concentration up to 80 - 90%;
- Casts and proteins in the urine.
Treatment of trichinosis in children is carried out with anthelmintic drugs (Tiabendazole, Vermox) in accordance with the body weight and age of the child.
Drugs for the symptomatic treatment of trichinosis:
- Ibuprofen, Paracetamol - to reduce temperature, relieve pain;
- Cetrin, Loratadine - antihistamines to reduce intoxication and allergy symptoms;
- Papaverine, No-shpa - antispasmodics to reduce pain;
- Vitamins C and B to improve immunity.
Rehabilitation after illness is carried out with the help of massage sessions, baths with sea salt and medicinal herbs, and a complex of therapeutic exercises.
Immunity
After suffering from T., due to the presence of parasite larvae in the body of the recovered person, non-sterile immunity remains for life. Its intensity depends on the intensity of the invasion, the frequency of infection, the characteristics of the pathogen strains, and the constitutional characteristics of the patient’s body. The local residents of the north. districts of the USSR, Canada, USA, who constantly eat meat of wild animals that have not undergone heat treatment and are affected by T., the disease manifests itself clinically extremely rarely.
How to test meat for trichinosis?
Trichinella larvae are found in many animal species. Meat consumed by humans must undergo epidemic control. The most dangerous types of meat are pork, bear meat, and wild boar meat.
The appearance of contaminated meat is practically no different from that of a healthy carcass. The concentration of trichinella in the affected tissue reaches 200 pieces per 1 gram. Meat examination is carried out in a laboratory using a microscope. After analysis, a special mark is placed on the carcass.
Where can a test for trichinosis be done?
At the sanitary and epidemiological station or at the veterinary laboratory of the food market, samples are taken from the animal carcass. Samples of no more than 5 g are taken from areas of increased blood supply: masticatory muscles, tongue, intercostal muscles, diaphragm.
Even one detected trichinella is a reason for the destruction of the entire carcass, which from now on is considered unfit for food.
There is no veterinary laboratory control in spontaneous markets, during mass slaughter of livestock, or when eating hunting trophies. Unfortunately, Trichinella can be found in 30% of meat considered edible. Prevention of infection is thorough cooking of meat. This is especially true when eating game in regions where trichinosis is endemic.
Clinical picture
There are various forms of T.—from subclinical to severe with widespread lesions of internal organs. The duration of the incubation period is usually 10-25 days, with an erased and mild course of the disease - 4-5 weeks, with a severe course - 7-10 days (sometimes 1-3 days). All in. In latitudes, the incubation period of T. is described as up to 43 days in severe cases of the disease. When infested meat is repeatedly consumed in the prodromal period, liquid stool often appears, while there is no abdominal pain and the general condition of the patient is not disturbed.
In erased and mild forms, body temperature does not exceed 38-38.5°, the number of eosinophils is within 10-20%; the illness lasts 1-2 weeks. In moderate cases of T., the body temperature reaches 39-40°C within 2-3 weeks. gradually decreases to low-grade fever (see Low-grade fever). Patients complain of severe muscle pain, they develop swelling of the face, conjunctivitis (see), and skin rashes of an exudative or polymorphic nature often appear. In 1IS patients, in the initial period, liquid stools, short-term abdominal pain are noted, with roentgenol. The study sometimes reveals “volatile” infiltrates in the lungs. The number of eosinophils against the background of moderate leukocytosis reaches 25-40%.
In severe cases, the disease often begins with diarrhea and dyspeptic disorders. Feverish reaction, edema, myalgia develop gradually and reach a maximum in the 3rd week of the disease. Muscle pain becomes generalized, accompanied by contractures with immobilization of the patient, swelling spreads from the face and neck to the torso and limbs. Characteristic rashes are erythematous-papular, sometimes hemorrhagic in nature, such as hemorrhagic vasculitis or in the form of pustules. Disorders of c are expressed. n. pp.— insomnia (see), delirium (see), hallucinations (see). Tachycardia (see), cardiac arrhythmias, collapse (see) are observed. From the end of the first week, myocardial lesions of a diffuse nature are detected; in the 3-4th week, the clinical picture of myocarditis, pneumonia, and lesions of c develops. n. With. Sometimes patients experience acute paroxysmal pain, usually in the upper abdomen, accompanied by hemorrhagic rashes and hypereosinophilia up to 80-90%. Dystrophic liver lesions are observed in all cases of severe T., but with recovery they disappear without a trace. The clinic of meningoencephalitis includes general neurol. disorders and is determined by the predominant localization of diffuse focal brain lesions. The development of acute psychoses (see Mental illnesses), hysterical amblyopia (see), epileptiform seizures is possible. The number of eosinophils often does not exceed 30-40%. At the onset of the disease, a decrease in ROE, an increase in hypoproteinemia due to hypoalbuminemia, and an increase in the activity of aldolase and cholinesterase are characteristic. At 4-6 weeks of the disease, there is a tendency to hypercoagulation with the development of thrombohemorrhagic syndrome (see), phlebothrombosis (see Thrombophlebitis).
Children usually tolerate T. relatively easily; pain in the throat, enlargement of the pharyngeal tonsils are often observed, and in some cases a severe course of the disease with a fatal outcome is possible.
Trichinosis - complications
Complications can occur even after successful treatment of trichinosis. These may include:
- menstrual irregularities
- hearing impairment
- weight loss
- hair and nail loss
- peeling skin
- loss of ability to speak
- muscle stiffness
- hoarseness
In people with severe infection, complications may include:
- heart failure
- damage to the central nervous system
- pneumonia
- brain inflammation
- inflammation of the heart
- low blood potassium levels
- blockage of blood vessels
- adrenal insufficiency
Some people may experience long-term complications such as:
- generalized muscle pain
- eye symptoms
- neuropathy
Diagnosis
The diagnosis is established on the basis of a characteristic wedge, picture, epidemiol. medical history (eating raw or insufficiently heat-treated animal meat, which is a possible source of infection). The most difficult diagnosis is severe forms of T., which appear during epidemic outbreaks earlier than other forms, and often begin atypically - with diarrhea. Confirmation of the diagnosis is the detection of Trichinella larvae in meat, which is considered the cause of infection. In case of single diseases, in the case of an unclear source of invasion, a diagnostic muscle biopsy is performed (see Helminthological research methods). Serological reactions are used - RSK, indirect hemagglutination reaction with antigen (see Serological tests).
Differential diagnosis during outbreaks of T. is carried out with acute respiratory viral diseases (see), typhoid fever (see), paratyphoid fever (see), food toxic infections (see Food toxic infections), in children - with measles (see), rubella (see), scarlet fever (see). The main distinguishing features of T. are pronounced eosinophilia, decreased ROE, and high aldolasemia. In case of single diseases, trichinosis is differentiated from Quincke's edema (see Quincke's edema), an allergic reaction to drugs (see Drug allergy), dermatomyositis (see). Granulomatous changes in muscle tissue during dermatomyositis can be interpreted as trichinosis, but unlike T., the skin itself is affected.
Trichinosis - Diagnosis
Diagnosing trichinosis is challenging because the symptoms of the disease are similar to those of other intestinal disorders. Symptoms may be confused with those of the flu or other common illnesses. People with trichinosis produce antibodies against the parasite, which doctors can detect in their blood. In severe trichinosis, muscle biopsy samples may contain Trichinella.
If your doctor suspects your symptoms are caused by a foodborne infection, he or she will ask about consuming raw or undercooked meat.
Treatment
Treatment of patients with mild and erased forms of T. can be carried out at home. For diseases of moderate and severe forms, patients are hospitalized in hospitals with intensive care facilities. For erased and mild forms, antihistamines, calcium salts, analgesics, ascorbic acid are prescribed, but no specific treatment is carried out. For moderate and severe T., specific treatment is prescribed with vermox (mebendazole) at a dose of 300 mg per day for adults (for children - at a dose of 5 mg/kg) in 3 doses after meals. For moderate forms, the drug is taken for 7 days, for severe forms - 10-12 days. Specific therapy for T. is often accompanied by an increase in allergic manifestations of the disease and an increase in the severity of organ damage in the first 1-3 days of treatment. In this regard, for T. of moderate severity, vermox is prescribed while taking antihistamines, and for severe disease - while taking prednisolone at a dose of 30-40 mg per day (for particularly severe disease - at a dose of 60-80 mg ), preferably inside. Treatment with prednisolone at the indicated dose continues for 5-7 days, then the dose of the hormone is reduced over 7-10 days. Specific therapy is more effective and better tolerated the earlier treatment is started. The most effective is specific treatment of infested individuals during the incubation period (preventive therapy), especially in the first week after invasion. If intensive invasion is suspected, preventive treatment must be carried out with Vermox at a dose of 300 mg per day for 7 days.
Patients are prescribed a complete protein diet with limited salt; according to indications, cardiovascular drugs, drugs that improve metabolic processes (ATP, cocarboxylase, vitamins C, group B, plasma transfusion, albumin, digestive enzymes, anabolic hormones, etc.).
Trichinosis - Treatment
Most people with trichinosis need medications to treat the parasitic infection and associated symptoms. As soon as the doctor confirms the diagnosis, he will immediately begin treatment. Treatment of trichinosis within the first 3 days after infection can prevent muscle invasion and progression of the disease.
Because Trichinella is a helminth (parasitic worm), your doctor will prescribe an anthelmintic drug such as albendazole or mebendazole. Mild infections may clear up within 2-6 months with appropriate treatment.
Some people may not need treatment as the infection may clear up on its own within a few months. However, lack of treatment can lead to complications. People with severe infection, such as heart or brain complications, have a poor prognosis. The mortality rate among these individuals is 5%.