Pharmacodynamics and pharmacokinetics
Pharmacodynamics
The active substance is isolated from foxglove leaves .
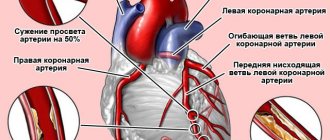
Effect of lanatoside on the cardiac system:
- carliotonic effect – enhances systole and increases the duration of diastole;
- negative dromotropic effect - impulse conduction in the AV node, heart rhythm, cardiac conductivity slows down, myocardial contractility increases, venous pressure decreases, diuresis increases;
- affects potassium-sodium and calcium metabolism in cardiomyocytes, the activity enzyme and the state of cyclic adenosine monophosphate.
Pharmacokinetics
Very well absorbed in the intestines. The cardiotonic effect begins to appear 2 hours after oral administration, the maximum concentration will be reached after 4-6 hours.
Bioavailability is 15-45%. 20-25% of the active substance binds to plasma proteins. Metabolism of the drug occurs in the liver.
The half-life is from 28 to 36 hours. It is excreted from the body in urine and feces unchanged or in the form of inactive metabolites .
Release form and composition
The dosage form of Celanide is tablets: white, biconvex, round (in blister packs of 10 or 30 pcs., in a cardboard pack 1 pack of 30 pcs. or 3 packs of 10 pcs.).
Composition of 1 tablet:
- active substance: lanatoside C – 0.25 mg;
- auxiliary components: calcium stearate (calcium stearate) – 1 mg; potato starch – 14.55 mg; sucrose (granulated sugar, refined sugar) – 16.2 mg; lactose (milk sugar) – 68 mg.
Contraindications
It is prohibited to take the drug if:
- atrioventricular block of 2-3 degrees of severity;
- severe bradycardia ;
- Morgan–Adams–Stokes syndrome;
- WPW syndrome;
- shock states;
- unstable form of angina ;
- acute phase of myocardial infarction ;
- polytopic extrasystole ;
- acute myocarditis ;
- hypersensitivity to digitalis and other cardiac glycosides;
- glycoside intoxication;
- paroxysmal ventricular tachycardia ;
- cardiac tamponade;
- hypertrophic subaortic stenosis ;
- restrictive cardiomyopathy .
Celanid powder substance
Instructions for medical use of the drug
Description of pharmacological action
Blocks Na+-K+-ATPase of cardiomyocytes, increases intracellular calcium content.
Indications for use
Atrial fibrillation, atrial flutter (to slow the heart rate or convert atrial flutter into fibrillation with a controlled frequency of impulses through the AV node), paroxysmal supraventricular tachycardia, chronic heart failure, acute left ventricular failure.
Release form
powder substance; jar (jar) of dark glass 50 g; powder substance; jar (jar) of dark glass 100 g; powder substance; jar (jar) of dark glass 200 g; powder substance; jar (jar) of dark glass 400 g;
Pharmacodynamics
Cardiac glycoside blocks the transport Na+/K+-ATPase, as a result of which the concentration of Na+ in cardiomyocytes increases, which leads to the opening of Ca2+ channels and the entry of Ca2+ into cardiomyocytes. Excess Na+ accelerates the release of Ca2+ from the sarcoplasmic reticulum and increases its concentration in the cell, which leads to inhibition of the troponin complex, which has an inhibitory effect on the interaction of actin and myosin. Increases the force and speed of myocardial contraction by a mechanism different from the Frank-Starling mechanism (does not depend on the degree of preliminary stretching of the myocardium); systole becomes shorter and more economical. As a result of increased myocardial contractility, SV and IOC increase. Reduces ESR and EDV of the heart, which, along with an increase in myocardial tone, leads to a reduction in its size, etc. to reduce myocardial oxygen demand. The negative dromotropic effect manifests itself in increased refractoriness of the AV node. With atrial fibrillation, cardiac glycosides slow heart rate, lengthen diastole, improving intracardiac and systemic hemodynamics. A decrease in heart rate occurs as a result of direct and indirect effects on the regulation of heart rate. Has a direct vasoconstrictor effect (in the event that the positive inotropic effect of cardiac glycosides is not realized in patients with normal contractility or with excessive stretching of the heart); in patients with CHF, it causes an indirect vasodilating effect, reduces venous pressure, increases diuresis, reduces edema, and shortness of breath. Positive bathmotropic effect is manifested in subtoxic and toxic doses. When administered intravenously, the effect begins within 10 minutes and reaches a maximum after 2 hours.
Contraindications for use
Hypersensitivity, glycoside intoxication. With caution. Bradycardia, AV block and CVS without a pacemaker, paroxysmal ventricular tachycardia, HOCM, isolated mitral stenosis, acute myocardial infarction, unstable angina, WPW syndrome, CHF with impaired diastolic function (restrictive cardiomyopathy, amyloidosis, constrictive pericarditis, cardiac tamponade), extrasystole, cardiac asthma in patients with mitral stenosis (in the absence of the tachysystolic form of atrial fibrillation), severe dilatation of the heart cavities, “pulmonary” heart. Electrolyte disturbances (state after dialysis, diarrhea, taking diuretics or other drugs that cause electrolyte disturbances, malnutrition, prolonged vomiting, etc.): hypokalemia, hypomagnesemia, hypercalcemia, hypernatremia. Hypothyroidism, alkalosis, myocarditis, obesity, old age, arteriovenous shunt, hypoxia, renal/liver failure, myocardial infarction.
Side effects
From the digestive system: loss of appetite, nausea, vomiting, diarrhea. From the cardiovascular system: arrhythmias, AV block. From the nervous system: drowsiness, delirious psychosis, sleep disturbances, headache, dizziness, confusion. From the hematopoietic organs: thrombocytopenia, thrombocytopenic purpura. Allergic reactions: skin rash, etc. Other: decreased visual acuity, nosebleeds, petechiae, gynecomastia.
Directions for use and doses
IV, orally (tablets, solution). The dose is set individually depending on the clinical picture and individual sensitivity. To obtain a quick effect, administer 0.2-0.4 mg intravenously 1-2 times a day. Orally, take starting from 0.25-0.5 mg or 10-25 drops of 0.05% solution 3-4 times a day. Maintenance dose - 0.4-0.2 mg intravenously, 0.5-0.25 mg orally or 40-20-10 drops of 0.05% solution. Higher doses: for adults orally - single 0.5 mg, daily 1 mg; IV - single 0.4 mg, daily 0.8 mg. If renal excretory function is impaired, the dose is reduced: with CC 50-80 ml/min, the average maintenance dose is 50% of the average maintenance dose for individuals with normal renal function; with CC less than 10 ml/min - 25% of the usual dose.
Overdose
Symptoms: digitalis intoxication - ventricular paroxysmal tachycardia, ventricular extrasystole (often polytopic or bigeminy), nodal tachycardia, SA block, atrial fibrillation and flutter, AV block, loss of appetite, vomiting, diarrhea, abdominal pain, intestinal necrosis; changes in visual perception (coloring of visible objects yellow-green, perception of objects in a reduced or enlarged form), flickering of “spots” before the eyes, decreased visual acuity; neuritis, radiculitis, manic-depressive syndrome, paresthesia. Treatment: discontinuation of the drug, administration of antidotes (unithiol, EDTA), symptomatic therapy; as antiarrhythmic drugs - class I drugs (lidocaine, phenytoin); for hypokalemia - intravenous KCl (6-8 g/day at the rate of 1-1.5 g per 0.5 l of 5% dextrose solution, 6-8 units of insulin, vitamins B1, B6, C; administered drip over 3 hours); in case of severe bradycardia, AV block - m-anticholinergic blockers (it is dangerous to administer beta-adrenergic stimulants due to a possible increase in the arrhythmogenic effect of cardiac glycosides). In case of complete transverse block with Morgagni-Adams-Stokes attacks - temporary cardiac pacing.
Interactions with other drugs
Antacids, sulfasalazine, cholestyramine reduce absorption. Beta-blockers and verapamil increase the severity of the decrease in AV conduction. Quinidine, methyldopa, spironolactone, amiodarone, verapamil increase blood concentrations (competitive reduction in secretion by the proximal tubules of the kidneys). GCS and diuretics increase the risk of developing hypokalemia and hypomagnesemia; thiazides, Ca2+ preparations (especially with intravenous administration) - hypercalcemia; amiodarone, mercazolil - hypothyroidism. Catecholamines, Ca2+ preparations, and diuretics increase the risk of developing glycoside intoxication.
Precautions for use
It should be borne in mind that the likelihood of intoxication increases in patients with electrolyte disturbances, incl. with hypokalemia, hypomagnesemia, hypercalcemia, hypernatremia, as well as with hypothyroidism, myocarditis, obesity, in elderly patients, with hypoxia, renal and/or liver failure.
Special instructions for use
In HOCM, the administration of lanatoside C leads to greater obstruction. With severe mitral stenosis, normo- or bradycardia, HF develops due to a decrease in LV diastolic filling. Lanatoside C, increasing the contractility of the right ventricular myocardium, causes a further increase in pressure in the pulmonary artery system, which can provoke pulmonary edema or aggravate LV failure. For patients with mitral stenosis, cardiac glycosides are prescribed when right ventricular failure occurs or in the presence of atrial fibrillation. In patients with stage II AV block. the administration of cardiac glycosides can aggravate it and lead to the development of a Morgagni-Adams-Stokes attack. Prescription of cardiac glycosides for stage I AV block. requires caution, frequent ECG monitoring, and in some cases, pharmacological prophylaxis with drugs that improve AV conduction. Lanatoside C in WPW syndrome, by reducing AV conduction, promotes the conduction of impulses through accessory pathways, bypassing the AV node and thereby provokes the development of paroxysmal tachycardia. As one of the methods for monitoring the level of digitalization, monitoring of plasma concentrations of cardiac glycosides is used.
Storage conditions
List A.: In a dry place, protected from light.
Best before date
48 months
ATX classification:
C Cardiovascular system
C01 Drugs for the treatment of heart diseases
C01A Cardiac glycosides
Side effects
When taking too large a dose or hypersensitivity to the drug, the following undesirable conditions appear:
- polytopic extrasystole ;
- bigeminy or trigeminy ;
- marked slowing of heartbeat;
- atrioventricular block;
- ventricular fibrillation;
- decrease in atrioventricular conduction velocity.
Sometimes unpleasant symptoms are observed from other systems:
- changes in peripheral blood in the form of eosinophilia and thrombocytopenia ;
- decrease in daily diuresis;
- from the digestive system: nausea , vomiting , stool disorders: constipation or diarrhea ;
- from the psyche and nervous system: headaches , drowsiness , depression, convulsions , agitation , anxiety , peripheral neuritis , confusion ;
- skin rash;
- impotence;
- gynecomastia.
Overdose
In case of an overdose, symptoms corresponding to side effects occur, only they are more pronounced.
Treatment of overdose:
- gastric lavage with water and activated carbon ;
- taking salt carrier drugs, Cholestyramine , Unithiol , potassium supplements;
- oxygen therapy;
- administration of atropine sulfate and use of an artificial pacemaker (for AV block, significant sinus bradycardia);
- taking Lidocaine , Diphenin , Phenytoin (for ventricular arrhythmia ).
Interaction
Celanide can interact with other medications:
- with calcium supplements – the risk of glycoside intoxication increases;
- with potassium preparations – the toxicity of cardiac glycosides, including Celanide, is reduced;
- with psychotropic drugs, in particular lithium preparations, sympathomimetics ( ephedrine ) - the risk of developing arrhythmias ;
- with medications that in some cases cause disturbances in electrolyte metabolism (corticosteroids, thiazide diuretics and others) - the toxicity of Celanide increases;
- long-term combination with saluretics increases the risk of developing cardiac side effects;
- with Verapamil , Quinidine , Nifedipine , Spironolactone , Amiodarone - the concentration of Celanide in plasma increases;
- with antacids – the adsorption of the drug in the gastrointestinal tract is reduced;
- with Phenobarbital – the effectiveness of Celanide decreases;
- with Aminazine – increases blood ;
- with Lincomycin - there is a risk of pseudomembranous colitis;
- with hypertensive drugs, saluretics (except for potassium-sparing drugs), insulin , Amphotericin , glucose , corticosteroids, antibiotics - the intensity of Celanide excretion decreases and its toxicity increases;
- with anabolic steroids, thiamine chloride, Riboflavin , pyridoxine hydrochloride, folic acid, Inosine , Unithiol , Methyluracil , Methionine , Phosphadenine - the positive inotropic effect of Celanide is enhanced.
ATTENTION!
The information on the page you are viewing is created for informational purposes only and does not in any way promote self-medication. The resource is intended to provide healthcare workers with additional information about certain medications, thereby increasing their level of professionalism. The use of the drug " Celanide " requires consultation with a specialist, as well as his recommendations on the method of use and dosage of the medicine you have chosen.
Source: allmed.pro
special instructions
Special instructions regarding treatment with Celanide:
- During the entire period of treatment, constant medical supervision is required, while the dosage is selected and adjusted individually for each patient;
- if signs of cor pulmonale, coronary insufficiency, problems with the liver or kidneys, or electrolyte imbalance appear, the dose must be reduced;
- Extreme caution is required when using the medicine in patients with angina pectoris or myocardial infarction - it is prescribed only for severe heart failure ;
- it must be taken into account that if the patient has kidney pathologies, the duration of action of Celanide in his body may increase;
- It is advisable to refrain from driving a car and work that requires concentration during the treatment period.
Indications for use of Celanide
According to the instructions for Celanide, this drug is indicated for:
• atrial fibrillation;
• atrial flutter (to reduce heart rate or convert flutter into fibrillation with controlled conduction of impulses through the atrioventricular node);
• paroxysmal supraventricular tachycardia;
• chronic heart failure;
• acute left ventricular failure;
• chronic pulmonary heart disease.
Celanid price, where to buy
In Russian pharmacies, Celanid costs about 30 rubles, in Ukrainian pharmacies – 13-15 hryvnia.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
ZdravCity
- Celanide tab.
0.25 mg No. 30 AO Pharmcenter VILAR 85 rub. order
Pharmacy Dialogue
- Celanide (tab. 0.00025g No. 30) VILAR Pharmcenter
67 RUR order
show more
Method of application of Celanide and dosage
Celanide is intended for parenteral and oral use. The dosage in each clinical case is determined by the doctor. If it is necessary to achieve a quick effect, Celanide is administered intravenously at a dosage of 0.2-0.4 mg, the frequency of administration is 1-2 times a day. The initial dosage for oral administration is 0.25-0.5 mg or 10-25 drops 3-4 times a day. Maintenance dosage – 0.4-0.2 mg (for intravenous administration), 0.5-0.25 mg or 40-10 drops (for oral administration). Maximum dosages: daily – 1 mg, single – 0.5 mg for oral administration; daily – 1 mg, single dose – 0.8 mg for intravenous use.
Before using the drug, you must study the instructions for Celanide, as well as the instructions of your doctor noted in the prescription for Celanide.