- October 21, 2020
- Other drugs
- Ulyana Romanova
“Hydrocortisone” in ampoules is a glucocorticoid drug (GCS) intended for periarticular and intraarticular use. What effect does it have? What does it help to cope with? And are there any contraindications? You will learn the answers to these and many other questions related to this topic from the article.
pharmachologic effect
Hydrocortisone is a glucocorticoid and a synthetic form of endogenously produced cortisol. Glucocorticoids are important steroids for intermediary metabolism, immune function, musculoskeletal and connective tissue, and the brain. Cortisol is the main glucocorticoid secreted by the adrenal cortex.
Natural glucocorticoids (hydrocortisone and cortisol), which also have salt-retaining properties, are used as replacement therapy for adrenal insufficiency. They are also used for their powerful anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body's immune responses to various stimuli.
Analogs
Their discussion is worth completing the study of this topic. Analogues of “Hydrocortisone” in ampoules can be considered drugs that belong to the same pharmacological group and have the same effect on the body as it does.
Popular substitutes are:
- "Ivepred."
- "Betamethasone."
- "Megadexan".
- "Dexasone."
- "Flosteron".
- "Dexamethasone-Vial".
- Solu-Medrol.
- "Deperzolon."
- "Rectodelt".
- "Diprospan".
- "Prednisone acetate."
- "Kenalog."
- "Metypred."
- "Medrol".
- "Medopred".
- "Cortisone".
- "Polcortolon."
However, if for some reason the original drug is not suitable for the patient, or it cannot be found in the pharmacy, his attending physician will also be involved in the selection of an alternative.
Side effects
The medicine is usually well tolerated and causes virtually no side symptoms. Only in rare cases, when the dosage is exceeded, may the following occur:
- water and salt retention, low blood potassium levels, sometimes high blood pressure;
- overexcitation, euphoria, sleep disturbances;
- acne, delayed healing, bruising, skin atrophy;
- hormonal and metabolic disorders: diabetes mellitus (reversible), weight gain, menstrual irregularities.
Overdose
Overdose with long-term use of the drug intramuscularly or intravenously can manifest itself as suppression of the adrenal cortex, nausea and vomiting, hyperglycemia , bleeding, sodium and water retention, increased blood pressure, the development of Cushing's syndrome , and exacerbation of chronic infections.
With topical use of the ointment, acute overdose is unlikely, but with prolonged use, symptoms of chronic overdose with systemic manifestations may appear. Treatment: symptomatic therapy, gradual withdrawal of the drug.
Drug interactions
The metabolism of corticosteroids may be increased and the therapeutic effects reduced by some barbiturates (eg, phenobarbital) and phenytoin, rifampicin, rifabutin, primidone, carbamazepine, and aminoglutethimide.
During long-term prophylactic treatment with any of the antibiotics, dosage adjustments of hydrocortisone should be considered.
Mifepristone may reduce the effect of corticosteroids for 3-4 days.
Concomitant use of salicylates or nonsteroidal anti-inflammatory drugs (NSAIDs) with corticosteroids increases the risk of gastrointestinal bleeding and ulcers.
Ritonavir may increase plasma concentrations of hydrocortisone.
Estrogens and other oral contraceptives increase plasma concentrations of corticosteroids, and dosage adjustments may be necessary if oral contraceptives are added to or removed from a stable dosage regimen.
The desired actions of hypoglycemic agents (including insulin), antihypertensive agents, and diuretics are counteracted by corticosteroids.
The effectiveness of coumarin anticoagulants may be affected by concomitant corticosteroid therapy, and close monitoring of INR or prothrombin times is necessary to prevent spontaneous bleeding.
Concomitant use with methotrexate may increase the risk of hematological toxicity.
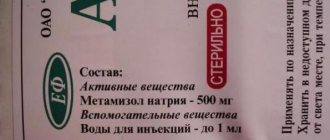
Release form
Lyophilized powder in bottles for the preparation of a solution for intravenous and intramuscular injections of 100 mg and 500 mg, a solvent (alcohol) in ampoules is included.
Suspension in ampoules for intramuscular and intra-articular injections 2.5% 1 ml, 2 ml.
Ointment 1% for external use, 5, 15, 20 and 30 g in a tube.
Eye ointment 0.5% 3.5.10 g in tube.
Eye ointment Hydrocortisone POS 1%, and 2.5% in a tube.
Cream 1% in a tube of 10 ml.
Tablets containing 5, 10 or 20 mg hydrocortisone are available under the name Cortef . An emulsion of 0.1% containing hydrocortisone 17-butyrate has the trade name Locoid Crelo .
Application and dosage
For maintenance treatment (chronic adrenal insufficiency, adrenal hyperplasia), adults are prescribed 20 to 40 mg/day, distributed in the morning, noon and 4 pm.
For children, 12 to 20 mg/m2/day is recommended, distributed in the morning, noon, and 4 pm. In children under 6 years of age, the tablets should be crushed and mixed with food.
Higher doses are needed in cases of intercurrent infection, significant fever, trauma, surgery, serious illness, and significant fever.
Dosage regimen
It is always individual. But in the instructions for using “Hydrocortisone” in ampoules you can read general recommendations.
Most often, the solution is used as a stream, into a vein (including during emergency therapy), or as a drip. Very rarely - into a muscle.
The initial dose can be 100-500 mg - this amount is administered over 30 seconds and 10 minutes, respectively. After the first procedure, repeat procedures are carried out, with breaks of 2-6 hours. The exact interval is determined by the doctor, taking into account the clinical situation.
In some cases, a very large amount of the drug is administered by injection with Hydrocortisone. But this is done only until the patient’s condition has stabilized.
Children are prescribed doses, calculating the required amount using the formula 25 mg/kg/day.
special instructions
In case of digestive disorders that prevent oral administration, parenteral replacement of hydrocortisone in higher doses is required.
Due to the presence of lactose, this drug is contraindicated in patients with congenital galactosemia, glucose-galactose malabsorption syndrome, or lactase deficiency.
When using the medication by athletes, attention must be paid to the fact that this specialty contains hydrocortisone and that this active ingredient is included in the list of doping substances.
Electrocardiograms should be performed in children receiving hydrocortisone to monitor myocardial structure and function.
Contraindications
There are conditions in which adults and children cannot use Hydrocortisone in ampoules. In particular, individual intolerance to the main component. But other contraindications include the following conditions:
- Intra-articular bone fracture.
- Pathological bleeding.
- Periarticular infections.
- Joint instability (usually an outcome of arthritis).
- Previous arthroplasty.
- Inflammatory infectious process in the joint.
- Common infectious diseases.
- Periarticular severe osteoporosis.
- Joint deformation and severe destruction.
- Aseptic necrosis of the bones forming the joint.
That is why the need to use “Hydrocortisone” in ampoules is determined by the doctor after examining the patient and studying his tests. If there are contraindications, the medication can cause great harm.
Nosological classification (ICD-10)
- A16
Respiratory tuberculosis - A17.0 Tuberculous meningitis
(G01*) - B75 Trichinosis
- C34 Malignant neoplasm of bronchus and lung
- C81 Hodgkin's disease [lymphogranulomatosis]
- C82 Follicular [nodular] non-Hodgkin's lymphoma
- C83 Diffuse non-Hodgkin's lymphoma
- C85 Other and unspecified types of non-Hodgkin's lymphoma
- C91 Lymphoid leukemia [lymphocytic leukemia]
- C92 Myeloid leukemia [myeloid leukemia]
- C95.0 Acute leukemia of unspecified cell type
- D59.1 Other autoimmune hemolytic anemias
- D60.9 Acquired pure red cell aplasia, unspecified
- D61.0 Constitutional aplastic anemia
- D69.3 Idiopathic thrombocytopenic purpura
- D86 Sarcoidosis
- E05.5 Thyroid crisis or coma
- E06 Thyroiditis
- E25.9 Adrenogenital disorder, unspecified
- E27.1 Primary
adrenal insufficiency - E27.2 Addison's crisis
- E27.4 Other and unspecified adrenal insufficiency
- E83.5.0* Hypercalcemia
- G35 Multiple sclerosis
- G45 Transient transient cerebral ischemic attacks [attacks] and related syndromes
- G56.0 Carpal tunnel syndrome
- H01.0 Blepharitis
- H01.1 Non-infectious dermatoses of the eyelid
- H10.1 Acute atopic conjunctivitis
- H16.9 Keratitis, unspecified
- H20 Iridocyclitis
- H30.9 Chorioretinal inflammation, unspecified
- H32.0 Chorioretinal inflammation in infectious and parasitic diseases classified elsewhere
- H44.1 Other endophthalmitis
- I01 Rheumatic fever
with cardiac involvement - I21 Acute myocardial infarction
- I61 Intracerebral hemorrhage
- I63 Cerebral infarction
- I95 Hypotension
- I95.1 Orthostatic hypotension
- J38.4 Edema of the larynx
- J45 Asthma
- J46 Status asthmaticus
- J63.2 Berylliosis
- J69.0 Pneumonitis caused by food and vomit
- J82 Pulmonary eosinophilia, not elsewhere classified
- J95.4 Mendelssohn syndrome
- K50 Crohn's disease [regional enteritis]
- K51 Ulcerative colitis
- K72.0 Acute and subacute liver failure
- K72.9 Liver failure, unspecified
- L10 Pemphigus [pemphigus]
- L13.9 Bullous changes, unspecified
- L20 Atopic dermatitis
- L21 Seborrheic dermatitis
- L23.9 Allergic contact dermatitis
, cause unspecified - L25.9 Unspecified contact dermatitis, cause not specified
- L26 Exfoliative dermatitis
- L29.3 Anogenital itching, unspecified
- L30.9 Dermatitis, unspecified
- L40 Psoriasis
- L40.5 Arthropathic psoriasis (M07.0-M07.3*, M09.0*)
- L43.9 Lichen planus, unspecified
- L53 Other erythematous conditions
- L56 Other acute skin changes caused by ultraviolet radiation
- L63 Alopecia areata
- L91.0 Keloid scar
- L92.0 Granuloma annulare
- L92.1 Necrobiosis lipoidica, not elsewhere classified
- L93.0 Discoid lupus erythematosus
- L98.9 Lesions of skin and subcutaneous tissue, unspecified
- M06.9 Rheumatoid arthritis, unspecified
- M08 Juvenile arthritis
- M10.0 Idiopathic gout
- M19.9 Arthrosis, unspecified
- M32 Systemic lupus erythematosus
- M33.2 Polymyositis
- M45 Ankylosing spondylitis
- M65.9 Synovitis and tenosynovitis, unspecified
- M67.8 Other specified lesions of synovium and tendon
- M67.9 Lesion of synovium and tendon, unspecified
- M71.9 Bursopathy, unspecified
- M75.0 Adhesive capsulitis of the shoulder
- M77.9 Enthesopathy, unspecified
- N04 Nephrotic syndrome
- R57.0 Cardiogenic shock
- R57.8 Other types of shock
- R58 Bleeding, not elsewhere classified
- S05.0 Conjunctival trauma and corneal abrasion without mention of foreign body
- S05.9 Injury to unspecified part of eye and orbit
- T45.2 Poisoning by vitamins not elsewhere classified
- T65.9 Toxic effects of unspecified substance
- T78.2 Anaphylactic shock,
unspecified - T78.4 Allergy,
unspecified - T79.4 Traumatic shock
- T80.6 Other serum reactions
- T81.1 Shock during or after procedure, not elsewhere classified
- W57 Bite or sting by non-venomous insects and other non-venomous arthropods
- X20 Contact with venomous snakes and lizards
- X21 Contact with poisonous spiders
- Y40-Y59 Medicines, drugs and biological substances that cause adverse reactions during therapeutic use
- Y47.2 Adverse reactions during therapeutic use of chlorine derivatives
- Z13.0 Special screening examination to identify diseases of the blood and hematopoietic organs, as well as certain disorders involving the immune mechanism
Content
- Structural formula
- Latin name of the substance Hydrocortisone
- Pharmacological group of the substance Hydrocortisone
- Characteristics of the substance Hydrocortisone
- Pharmacology
- Use of the substance Hydrocortisone
- Contraindications
- Use during pregnancy and breastfeeding
- Side effects of the substance Hydrocortisone
- Interaction
- Routes of administration
- Precautions for the substance Hydrocortisone
- Interactions with other active ingredients
- Trade names
Reviews of Hydrocortisone
Ointments and creams containing corticosteroids have antiallergic, anti-inflammatory and antipruritic effects. What is Hydrocortisone ointment for and for what skin diseases is it used? This is primarily eczema, neurodermatitis, psoriasis, itchy and allergic dermatoses, skin manifestations of lupus erythematosus. Most often, hormonal therapy is resorted to only if other local treatments are ineffective. Indeed, the use of this ointment gives a rapid anti-inflammatory effect; after a few days, itching and swelling disappear.
Reviews of Hydrocortisone ointment are most often positive, and this applies to people who tried to use hormonal ointment for the first time. Those who have extensive experience in using hormone-based ointments say that prednisolone is significantly superior in anti-inflammatory activity to hydrocortisone, and also retains water to a lesser extent in the body. And ointments containing dexamethasone and betamethasone are even more active. Hydrocortisone and prednisolone belong to the first generation of corticosteroids, which are relatively weakly active substances. Ointments and creams with these substances are used in pediatric practice, in addition, they can be applied to the skin of the face. Judging by the reviews, for any form of eczema, treatment began with the use of this ointment; in case of an unexpressed effect, more potent agents were used - Fluorocort or Polcortolone. Skin atrophy, acne, hypopigmentation, and striae are common local adverse reactions of corticosteroids that occur on the face and groin area, so low-potency corticosteroids should be used in these areas.
What else can the ointment be used for? It is used in physiotherapeutic procedures, for example, in the treatment with ultrasound of diseases of the joints and spine, scar contractures, heel spurs. Under the influence of ultrasound, exudates are absorbed, analgesic, anti-inflammatory and vasodilating effects are manifested. Phonophoresis using a suspension has a similar effect. Almost everyone who underwent treatment left positive reviews about phonophoresis with hydrocortisone. High efficiency, rapid disappearance of pain and recovery were noted. This procedure was prescribed after gynecological diseases, as well as for sinusitis. Some patients noted an exacerbation after the first sessions.
Information has appeared on the Internet about the use of this ointment for wrinkles. What is this based on and is it harmful to use the ointment for this purpose? Topical application of hydrocortisone causes fluid retention and some swelling, which hides wrinkles and makes them visually invisible. But this is a temporary effect; after the “procedures” are stopped, the liquid is lost and the wrinkles appear again. Doctors are categorically against the use of hydrocortisone for cosmetic purposes. First of all, it is a hormonal drug that has a systemic effect on the body (in the form of changes in metabolic processes) and a local effect - skin atrophy, it becomes thinner and the aging process accelerates. In addition, hormonal ointment causes skin addiction and a decrease in effect when applied topically. Considering the contraindications and possible complications, isn’t the price of such imaginary rejuvenation too high? Hydrocortisone ointment and eye ointment should be prescribed only by a doctor according to strict indications; you cannot treat them yourself. Eye ointment was prescribed to patients with keratitis, chemical burns and after surgical interventions. Some patients experienced burning, redness of the sclera and itching of the eyelids during the first days of using it, but after examination by a doctor, treatment was continued. There are no eye drops containing the active ingredient hydrocortisone. If you are interested in hormonal eye drops, then these are: Oftan Dexamethasone, Dexapos, Maxitrol, Maxidex, Dexamethasone, which includes dexamethasone.
Hydrocortisone can be used for inhalation for laryngitis for decongestant purposes. If a suspension is used for inhalation, it must be diluted. How to dilute for inhalation? Take 1 ml of suspension and 2-3 ml of physiological solution, fill the inhaler, breathe for 5 minutes. Inhalation is carried out in the morning and evening. Reviews about inhalations are positive, since swelling and spasm quickly stop, cough decreases, and breathing becomes easier.
Nasal suspension is sometimes prescribed as an instillation for hypertrophic rhinitis, but, as a rule, this is not effective and surgical treatment cannot be avoided. Otolaryngologists often prescribe pharmaceutical drops, which include a solution of dioxidine, adrenaline and a suspension of hydrocortisone or Miramistin, Nazivin and a suspension. There are good results in the treatment of allergic rhinitis and sinusitis.
Indications
Hydrocortisone is prescribed for acute adrenal insufficiency, status asthmaticus, acute allergies, and for the treatment of shock. In addition, this drug is used for myocardial infarction complicated by cardiogenic shock, for thyrotoxic crisis, for non-purulent thyroiditis, and for congenital adrenal hypoplasia. They treat hypercalcemia, rheumatological and collagen diseases, bullous dermatitis herpetiformis, pemphigus, multiform bullous erythema, exfoliative dermatitis, mycoses, psoriasis.
Hydrocortisone is indicated for use in the treatment of chronic eye lesions, berylliosis, symptomatic sarcoidosis, Loeffler's syndrome, focal or disseminated tuberculosis, aspiration pneumonitis, idiopathic thrombocytopenic purpura, congenital hypoplastic anemia, erythroblastopenia. With the help of this medicine, palliative therapy is carried out for leukemia and lymphomas, increases diuresis and reduces proteinuria in nephropathic syndrome. Used for regional enteritis, tuberculous meningitis, ulcerative colitis, trichinosis with damage to the heart muscle or nervous system.
The medicine in the form of a cream is used in the treatment of skin diseases of non-microbial etiology (inflammatory and allergic): eczema, dermatitis, toxicoderma, neurodermatitis.
It is also good to do inhalations with Hydrocortisone for bronchitis and laryngotracheitis. Due to its anti-allergic and anti-inflammatory effects, the drug is excellent for the treatment of bronchitis accompanied by asthmatic syndrome and bronchial asthma.
Given the immunosuppressive property of this glucocorticosteroid, it is prescribed for transplantations and implantations, as well as for blood transfusions.