A number of hormones produced by our body have synthetic and artificial analogues. They are not always medicines: much more often the circulation of such substances is regulated by criminal or special legislation. Among medications, replacement or addition natural hormones Testosterone pionate, ethinyl estradiol, thyroidin are used. But most of the copies are broken around the synthetic corticosteroid prednisolone. Few people think about what it helps with, but it is in relation to it that the phrase “put on hormones” is used.
Description of the drug
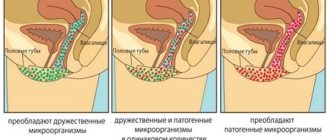
Prednisolone is a glucocorticoid hormone, which is a synthetic analogue of our hydrocortisone. The latter is produced by the adrenal glands, or more precisely, their cortex. The function of hydrocortisone in the body is to preserve glucose reserves in the liver and regulate water and electrolyte balance. The maximum amount of this hormone occurs in the morning, and the minimum in the evening.
Prednisolone is not a complete analogue of hydrocortisone and the latter cannot always be replaced by the former. Moreover, its use is not based on its functions as a hormone. Speaking about prednisolone, it is worth mentioning its dose dependence. Some properties that were once considered side effects have become medicinal in large doses: it is not used for hormonal disorders.
Anti-inflammatory and antihistamine effect
Prednisolone suppresses the production of histamine and prevents its secretion into the bloodstream . It also helps reduce the number of lymphocytes and antibodies.
This drug can act in any form, so all release options are common: in the form of injections, tablets and ointments.
The effectiveness of the drug against inflammation and allergic reactions is so pronounced and rapid that at one time prednisolone became a panacea against these unpleasant phenomena. They began to massively treat allergies, arthritis, heart attacks and tuberculosis.
But it was then that a number of difficulties arose related to the side effects of this medicine. I had to remember that this is, after all, a hormone.
Side effects
There were so many of them that a number of restrictions were imposed on the use of prednisolone. The list of side effects looks like this:
- The drug prevents the absorption of potassium in the intestine, but accumulates sodium and fluid. This negatively affects the functioning of the heart.
- By blocking the secretion of lymphocytes, prednisolone becomes an immunosuppressant, that is, it reduces the body's defenses.
- Blood glucose levels increase, resulting in increased insulin production. This leads to excess weight despite the fact that the hormone itself has a lipolytic and catabolic effect.
- Increases the secretion of gastric juice, which leads to the formation of ulcers.
- Removes calcium from the body, which causes osteoporosis.
With prolonged use of the drug, these effects become pronounced: patients experience fat deposition in the upper body , stomach and musculoskeletal problems.
After stopping taking prednisolone, withdrawal syndrome is observed - because the body, getting used to the synthetic hormone, reduces the production of its own.
Indications for use
Before giving preference to Prednisolone or Prednisone tablets, the instructions for use of each drug should be studied very carefully. It would seem that since the same substance is present in the medications, then their purpose should be the same. Is it really? Is it possible to safely replace one remedy with another? Let's figure it out.
Prednisolone tablets are prescribed for endocrine disorders, adrenal pathologies, severe allergies, rheumatic diseases, hematological diseases and liver dysfunction. Also, indications for use of the drug will be oncological and neurological pathologies, infectious diseases, and surgical interventions. The drug Prednisone is used under the same circumstances.
Application in treatment
Today, there are many diseases and acute conditions for which prednisolone is used. Many people know why this drug is prescribed: perhaps everyone has taken it at least once in their life, most often once.
Joint diseases
In chronic forms of joint diseases, glucocorticoids are used to relieve pain and restore connective tissue. Prednisolone is used in the form of tablets, and if there are contraindications to their use, an intra-articular injection is made, which creates a depot directly in the affected joint.
Today, similar pathologies are treated with other means, so often prednisolone and other hormones are the drugs of choice here.
Among the diseases of the musculoskeletal system for which prednisolone is used, the following can be noted:
- rheumatoid arthritis;
- periarthritis;
- bursitis;
- tenosynovitis;
- dermatomyositis;
- polyarthritis.
Since prednisolone has a beneficial effect on connective tissue, it is actively used in the treatment of rheumatism, systemic lupus erythematosus, and scleroderma.
Endocrine diseases
This is the case when prednisolone is used for its intended purpose - as a substitute for natural hormones of the adrenal cortex. The drug is used continuously in individually calculated dosages. As a rule, these are congenital pathologies, but sometimes they are the result of other diseases. Among such endocrine diseases, three are worth mentioning:
- hypocorticism;
- adrenogenital syndrome;
- Addison's disease.
In such conditions, the production of cortisol is reduced or absent, and patients are forced to “go on hormones” for life.
Asthma and COPD
Prednisolone for bronchial asthma and chronic obstructive pulmonary disease is used when the body does not respond to bronchodilators or they are contraindicated. This property of glucocorticosteroids is used here as an anti-inflammatory effect . They reduce obstruction in the bronchi, so the main form of their use is aerosol. Inhalers are produced containing hormone compounds with chlorine, fluorine and other elements.
Prednisolone can be used systemically instead of inhalers, both in the form of tablets and injections. At the same time, due to the average age of patients and the removal of calcium from the body by glucocorticoids, drugs against osteoporosis are prescribed in parallel with them.
I suffer from asthma and arrhythmia at the same time. I take bronchodilators, which make my heart skip a beat. And heart medications cause bronchospasms. My hormones turned out to be better, but I gained weight.
Anna
Prednisolone becomes mandatory when status asthmaticus occurs, an acute attack of suffocation, in which all remedies have already been exhausted and do not work. This is a life-threatening condition with a mortality rate of 5%. Prednisolone is administered in a large dose - 300-400 mg, often in the form of a dropper every three hours.
Acute allergic reactions
Today there are a lot of remedies for allergies. These are antihistamines with different mechanisms of action. The latest generation of products is designed for dose accumulation in the body and prolonged action. They do not cause drowsiness, but serve as a good prevention of exacerbations. In fact, hormonal drugs are now rarely used in the treatment of allergies. But sometimes situations arise in life when the only thing that can save a person is prednisolone. This happens in the following cases:
- For the first time in his life, a man ate something to which his body reacted with Quincke's edema and urticaria. Since he does not know what to do about it, the symptoms progress before his eyes, and swelling can occur anywhere - for example, in the larynx.
- Allergic reaction to a viral infection. A virus is a living organism consisting of several molecules, one of which is DNA or RNA, and the rest are proteins that protect the genetic material and perform an invasive function. An allergic reaction in such cases is natural, but sometimes it can take life-threatening forms. Thus, the consequence of viral infections can be encephalitis with cerebral edema, the mortality rate of which is about 25%. Among the champions for this complication are the pathogens of herpes, chicken pox and measles.
- Introducing a new drug parenterally or being bitten by an insect that has not bitten before can trigger anaphylactic shock. This is a condition in which blood pressure decreases, bronchospasm begins. Due to the sharp restriction of oxygen supply to the brain, anxiety appears, and then collapse occurs. Death can occur within minutes to hours from cardiac arrest. With the secondary introduction of the allergen, the likelihood of anaphylaxis increases, and with prolonged remission, it decreases.
The only drug available here is prednisolone. It is prescribed in “frightening” doses. So, in case of anaphylactic shock, it is administered after adrenaline in a single dose of 500 mg. If it is not possible to relieve bronchospasm, give an injection of aminophylline.
One day at work I was bitten by a hornet. Before that, I didn’t tolerate bites well, but then my shift worker had to call an ambulance. There was clinical death. I woke up in the intensive care unit, prednisolone was being administered. By evening it disappeared as if by hand.
Hope
For angioedema, 60 to 90 mg of prednisolone is enough. The injection can be given either intramuscular or intravenous. In this case, the dose may vary depending on whether the patient is a child or an adult.
Cerebral edema involves regular injections of 60-90 mg up to three times a day until symptoms subside. Treatment is carried out, naturally, in intensive care.
Other uses of prednisolone
In clinical practice, prednisolone has found use in complex therapy of the following diseases:
- seborrheic dermatitis;
- psoriasis;
- hepatitis;
- inflammatory eye diseases - conjunctivitis, blepharitis;
- agranulocytosis;
- lymphogranulomatosis;
- hemolytic anemia.
As a rule, the drug in these cases is taken either orally or in the form of eye drops.
Patient reviews
I was prescribed Prednisolone during allergies. To be honest, after I found out about the side effects, I was afraid to take it. But when it got really bad, I had to. I was pleasantly surprised that one ampoule of this drug helped me. Now I often use this product, of course, when necessary.
Valentina
I spend most of my time at work and I simply don’t have time to go to hospitals. When my allergies started, I didn’t go to the doctor, but hoped that everything would go away on its own. In general, I reached a state where my whole body itched terribly and there was severe swelling. At first I was prescribed some injections, but they had no effect. After this, Prednisolone tablets were prescribed. You had to drink them for 2 weeks. After taking it for three days I felt much better.
Elena
The doctor prescribes me to take this drug every year, since I suffer from allergies throughout the summer.
He helps me well. I take 2 tablets 2 times a day as prescribed by the doctor. Then I gradually reduce the daily dosage. Vladimir
Contraindications and restrictions
Due to its versatile action, prednisolone, especially with its long-term use, works according to the saying: “we treat one thing, cripple another . Because of this, in some cases it becomes the last thing the doctor turns to. If prednisolone is prescribed for allergies, its dosage should be strictly controlled.
Prednisolone is contraindicated if you have:
- Stomach or duodenal ulcer. The drug can cause perforation and bleeding.
- Itsenko-Cushing syndrome, when the adrenal cortex produces a clear excess of corticosteroids.
- Osteoporosis.
- Kidney failure.
- Hypertension, especially in severe form.
- Viral infections in the acute phase.
- Vaccination - taking prednisolone can reduce the entire work of the vaccine to zero due to the immunosuppressive effect.
- Syphilis.
- Tuberculosis in open form.
When prescribing prednisolone to children and pregnant women, one should be guided only by vital indications. In this case, it is necessary to compensate for the negative effects of the drug on the body.
If you have been taking prednisolone for a long time and no longer need it, the dose should be reduced gradually. Abrupt cessation of use will provoke withdrawal syndrome.
Drug interactions
Due to its high pharmacological activity, prednisolone, like other corticosteroids, can weaken or enhance the effect of many drugs/substances. If it is necessary to use Prednisolone solution, tablets or eye drops in combination with other drugs, the attending physician should consider and take into account their possible interaction.
There are no data on drug interactions of the ointment.
Due to the possible pharmaceutical incompatibility of Prednisolone solution with other drugs administered intravenously, it is recommended to administer it separately: as a bolus, or through another dropper. Mixing solutions of prednisolone and heparin occurs with the formation of a precipitate.
Forms of release and administration of the drug
This drug is available in a wide variety of forms. The following forms are available in pharmacies:
- prednisolone ointment, concentration 0.5%;
- tablets, from 1 to 5 mg;
- eye drops, 0.5%;
- solution for injection, ampoules 30 mg/1 ml.
The anti-shock kit also contains methylprednisolone, a stronger derivative in large quantities.
Trade names of prednisolone may vary: in pharmacies it can be sold under the brands Decortin and Medopred.
Withdrawal syndrome
Abrupt withdrawal of Prednisolone can provoke serious consequences, including the development of collapse and even coma. Therefore, doctors always inform patients about the inadmissibility of skipping a glucocorticosteroid or unauthorized termination of treatment. Prescribing high daily dosages often leads to improper functioning of the adrenal cortex. When discontinuing the drug, the doctor recommends that the patient take vitamins C and E to stimulate the functioning of these paired organs of the endocrine system.
Dangerous consequences that occur after stopping Prednisolone therapy also include:
- return of pathological symptoms, including pain;
- headache;
- sudden fluctuations in body weight;
- worsening mood;
- dyspeptic disorders.
In this case, the patient should resume taking the drug for several weeks, and then, under the supervision of a doctor, gradually reduce the single and daily dosages. During the withdrawal of Prednisolone, the doctor monitors the main indicators: body temperature, blood pressure. The most informative tests include laboratory tests of blood and urine.
Proper nutrition allows you to avoid the negative consequences of taking Prednisolone
Pharmacological properties
Pharmacodynamics
Prednisolone is a synthetic corticosteroid, a dehydrogenated analogue of hydrocortisone. It has an immunosuppressive, anti-inflammatory and antiallergic effect, and also increases the sensitivity of beta-adrenergic receptors to norepinephrine, adrenaline and dopamine.
Prednisolone interacts with special receptors for GCS, which are present in all tissues. The complex formed as a result of this interaction induces the synthesis of proteins, including enzymes that regulate important processes that occur in the cells of the body.
The drug affects all types of metabolism (protein, carbohydrate, lipid and water-electrolyte).
The anti-inflammatory effect of Prednisolone occurs by reducing capillary permeability, stabilizing cell membranes and organelle membranes, activating the release of inflammatory mediators by eosinophils and mast cells, inducing the synthesis of lipocortins and reducing the number of mast cells that produce hyaluronic acid. The effect of the drug is manifested at all stages of inflammation: it inhibits the synthesis of anti-inflammatory cytokines and prostaglandins and makes cell membranes more resistant to the influence of damaging factors.
The antiallergic and immunosuppressive effect of Prednisolone develops due to the following mechanisms: a decrease in the synthesis and secretion of allergy mediators; reduction in the number of circulating mast cells, basophils, T-lymphocytes and B-lymphocytes; inhibition of histamine release from mast cells and basophils; reducing the sensitivity of body cells to allergy mediators; inhibition of antibody synthesis; suppression of the development of lymphoid and connective tissue; modification of the immune response.
In patients with obstructive airway diseases, Prednisolone prevents or reduces swelling of the mucous membranes, inhibits the process of inflammation, reduces the infiltration of eosinophils in the bronchi and inhibits exfoliation and erosion of the mucous membrane. Beta-adrenergic receptors located in the middle and small bronchi become more sensitive to endogenous catecholamines and exogenous sympathomimetics. The drug also helps to reduce mucus production and reduce its viscosity.
When used externally, in addition to anti-inflammatory and antiallergic effects, Prednisolone exhibits antipruritic and antiexudative activity. It reduces vasodilation at the site of inflammation, reduces inflammatory reactions in the skin and increases the permeability of vascular walls.
Pharmacokinetics
After taking the tablets orally, the drug is quickly absorbed from the gastrointestinal tract (maximum concentration in plasma is observed after 1–1.5 hours). Approximately 90% of prednisolone is bound to plasma proteins (mainly transcortin and albumin).
Metabolism occurs in the kidneys, liver and other tissues by conjugation with glucuronic acid and sulfuric acid. Metabolites of Prednisolone are pharmacologically inactive.
The drug is excreted by the kidneys (urine) and liver (bile). About 20% is excreted unchanged in the urine. The half-life of the drug after oral administration is 2–4 hours, and after intramuscular or intravenous injection – 2–3 hours.