General information
Pulmonary edema is a clinical syndrome based on excessive transudation of fluid from venules/capillaries into the interstitial lung tissue, and then into the alveoli, and is accompanied by a severe disturbance of gas exchange in the lungs with the development of hypoxia of various tissues, acidosis , and depression of central nervous system functions.
Pulmonary edema code according to ICD-10: J81. This clinical syndrome can be a complication of various cardiological, pulmonary, urological, gynecological, neurological, and gastroenterological diseases. Pulmonary edema is one of the most severe clinical and common types of acute heart failure (AHF), the prevalence of which is 0.5–2.1%. At the same time, by age, pulmonary edema “leads” in elderly people in the age group over 65 years. The mortality rate for pulmonary edema varies from 50 to 80% depending on the etiology and is significantly higher in older people. It is fundamental to divide pulmonary edema into two types - cardiogenic and non-cardiogenic, which is due to different etiology, pathogenesis, course characteristics, treatment tactics and further prognosis.
, cardiogenic pulmonary edema is more common . In most cases, cardiogenic edema develops with ischemic heart disease, CHF, acute cardiac arrhythmias, and valve pathologies in which congestion in the lungs develops. In old age, coronary heart disease predominates, and in young people, heart defects, dilated cardiomyopathy , and myocarditis .
Refers to life-threatening complications that require urgent measures. Delay in providing medical care for pulmonary edema leads to death.
The development of the pathological process is based on an increase in pressure (gradual/sharp) in the pulmonary circulation. At the same time, the speed of development of the pathological process is of utmost importance, since the likelihood of cardiogenic edema occurring is much higher in acute disorders, since in such situations compensatory mechanisms do not work (they do not have time to stop/reduce their consequences). In cases of a more gradual development of the process of circulatory failure and an increase in clinical manifestations, the consequences are often not so dramatic.
Non-cardiogenic pulmonary edema develops both with direct damage to the lungs (inhalation of toxins/toxic gases, aspiration of gastrointestinal contents, water, blood, burns, pneumonia ) and with extrapulmonary diseases ( shock , severe polytrauma, sepsis , massive blood loss, pancreatitis / pancreatic , blood transfusion , uremia ) is much less common. Another syndrome manifested by non-cardiogenic pulmonary edema and acute respiratory failure is ARDS - acute primary/secondary respiratory distress syndrome (synonymous with wet lung, shock lung). The development of this type of edema is caused primarily by a disruption of the function/structure of the alveolocapillary membrane.
According to modern concepts of primary ARDS, the damaging factor directly affects alveolocytes , surfactant , leading to damage to the alveolar epithelium and disruption of the integrity of the alveolar capillary membrane, resulting in transfusion of the liquid component of blood into the alveolar spaces. In secondary ARDS, the basis is an extrapulmonary factor that forms against the background of an inflammatory reaction syndrome in the body ( sepsis , bacteremia ). Edema of this type (shock lung) does not obey the laws of fluid transport and does not depend on the level of hydrostatic pressure.
Its peculiarity is a sharp decrease in ventilation/oxygenation of the body, causing congestion in the lungs, oxygen deficiency in the tissues of the brain and heart with the rapid development of life-threatening conditions. With inadequate/delayed assistance, mortality reaches 65-80%.
Providing emergency assistance
There are a number of urgent measures to provide first aid to a person with pulmonary edema. The absence of such assistance can worsen the patient's condition.
Read: Blind probing with sorbitol and analogues
First aid:
- It is necessary to give the patient a sitting position, and it is necessary to lower his legs to the floor.
- Organize direct access to fresh air, which will help breathing.
- Place your feet in hot water; foot baths will dilate blood vessels.
- Allow the patient to breathe freely by removing tight and constricting clothing.
- Monitor breathing and pulse, measure blood pressure every 5 minutes.
- Allow the patient to inhale alcohol vapor.
- It is imperative to restore the patient’s mental and emotional state.
- For low blood pressure, give nitroglycerin.
- Apply venous tourniquets to the lower extremities.
- Provide access to a large vein upon the arrival of doctors.
First aid is required before the ambulance arrives
These measures are carried out before the ambulance arrives. The emergency team, prior to medical examination and diagnosis, carries out some measures before arriving at the hospital. Usually this:
- Suctioning foam and inhaling alcohol vapor
- Removing excess liquid
- Pain relief for pain or shock
- Subcutaneous administration of camphor solution
- Using an oxygen cushion to enrich breathing with oxygen
- Bloodletting
- Pressure regulation
The remaining measures are carried out in the hospital under the guidance of specialists.
After complete stabilization of the patient’s condition, treatment of the patient begins, which is aimed at eliminating the causes of edema.
Preventing oxygen starvation is the primary task of doctors. Otherwise, the consequences of the attack will be irreversible.
The coordinated work of emergency workers and the correct actions of loved ones will help avoid serious complications and consequences after an attack of respiratory failure.
Pathogenesis
The pathogenesis of pulmonary edema is determined by its type (cardiogenic/non-cardiogenic). Accordingly, a hydrostatic and membranogenic mechanism for the development of edema is distinguished.
Hydrostatic pulmonary edema
The main etiological factor is diseases of the cardiovascular system, in which there is an increase in intracapillary hydrostatic pressure. When the pressure reaches 15 mm Hg. Art. blood plasma is transfused into the interstitium in a volume that exceeds the physiological ability to remove it by lymphatic drainage. When pressure rises to 20 mm Hg. Art. and higher, the liquid enters the surface of the alveoli. The mechanism of development of this type of edema is based on the Frank-Starling law, which describes the patterns of exchange of liquid media in lung tissue. Within the framework of the article, it is not possible to decipher each of the operating factors of the formula. Let us highlight only the main sequentially changing interconnected stages of the pathological process:
- An increase in hydrostatic pressure in the pulmonary circulation, which contributes to an increase in pressure in the pulmonary artery and then inside the capillaries of the lungs.
- Increased filtration of fluid from the pulmonary vessels directly into the tissue.
- The formation of excessive negative pressure in the interstitial space of the lungs and the development of interstitial edema .
- Decompensation of fluid outflow through the lymphatic pathways.
- Development of alveolar edema (a developed clinical picture of pulmonary edema is observed).
- Reduction in the area of gas exchange and disorganization of the gas exchange mechanism between the external air and blood.
- A state of hypoxia , which, in turn, provokes the production of stress hormones, catecholamines , which leads to an even greater increase in blood pressure and a decrease in vascular permeability, further increasing the load on the left ventricle of the heart, thereby forming a vicious circle.
The figure schematically shows the pathogenesis of cardiogenic pulmonary edema
Membranogenic pulmonary edema
Its development is due to a primary increase in permeability and dysfunction of the alveolar-capillary membrane, which is caused by damage to the alveolar epithelium and capillary endothelium. Increased insight occurs under the influence of toxic oxygen radicals, proteinases , prostaglandins , leukotrienes , histamine , formed or released in the tissue under the influence of various types of irritants.
An increase in the permeability of the pulmonary capillaries quickly leads to the appearance of a large amount of edematous fluid, which contains a lot of protein. At the same time, changes in the permeability of the alveolar and capillary parts of the barrier do not occur uniformly. First, the permeability of the endothelial layer increases, which leads to the leakage of vascular fluid into the interstitium, where it temporarily accumulates ( interstitial pulmonary edema ). At the same time, interstitial edema is partially compensated by accelerating lymph drainage. In most cases, this adaptive reaction is insufficient, and gradually the edematous fluid penetrates through the surface of the destructively altered cells of the alveoli into their cavity, filling the entire volume.
Alveolar pulmonary edema develops . The exclusion of part of the alveoli from the gas exchange process is compensated by stretching (emphysema) of the remaining intact alveoli, which leads to compression of the lymphatic vessels and capillaries of the lungs. Alveolar edema develops when the alveoli are filled with fluid and is characterized by the appearance of severe disturbances in the respiratory system, the development of arterial hypoxemia / hypercapnia .
Against this background, microcirculation changes/blood viscosity increases (development of DIC syndrome). Vascular reactivity and bronchial muscle tone are disrupted, surfactant activity decreases, which leads to the development of microatelectasis . Alveolar hypoventilation increases, leading to a mismatch between perfusion and ventilation, changes in carbon dioxide/oxygen diffusion and a decrease in oxygen supply to tissues with the development of hypoxia and metabolic acidosis .
Membranogenic pulmonary edema develops under the influence of various types of damaging factors, one of which is toxicants of various origins, using the example of which we will consider in more detail the pathogenesis of toxic edema.
The figure schematically shows the pathogenesis of toxic pulmonary edema
Toxic pulmonary edema . The pathogenesis of this type of pulmonary edema is due to the effect of toxicants directly on the cells of the alveolar-capillary barrier with disruption of their function. Toxic edema has different mechanisms of damage to lung cells, but the pathological processes that develop behind this are quite similar. When cell damage/death occurs, the permeability of the barrier increases and the production of biologically active substances in the lung tissue sharply increases ( histamine , norepinephrine , angiotensin , acetylcholine , serotonin , prostaglandins ), which contributes to a further increase in permeability/impairment of the function of the alveolar-capillary barrier and the development of hemodynamic disorders in the lungs (blood flow speed decreases, pressure in the pulmonary circulation increases). As the edema progresses, the respiratory and terminal bronchioles fill with fluid, and under the influence of turbulence arising from air movement, foam forms in the airways.
Pulmonary edema of mixed type . The development is based on a combination of the mechanisms of edema of both types.
Classification
There is no single generally accepted classification of pulmonary edema. It is generally accepted to divide pulmonary edema into cardiogenic and non-cardiogenic.
Cardiogenic pulmonary edema, in turn, is divided according to several criteria.
Based on the presence/absence of a history of CHF:
- Newly occurring (without a history of CHF).
- Decompensated (acute decompensation of CHF).
Due to the occurrence:
- Left ventricular failure ( arrhythmias ; acute coronary syndrome; myocarditis / pericarditis / endocarditis ; valve dysfunction - mitral insufficiency, aortic stenosis , etc.).
- Increased intravascular volume ( renal failure , volume overload).
- Pulmonary venous obstruction ( mitral valve stenosis ).
Non-cardiogenic edema is divided into:
- Primary - associated with the presence of a damaging factor directly in the lung tissue.
- Secondary - developing in the presence of an extrapulmonary factor and severe systemic inflammation.
Along the flow they distinguish:
- Fulminant edema - rapid development over several minutes, fatal.
- Acute edema – increases rapidly (over a period of up to 4 hours). Develops mainly with myocardial infarction , anaphylaxis , and traumatic brain injury. Even with timely resuscitation measures, there is a high risk of death.
- Subacute edema is characterized by a wave-like course with a gradual increase in symptoms and its subsidence. It is observed more often with endogenous intoxication of the body of various origins ( liver failure , sepsis , uremia ).
- Prolonged edema – development period from 12 hours to 1-3 days. It often occurs mildly, with mild symptoms without characteristic clinical signs. It occurs more often in chronic lung diseases, CHF.
Causes of pulmonary edema
The main cause of pulmonary edema in heart disease (cardiogenic edema) is an increase in hydrostatic pressure in the capillary system of the pulmonary artery. The most common cause of edema is congestive cardiac failure, often left ventricular failure, caused by decreased myocardial contractility, volume/pressure overload, or heart valve pathology. An increasing imbalance of arterial/venous blood supply and the development of pronounced venous stagnation in the pulmonary circulation is an unfavorable prognostic sign. Venous congestion in the lungs, what is it? This is a violation of the hemodynamics of the pulmonary circulation, characterized by overflow of the venous portion of the bloodstream with blood, caused by cardiac disorders.
The immediate causes and factors contributing to the development of cardiogenic pulmonary edema are “cardiac” factors - CHF in the stage of decompensation, hypertensive crisis , exacerbation of coronary heart disease, severe pathology of the heart valves, acute arrhythmia , acute myocarditis / endocarditis / pericarditis ; non-cardiac factors - volume overload (massive administration of blood replacement solutions), severe stroke , renal failure , alcohol abuse, drug overdose.
The causes of the development of non-cardiogenic pulmonary edema can be: inhalation of toxic substances, severe chest trauma, acute viral lung diseases ( pneumonia ), sepsis, aspiration syndrome , radiation damage to the lungs, blood transfusion, pancreatic necrosis , polytrauma, blood loss.
Medicines
Photo: healthline.com
To suppress the activity of the respiratory center, morphine, which is a narcotic analgesic, is used. This effect is achieved due to the effect of the drug on mu receptors. In case of an overdose, the following symptoms appear: dizziness, confusion, cold sticky sweat, decreased blood pressure, decreased heart rate, difficulty breathing, dry oral mucosa, and occasionally hallucinations and convulsions. If a clinical picture of overdose develops, it is necessary to administer intravenously a specific antagonist of narcotic analgesics - naloxone.
Furosemide is used as a diuretic, which reduces the volume of circulating blood. When administered intravenously, the effect is achieved within 5 to 10 minutes. Furosemide is known to lower blood pressure, so administration of the drug should be carried out under strict control of blood pressure levels. In addition, nitrates are administered under control, the effect of which is aimed at reducing venous blood flow to the heart, resulting in a decrease in pressure in the right atrium, in the pulmonary artery system, and also a decrease in peripheral vascular resistance.
Cardiac glycosides are used to weaken myocardial contractility, which subsequently leads to decompensation of cardiac activity. These drugs normalize metabolic processes and energy metabolism in the heart muscle, due to which the systolic function of the myocardium is significantly enhanced. As a result, stroke volume increases, blood pressure rises, and the rhythm of cardiac activity slows down.
The use of antihypertensive drugs is necessary in the presence of high blood pressure. The choice of a specific drug and its dosage is made depending on the initial blood pressure figures.
Antiarrhythmic drugs are used when a person has a rhythm disorder of any etiology.
Thrombolytic agents, antihistamines and antibacterial agents are prescribed according to indications.
Symptoms of pulmonary edema
It belongs to the group of conditions that can be diagnosed almost at a distance, since the symptoms of pulmonary edema in adults are very characteristic: severe shortness of breath , predominantly inspiratory, much less often mixed; orthopnea (shortness of breath when lying down); cough with sputum production; the number of respirations exceeds 30/min.; cold profuse sweat; cyanosis of the skin/mucous membranes; presence of wheezing in the lungs; tachycardia (gallop rhythm), auscultation - accent of 2 tones over the pulmonary artery.
Signs of pulmonary edema in humans are determined by pathogenetic processes. Conventionally, clinically there are several stages:
- Dyspnoetic. It manifests itself as dry rales, dyspnea , which is associated with the onset of edema of predominantly interstitial lung tissue, and isolated moist rales.
- Orthopnea stage . Characterized by an increase in wet wheezing, which prevails over dry wheezing.
- Stage of expanded clinic. Severe orthopnea, wheezing is clearly audible at a distance.
- Difficult stage. Many different types of wheezing, foaming, profuse cold sweat, progressive diffuse cyanosis .
In practice, it is extremely important to distinguish between the interstitial and alveolar stages of edema development. Interstitial pulmonary edema corresponds to the clinical symptoms of cardiac asthma, which is caused by a sharp deterioration in the exchange of oxygen and carbon dioxide between the blood and the air of the alveoli, which contributes to an increase in vascular and bronchial resistance.
An attack of cardiac asthma usually develops at night. The patient wakes up from a strong feeling of lack of air, is forced to take a sitting position, tries to open the window, fear of death appears, excitement appears, does not answer questions, concentrating on the struggle for air.
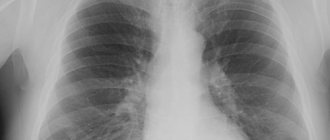
The duration of an attack of cardiac asthma varies from 5-10 minutes to 1-3 hours. On auscultation - dry wheezing, weakened breathing in the lower parts of the lungs. In cases of chronic heart failure, mitral stenosis, accompanied by hypervolemia of the pulmonary circulation, X-ray examination is more important for diagnosing interstitial edema. The X-ray shows characteristic signs - increased pulmonary pattern, which is especially pronounced in the hilar zones, which is due to the presence of lymphatic spaces and edematous infiltration of peribronchial/perivascular and interstitial tissue; presence of Kerley's line and subpleural edema .
X-ray image. Interstitial edema
Next, fluid from the interstitium enters the alveoli, which causes alveolar pulmonary edema with collapse of the alveoli, destruction of surfactant, and flooding of the alveoli with transudate. At this stage, the formation of a persistent protein foam may occur, which blocks the lumen of the bronchi/bronchioles, which leads to hypoxemia and hypoxia .
Acute alveolar pulmonary edema refers to a more severe form of left ventricular failure. The transition from interstitial edema to alveolar edema often occurs quite quickly - within a few minutes. Rapidly occurring alveolar edema often develops at the onset of myocardial infarction or at the height of a hypertensive crisis .
Characteristic is loud bubbling breathing with the release of white or pink foam due to the admixture of red blood cells. Against this background, blood oxygenation is sharply impaired and there is a high risk of asphyxia . As a rule, the extensive clinical symptoms of alveolar edema are pronounced and do not cause difficulties in making a diagnosis. An additional characteristic sign is the appearance of a significant number of moist wheezing of various sizes, sometimes dry wheezing is also present. Alveolar edema, like cardiac asthma, occurs mainly at night. The attack can be either short-term, which goes away on its own, or long-lasting, lasting several hours. In cases of strong foaming, death from asphyxia can quickly occur, literally within 5-10 minutes after the appearance of the first clinical manifestations.
X-ray image. Alveolar pulmonary edema.
With alveolar pulmonary edema, the typical x-ray picture is caused by transudate infiltration symmetrically in both lungs with localization of edema mainly in the basal and hilar regions.
Laboratory data have no clinical significance and are reduced mainly to sudden changes in the gas composition ( hypoxemia ) and the acid-base state of the blood ( metabolic acidosis ). The ECG shows tachycardia , increased/deformed amplitude of the P wave, decreased ST segment.
In congestive heart failure caused by a decrease in the contractility of the left ventricle, edema often develops with disturbances in heart rhythm/increased blood pressure, leading to a decrease in minute blood volume.
Tests and diagnostics
Diagnostic criteria are complaints of a sharp feeling of lack of air, dry/wet cough, and later the release of foamy sputum; a history of various heart diseases (CHF, ischemic heart disease, cardiomyopathy, hypertension) or non-cardinal causes.
Physical examination: The main signs of acute left ventricular failure include paroxysmal nocturnal dyspnea , orthopnea , bilateral pulmonary rales, wet cold extremities, dizziness , confusion , oliguria , low pulse pressure.
Possible signs of AHF: tachycardia (HR> 120 beats/min.)/ bradycardia (HR <40 beats/min.), blood pressure (systolic) <90 mm Hg. Art. RR>25/min. with the involvement of auxiliary muscles in the respiratory process.
Laboratory criteria for diagnosing cardiogenic pulmonary edema:
- Low oxygen saturation (pulse oximetry SaO2<90%).
- Hypoxemia (PaO2 levels in arterial blood <80 mmHg).
- Respiratory failure of the hypoxic type.
- Hypercapnia (PaCO2 > 45 mmHg in arterial blood).
- Respiratory failure of the hypercapnic type.
- Metabolic acidosis.
Instrumental methods:
- X-ray of the lungs - signs of pulmonary congestion.
- ECG - the presence of conduction disturbances, paroxysmal arrhythmias and ACS, signs of structural heart damage.
- Pulse oximetry - oxygen saturation <90%.
Differential diagnosis between cardiogenic and non-cardiogenic types of pulmonary edema is extremely important, since treatment methods and outcomes of the disease vary.
Prevention
Prevention of cardiogenic pulmonary edema comes down to early detection of diseases, the complication of which may be pulmonary edema and their timely and effective treatment. Of particular importance in the development of pulmonary edema are diseases such as hypertension , coronary heart disease , defects / arrhythmias , pulmonary emphysema , as well as bronchial asthma , which cause congestion in the lungs. Accordingly, it is important to both treat pulmonary congestion in elderly patients and monitor them constantly, taking into account the decrease in adherence of people in this age group to treatment.
Folk remedies
There are many “folk” methods for treating pulmonary edema. Among the recipes that should help relieve swelling, the most common are formulations based on the following plants:
- Cherry
- Linen
- Liquorice root
- Juniper fruits
- Lovage root
- Steelwort root
- St. John's wort
- Dog-rose fruit
- nettle leaves
- Plantain leaves
- bearberry leaf
These and some other plants in various proportions are offered to be brewed, steamed or infused. Such a solution should help in the treatment of pathology.
Some substances contained in these plants may indeed help relieve symptoms, but are not very effective as a primary treatment.
Consequences and complications
The consequences of cardiogenic pulmonary edema are associated primarily with hypoxia and hypercapnia . There is a risk of complications in the form of ischemic damage to brain cells, myocardial ischemia , congestive pneumonia , pulmonary atelectasis , which leads to somatic and cognitive disorders. With non-cardiogenic pulmonary edema, especially in cases of its rapid development, death from pulmonary edema reaches high rates.
What is dangerous, forecast
Pulmonary edema is a direct threat to life . Without taking extremely urgent measures, which must be carried out by the patient’s relatives, without subsequent urgent active treatment in the hospital, pulmonary edema is the cause of death in 100% of cases. A person will experience suffocation, coma, and death.
Attention! When the very first signs of an acute pathological situation appear, it is important to provide qualified assistance at a hospital as soon as possible, so an ambulance is called immediately.
Forecast
The prognosis for pulmonary edema, regardless of its etiology, is always extremely serious and depends on the timeliness and adequacy of the treatment. Cardiogenic pulmonary edema, with adequate therapy, resolves over several hours/days; non-cardiogenic edema is characterized in most cases by a longer course, and stabilization of the condition occurs more slowly, over several days or more. The prognosis largely depends on the etiology and the treatment and therapy provided. Thus, with acute myocardial infarction and the development of edema without adequate treatment, mortality reaches 50%, while at the same time, with adequate treatment, it decreases several times.
To a large extent, a favorable outcome is facilitated by pathogenetic therapy, begun already in the interstitial phase of edema, rapid identification of the underlying disease and its adequate treatment by specialists of the appropriate profile. It should be remembered that even in cases of successful relief of pulmonary edema, subsequent complications are possible in the form of congestive pneumonia, pneumosclerosis , pulmonary atelectasis , ischemic damage to internal organs . Also, there is a high probability of recurrence of swelling if its root cause is not eliminated. Treatment of non-cardiogenic pulmonary edema is more complex; long-term mechanical ventilation and respiratory support is required, as well as various measures to maintain the vital functions of the body. Mortality with non-cardiogenic edema exceeds 60%.
Treatment
Photo: nxstage.com
Since pulmonary edema is a life-threatening condition, treatment should be carried out in the intensive care unit (ICU). The person is given a sitting or semi-sitting position (with the head of the bed raised). If necessary, for example, to remove a foreign body or aspiration of contents from the respiratory tract, a tracheostomy is performed - dissection of the anterior wall of the trachea with subsequent creation of an artificial opening. This manipulation eliminates the factor that complicates breathing, which in some cases is an emergency. Next, oxygen is supplied. Subsequently, if the person continues to need a continuous supply of oxygen, in the ICU conditions the patient is transferred to mechanical ventilation. An artificial lung ventilation device (ventilator) provides a forced supply of a gas mixture into the lungs, due to which the blood is saturated with oxygen and carbon dioxide is removed from the lungs. To suppress the activity of the respiratory center, morphine, which is a narcotic analgesic, is used. To reduce the volume of circulating blood, as well as to achieve dehydration of the lungs, diuretics are administered. In addition, agents are used to reduce afterload on the heart, which also forms the basis for the treatment of pulmonary edema.
According to indications, the following groups of drugs may be prescribed:
- cardiac glycosides;
- antihypertensive drugs;
- antiarrhythmic drugs;
- thrombolytic agents;
- antihistamines;
- antibiotics.
After stopping the pathological process, the underlying disease that caused the development of pulmonary edema is treated. This is necessary because in the absence of appropriate treatment, the risk of developing a recurrent attack of pulmonary edema increases significantly.
List of sources
- Braunwald E. Acute pulmonary edema // Internal diseases / Ed. Braunwald E. Book. 5. Per. from English -Moscow: Medicine, 1995. P. 123-124.
- Inkova A. N. Handbook of emergency and emergency medical care doctors. Rostov n/a: Phoenix; M.: ACT, 2001. - 337 p.
- Stranshnov V.I., Voinov V.A. Respiratory distress syndrome. In: Koryachkin V.A., Strashnov V.I., eds. Intensive therapy of threatening conditions. St. Petersburg Medical Publishing House, St. Petersburg, 2002. 135 p.
- Vlasenko A.V., Ostapchenko D.A., Pavlov D.P. et al. Features of the pathogenesis and effectiveness of therapy for acute respiratory distress syndrome. Abstracts of reports of the XI Congress of the Federation of Anesthesiologists and Resuscitators of Russia 2008; 508-509.
- Acute respiratory distress syndrome in pediatric practice / Aleksandrovich Yu.S., Pshenisnov K.V. // Bulletin of intensive care. – 2014 – No3.
Tuberculosis
Many are still confident that tuberculosis is a thing of the past, in history and in Remarque’s novels, says Arkady Vertkin. Unfortunately, it is not. Russia is in third place in terms of the prevalence of this disease.
Another incorrect belief is that tuberculosis is a disease of people of special social status (people without a fixed place of residence, migrants released from prison, alcohol and drug abusers).
“These are indeed risk groups for infection with this disease, but, unfortunately, due to its widespread prevalence, tuberculosis can be contracted regardless of belonging to any social group - just look at the patients in TB departments,” the professor notes.
Symptoms:
- prolonged dry cough;
- constant low-grade fever (increase in temperature from 37.0 °C to 37.9 °C) or an increase in body temperature in the morning with the evening temperature curve returning to normal;
- sweating, especially at night;
- weight loss with preserved appetite;
- weakness, fatigue;
- generalized or limited enlargement of lymph nodes;
- hemoptysis.
Treatment is required; there should be no self-help, only examination and therapy prescribed by a doctor, so as not to aggravate the situation.
What is COPD and how to cope with chronic bronchitis? More details