Medicinal properties
The medication is considered one of the most effective antiviral drugs. It belongs to the synthetic analogues of nucleosides. When the active substance combines with the virus cell, it turns into a more active form and begins to affect the viral enzymes necessary to create conditions for reproduction. Thus, a more active component is introduced into the nucleotide chain of a harmful agent, thereby changing its DNA and preventing further reproduction. Treatment with a single HIV antiviral drug will not bring visible results; combinations must be used. For example, stavudine and didanosine, zidovudine and lamivudine or didanosine, etc.
After oral administration, the active substance is quickly absorbed by the body, regardless of food intake. Bioavailability is approximately 70-75%. The maximum concentration in the blood after use is reached within 30-90 minutes. Converts to a stronger and more active metabolite in the liver. The half-life is approximately 75 minutes, and in the presence of liver failure - from 30 to 240 minutes, depending on the degree of damage.
Overdose
Specific symptoms or signs of acute overdose of zidovudine, in addition to those indicated in the section “Adverse reactions” (increased nausea, headache, vomiting, occasional episodes of hematological changes), no. Є information about the loss when the level of zidovudine in the patient’s blood after taking an unknown amount of zidovudine exceeded the therapeutic level in more than 16 times, against short-term clinical drugs, biochemistry No original or hematological traces were identified.
In case of overdose, it is necessary to carefully monitor the patient for signs of toxicity (section “Adverse reactions”) and initiate appropriate supportive therapy.
Hemodialysis and peritoneal dialysis may have a negative effect on the elimination of zidovudine and may accelerate the elimination of its glucuronide metabolite.
Mode of application
The medication is taken orally, the standard dosage for adults is 600 mg of the substance, divided into several doses. It is necessary to take antiviral medicine only as part of complex therapy. It can be prescribed to children, but the dosage is strictly limited to the child’s live weight.
From 4 to 9 kg is prescribed at a rate of 12 mg per 1 kg, 2 times a day. From 9 to 30 kg – 9 mg per kilo of weight, 2 times a day. If your weight exceeds 30 kg, then you need to drink 300 mg 2 times a day. If the patient has a history of anemia or neutropenia, then the dosage is adjusted downward by the attending physician; in case of chronic renal failure, you need to drink 100 mg 3 times a day to maintain bone marrow function, erythropoietin is prescribed.
To prevent the transmission of HIV infection from mother to child in the womb, the drug is prescribed from the 14th week of pregnancy, 100 mg 5 times a day until the end of the gestation period. Before cutting the umbilical cord, you need to administer 2 mg of the drug per kilogram of body weight (intravenously), and then after birth the baby needs to take 2 mg per kilogram of the drug orally.
Features of good stagnation
Patients should be guarded against the immediate self-stagnation of other drugs (section “Interactions with other drugs and other types of interactions”).
We must inform you that treatment cannot be transmitted to other persons in case of physical contact or contact with contaminated blood. Therefore, it is necessary to practice safety at all times.
The drug does not prevent HIV infection, and the patient has no risk of developing diseases associated with suppressed immunity, including opportunistic infections and new infections. Although it has been established that the risk of development of opportunistic infections is changing, there is a lack of data on the development of swelling, including lymphoma. According to the data of treatment of patients with advanced stage of IL-illness, the risk of lymphoma development in them is the same as in patients who were not treated with zidovudine. In patients with the embryonic stage of IL-illness following treatment with zidovudine, there is a risk of developing unknown lymphoma.
VAGITYA, Yaki Paymayu Rizhennya about Lіkuvannya Zidovudin with a meta zbizhannya vil-transm to Ditini, Povinni nobility, Scho at the Vipadki, unnecessary to Lіkuvannya, Vil-Transmiya.
Hematological adverse reactions.
In patients with an advanced stage of IL-illness on aphids, zidovudine treatment can cause severe anemia (not earlier than 6 years of age, and sometimes earlier), neutropenia (after tea no earlier than 4 years of age, or even earlier) and leukopenia (which є secondary to neutropenia). It occurs more often when high doses are administered (1200–1500 mg/dose) and in patients with low bone marrow reserve before treatment, especially in advanced stages of IL-disease.
Carefully monitor hematological parameters. At an advanced stage of IL-illness, it is recommended to perform a blood test at least once every 2 months during the first 3 months of treatment and at least once every month thereafter. In patients with early stages of IL disease (if the bone marrow reserve is still sufficient), hematological side effects occur infrequently. Before the clinical stage of the patient, blood tests should be carried out earlier, for example, every 1–3 months.
With a decreased level of hemoglobin from 7.5 g/dl (4.65 mmol/l) to 9 g/dl (5.59 mmol/l) or the number of neutrophils from 0.75×109/l to 1.0×109/ l It may be necessary to change the dose until signs of cystic cord renewal appear; Another way to speed up your workout is to take a short (2-4 days) break from zidovudine treatment. Renewal of the bone marrow is achieved after 2 days, after which zidovudine therapy can be restarted at reduced doses. In cases of severe anemia, changing the dose of zidovudine does not exclude the need for blood transfusions (section “Contraindications”).
Lactic acidosis.
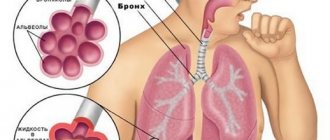
When nucleoside analogues are ingested, episodes of lactic acidosis are reported, which are associated with hepatomegaly and hepatic steatosis. Before early symptoms (symptomatic hyperlactatemia), there are mild gastroenterological symptoms (nausea, vomiting and abdominal pain), nonspecific illness, loss of appetite, loss of body weight, respiratory symptoms (Swedish and/or deep breathing) or neurological symptoms (including rotary weakness).
Lactic acidosis has a high mortality rate and may be associated with pancreatitis, hepatic or nitric insufficiency.
Lactic acidosis occurs after many months of treatment.
In case of symptomatic hyperlactatemia and metabolic lactic acidosis, progressive hepatomegaly or rapid elevation of aminotransferase levels, treatment with nucleoside analogues is necessary.
Nucleoside analogues should be used with caution for the treatment of any patients (especially obese women) with hepatomegaly, hepatitis or other relevant factors that risk liver disease and hepatic steatosis (including and medicinal practices and alcohol). There is a particular risk for patients who are infected with hepatitis C and who are treated with alpha-interferon and ribavirin.
It is necessary to keep a close eye on patients who may have advanced developmental risks.
Impaired mitochondrial function
Nucleoside and nucleotide analogues can cause disruption of the function of mitochondria at various stages, which is especially noticeable when combined with stavudine, didanosine and zidovudine. There were reports of episodes of mitochondrial dysfunction in VIL-negative patients, who recognized the influx of nucleoside inhibitors in the intrauterine and/or postnatal period, the main focus was on treatment regimens, which included zidovudine. The main adverse reactions that have been reported include hematological disorders (anemia, neutropenia) and metabolic disorders (hyperlactatemia, hyperlipasemia). These boxes were often transient. There have rarely been reports of neurological disorders (hypertension, seizures, behavioral disturbances) that occurred after the drug was discontinued. Whether such neurological damage is transient or permanent is still unknown. It is possible to understand the possibility of such disorders in the skin of a child, when nucleoside and nucleotide analogues were infused in the intrauterine period, with severe clinical disorders of unknown etiology, especially neurological. This data does not coincide with current recommendations for the use of antiretroviral drugs to prevent the vertical transmission of VIL.
Lipoatrophy
Treatment with zidovudine is associated with loss of subcutaneous fat, which is associated with mitochondrial toxicity. The frequency and severity of lipoatrophy is associated with cumulative influx. This loss of fat deposits, which is most clearly visible on the face, ends and sides, can be non-negotiable when switching to a treatment regimen without zidovudine. Patients should be regularly assessed for signs of lipoatrophy during therapy with zidovudine and zidovudine-containing drugs. If there is a strong suspicion of the development of lipoatrophy, it is necessary to transfer the patient to an alternative treatment regimen.
Body mass and metabolism parameters
Body weight, blood serum lipids and blood glucose levels may improve with antiretroviral therapy. Factors in play in some countries may also include disease control and a change in lifestyle. There is no confirmation of the influx of treatment on an increased level of lipids in certain seizures, while there is no confirmation of the infusion of treatment on an increased level of body weight. Monitoring of blood serum lipids and blood glucose is routinely carried out before the confirmation of HIV treatment protocols. Treatment of disorders associated with changes in the level of lipids is followed by clinical indicators.
Liver ailments.
The clearance of zidovudine in patients with mild liver failure without cirrosis (5–6 points on the Child–Pugh scale) is similar to that observed in healthy volunteers, so there is no need to change the dose of zidovudine. For patients with mild to severe hepatic insufficiency (7–15 points on the Child–Pugh scale), specific dosage recommendations cannot be made due to the wide variability in exposure to zidovudine, However, it is not recommended to administer zidovudine to this group of patients.
Patients with chronic hepatitis B or C who are treated with combination antiretroviral therapy may be at increased risk of developing severe and potentially fatal similar effects on the side of the liver. In case of medical treatment with other antiviral drugs for the treatment of hepatitis B and C, please refer to the relevant instructions for medical treatment of these drugs.
Patients with already obvious impaired liver function, including chronic active hepatitis, may be at risk of impaired liver function under combined antiretroviral therapy and may be under medical supervision. Once a sign of worsening liver disease appears in such patients, it is important to take a break or take a regular bath (section “Method of administration and dosage”).
Immune renewal syndrome.
In HIV-infected patients with severe immunodeficiency, treatment with antiretroviral drugs may result in the development of an asymptomatic or residual opportunistic infection, which can cause severe clinical stage or worsening of symptoms.
Such reactions may occur during the first year or months of treatment with antiretroviral drugs. Common causes of this include retinitis, caused by cytomegalovirus, generalized or focal infections, caused by mycobacteria or Pneumocystis jiroveci (P. Carinii) pneumonia
. Any ignition boxes must be traced without obstruction and, if necessary, they must be cleaned. During the period of immune regeneration, the occurrence of autoimmune disorders (such as Graves' disease, autoimmune hepatitis, polyomyositis and Guien-Barré syndrome) was also reported, although their origin is more variable and may cause and many months after the beginning of the treatment and sometimes the atypical picture.
Patients with rare episodes of fructose intolerance are guilty of stagnation of oral intake.
Osteonecrosis
. Although the etiology of osteonecrosis is considered to be multifactorial (including depletion of corticosteroids, alcohol abuse, severe immunosuppression, high body mass index), episodes of osteonecrosis were reported primarily in patients with advanced with ailments and/or with long-stagnant combination antiretroviral therapy. Patients should be advised of the need to seek medical help whenever pain, stiffness in joints or rashes occurs.
Patients infected with the hepatitis C virus.
Acute anemia associated with zest-supplemented ribavirin was observed in patients who took zidovudine in a complex regime for the treatment of HIV, although the exact mechanism of this phenomenon is unclear. It is not recommended to take ribavirin and zidovudine. The doctor must replace zidovudine with another type of combination antiretroviral therapy if it is already prescribed. This is especially important for patients with a history of known zidovudine-induced anemia.
Suspension during pregnancy or breastfeeding.
Vaginism
Make decisions about the use of antiretroviral agents for the treatment of HIV infection in pregnant women and to reduce the risk of vertical transmission of HIV to the newborn, take into account the data taken from the investigations on animals nah, as well as clinical evidence of the stagnation of female women.
In this stage, administration of zidovudine to the pregnant woman with further treatment of the newborn changes the frequency of transmission of VIL from the mother to the fetus. A large number of data from these pregnant women (over 3000 results obtained during the first trimester, and more than 3000 results obtained during the second and third trimester) indicate the prevalence of malformative toxicity. Zidovudine can be frozen during pregnancy, if it is clinically primed. The risk of birth defects in people is low, coming from a large number of data.
Data from studies of zidovudine in animals indicate reproductive toxicity. Active storage drugs can inhibit cell DNA replication, and zidovudine has shown transplacental carcinogenic potential in one study in animals. The clinical significance of these results is unknown. The transplacental penetration of zidovudine into the human body has been established.
Mitochondrial dysfunctions: nucleotide and nucleoside analogues in vitro
and
in vivo
cause damage to mitochondria. There has been no information about impaired mitochondrial function in VIL-negative babies whose mothers were treated with nucleoside analogues during pregnancy and/or in the postnatal period (section “Peculiarities of stagnation”).
Fertility
Zidovudine did not reduce human fertility or reduce fertility in squirrels, who were administered a dose of up to 450 mg/kg per dose. There is no data about the infusion of zidovudine for women's fertility. In humans, zidovudine does not affect the size, morphology or friability of sperm.
Breast bath period
After administration of a single dose of 200 mg zidovudine to HIV-infected women, the mean concentration of zidovudine was similar to that of breast milk and blood syringes. It is recommended that HIV-infected women, under any circumstances, be aware of breastfeeding as a means of preventing the transmission of HIV infection to children.
This is due to the fluidity of the reaction during treatment with vehicles or other mechanisms.
Investigations of the infusion of zidovudine on the fluidity of the reaction during treatment by motor transport or robots using other mechanisms were not carried out. The pharmacology of zidovudine does not allow any negative effects to occur. Ale, regardless of the situation, you should always call the patient to the final stage and the profile of side effects of the drug with high nutrition about the possibility of ending these types of activities.
Side effects
Gastrointestinal tract: nausea, vomiting, gas, diarrhea, stomach pain, yellowing of the skin, refusal to eat.
Blood: thrombocytopenia, anemia, bone marrow hypoplasia.
Systemic phenomena: edema, hearing loss, rash, urticaria, scabies.
CNS: dizziness and migraine, depression, convulsions, drowsiness, lethargy, difficulty falling asleep.
Respiratory system and heart: cardiomyopathy, cough, runny nose, shortness of breath, sinusitis.
Other reactions: gynecomastia, muscle pain, flu-like condition, fever, myalgia, amblyopia, frequent bladder urge, increased sweating.
Overdose
As for an overdose of Lamivudine-Zidovudine, the instructions for use state that cases of increased adverse reactions are common, but no deaths have been reported.
It is important that the health status of a patient suffering from human immunodeficiency virus is closely monitored. In some cases, a continuous course of hemodialysis may be required.
To eliminate any adverse reactions that may occur, the following measures can be taken:
- gastric lavage,
- use of adsorbents,
- prescription of symptomatic drugs.
Unfortunately, hemodialysis is ineffective in this case, but it can accelerate the elimination of the glucuronic metabolite.
The purchased medication should be stored in a dark and dry place, out of reach of children, where the air temperature does not exceed twenty-five degrees Celsius.
The use of the medicine is permitted for two years from the date of release, after which it is strictly prohibited to use it.
Zidovudine + Lamivudine is available in pharmacies only with a doctor's prescription.
Analogs
Zeffix
Glaxo Wellcome Operation, UK
The average price in Russia is 3,000 rubles per package.
The active ingredient in Zeffix is lamivudine. It has similar pharmacological properties to its analogue, but is prescribed purely for therapy as part of the complex composition of viral hepatitis B. It is available in tablet form.
Pros:
- Convenient release form
- An effective drug.
Minuses:
- Expensive
- Has a narrow focus in treatment.
Lamivudine
Aurobindo Pharma, India
The average price in Russia is 2200 rubles.
It is a complete analogue of the active substance of Zeffix. Release form: tablets. Can be prescribed as part of complex treatment of HIV infection.
Pros:
- Effective
- Suitable for the treatment of HIV and hepatitis.
Minuses:
- Expensive, hard to find on sale
- Not suitable for everyone.
Use during pregnancy and lactation
Safety during childbearing has not been fully studied to this day. However, you should not use Zidovudine + Lamivudine for the first three months. But an exception may be a situation when the benefits for the expectant mother are higher than the possible negative consequences for the baby.
Treatment with medication during pregnancy and further use for newborns has been proven to reduce the likelihood of transmitting a dangerous virus.
In medical practice, there have been situations when, after using Zidovudine with Lamivudine, the following conditions were identified:
- delay in fetal development,
- neurological disorders,
- convulsions.
Doctors do not recommend infected women to breastfeed, as this significantly increases the risk of infecting the baby.
But not only for this reason, Zidovudine + Lamivudine cannot be used during lactation, another reason is the penetration of the active ingredients of the drug into the milk, which enters the fragile body, which can provoke negative consequences.