Still's disease is an inflammatory disease that affects multiple organ systems. This is a very rare pathology that is diagnosed in only 1 in 1000 people. However, it progresses in only one in 10 thousand patients. The incidence of infection in men and women is approximately the same; most often the disease affects children under 16 years of age.
Attention was first paid to this symptom complex in 1886. Due to the similarity of symptoms, the pathology was considered one of the varieties of rheumatoid arthritis. A year later, George Still began researching the disease. In 1897, he classified it as seronegative chronic polyarthritis in combination with a systemic inflammatory process. Later, in 1971, the pathology was named Still's disease/syndrome.
Characteristics of the disease
This disease was first described at the end of the 19th century. Since it occurs most often in adolescents and young adults, the British doctor George Still, who discovered such symptoms, classified it as a form of juvenile rheumatoid arthritis. He described similar symptoms in more than two dozen children, and the disease was later named after him. And only in the 70s of the 20th century it was confirmed that Still's disease also occurs in adults.
The etiology of the disease is poorly understood, and it is quite difficult to diagnose it. Based on clinical signs, patients are often first diagnosed with sepsis or fever of unknown origin. But it is very important to start adequate treatment as early as possible so that complications do not develop. This disease refers to systemic diseases that negatively affect the entire body.
Affected Populations
The adult form of Still's disease affects men and women in equal numbers. Some medical literature suggests that the disorder affects women slightly more often than men. This primarily concerns young people aged 16 to 35 years. The incidence of the disease in adults is still unknown. Due to the highly variable symptoms and rarity of the disorder, it is often underdiagnosed or misdiagnosed, making it difficult to determine its true incidence in the general population.
Causes
Despite more than a century of research into the disease, it has still not been possible to find out exactly what causes it. Most symptoms of Still's disease indicate an infectious origin. This is indicated by a sudden onset, high temperature and enlarged lymph nodes. But there is no single pathogen; the cause may be viral or bacterial diseases. Most often, Still's disease develops against the background of such infections:
- rubella;
- cytomegalovirus;
- parainfluenza;
- Epstein-Barr virus;
- mycoplasmosis;
- Escherichia;
- The disease may appear after a sore throat or pharyngitis.
In some cases, patients have been found to have a connection with autoimmune pathologies or a hereditary predisposition. It is believed that disruption of the endocrine system may also influence the onset of the disease. But these are all unconfirmed causes of Still's disease, as they rarely cause it.
Still's disease was first thought to be a form of juvenile rheumatoid arthritis because it often occurs in children.
Cytostatics and biological drugs
Cytostatic drugs include Methotrexate, Arava, Remicade, Equoral, Cyclophosphamide and many other drugs. Most often used in the treatment of juvenile rheumatoid arthritis:
- Methotrexate. “Gold standard” in the treatment of diseases of the musculoskeletal system. The required dosage is selected individually, but on average it is enough to take 1 tablet every 7 days. The effect of its use develops after 5-6 weeks from the start of use. The maximum concentration of the substance in the blood is reached after 6-12 months.
- Arava. Prescribed in case of side effects from taking Methotrexate. Begins to act in 4-6 weeks.
- Remicade. It has a faster therapeutic effect, but has a fairly large list of contraindications. It is used only in the absence of proper results from taking other basic drugs. Requires simultaneous administration of antihistamines, as it can provoke the development of an allergic reaction.
Biological drugs quickly and very effectively relieve inflammation. However, they also have some disadvantages. They can only be used in a hospital setting, since this group of drugs must be administered under the supervision of a physician. The duration of drug administration ranges from 30 minutes to 2 - 3 hours, depending on the chosen dosage. This group of medications includes:
- Etanercept. Provides an increase in the transport of leukocytes to the site of the inflammatory process, thereby enhancing the immune response.
- Anakinra. Has an inhibitory effect on Interleukin-1. As a result, the activation of inflammatory cells becomes impossible.
- Orence. It is the drug of choice in case of ineffectiveness of other basic drugs, in particular Methotrexate. Often used in the treatment of children.
- Actemra. Neutralizes Interleukin-6, which is one of the main mediators of inflammation. Used as monotherapy or combined with Methotrexate.
- Rituximab. Reduces the number of lymphocytes and prevents the progression of the inflammatory process.
Sources
- https://okeydoc.ru/bolezn-stilla-u-vzroslyx-iu-detej-simptomy-lechenie/
- https://www.neboleem.net/bolezn-stilla.php
- https://diartroz.ru/artrit/revmatoidnyy-artrit/bolezn-stilla-i-felti.html
- https://NogivNorme.ru/bolezni/artrit/vidy-artritov/bolezn-stilla.html
- https://medbe.ru/materials/klinicheskie-rekomendatsii/bolezn-stilla-u-vzroslykh/
- https://www.syl.ru/article/299139/bolezn-stilla-prichinyi-simptomyi-diagnostika-i-osobennosti-lecheniya
- https://lechenierebenka.ru/bolezn-stilla-u-detej/
- https://sustavy-lechenie.ru/bolezn-stilla-vzroslykh-detey-priznaki-simptomy-lechenie/
- https://liqmed.ru/disease/bolezn-stilla/
- https://DetStrana.ru/service/disease/children/bolezn-stilla/
- https://OrtoCure.ru/kosti-i-sustavy/artrit/bolezn-stilla-u-vzroslyh.html
Symptoms
It is difficult to immediately diagnose this pathology based on external manifestations, since similar signs are found in many infectious and inflammatory diseases. But some characteristic symptoms of Still's disease can be identified. True, a diagnosis can be made only on the basis of external signs if they last for at least 2-3 weeks.
The most important symptom of Still's disease is fever. A rise in temperature to high values – 39-40 degrees – does not occur in the same way as in most infectious and inflammatory diseases. The patient may feel well all day, and only in the evening does he develop a high fever with increased sweating and chills. Some patients may have a fever twice a day. But it decreases after some time after taking antipyretics or even without medications. It is also characteristic that in children the temperature rises to higher numbers, and the older the patient, the less pronounced his fever. In very rare cases, the temperature can remain constant without being affected by antipyretics.
The same thing happens with another characteristic symptom of Still's disease - a rash. Rashes on the patient’s body appear periodically, along with a rise in temperature. Most often, the rash appears as small, flat pink spots covering the limbs and torso; very rarely it occurs on the face. Sometimes the rashes are more noticeable, rise above the body and appear in places where the skin is subject to pressure from clothing or trauma, such as scratching. This is the so-called Koebner syndrome. The rash may be itchy, but most patients do not notice it at all. To detect it, it is sometimes necessary to expose the body to heat, for example, examining the patient after a shower.
A small pinkish rash on the body and limbs is a characteristic symptom of the disease
The last characteristic symptom of Still's disease is joint damage and myalgia. At first, inflammation is observed in one joint, but as the disease progresses, polyarthritis develops. It is characteristic that the interphalangeal joints of the hand are necessarily affected. The cervical spine and knees are often affected. It is this symptom that makes it possible to distinguish Still’s disease from the juvenile form of rheumatoid arthritis, because in children the hands are very rarely affected.
Inflammation is accompanied by severe pain in the joints and muscles, swelling, and accumulation of fluid in the joint cavity. In the later stages of the disease, muscle atrophy and severe stiffness in movements may be observed. In severe cases, it is possible to develop osteoporosis of the bones and ankylosis of the wrist joint with a complete loss of its mobility.
The disease often affects the patient's lymphatic system. The cervical lymph nodes become inflamed - they become enlarged and have a moderately dense consistency. Most patients also complain of pain and sore throat. This symptom appears at the beginning of the disease and is usually permanent. This pain is characterized by a burning sensation in the throat. Apathy, decreased appetite, abdominal pain, nausea and vomiting, and enlarged liver and spleen may also be observed. The inflammatory process in the joints is often accompanied by general intoxication and exhaustion of the body, hair loss, hearing and vision impairment.
More rare symptoms of the disease include pathologies of the cardiovascular and bronchopulmonary systems. If the patient is bothered by cough, shortness of breath, or chest pain, consultation with a cardiologist and pulmonologist is necessary. Tachycardia, vegetative-vascular dystonia, hypotension, pericarditis, pleurisy or bilateral pneumonia may develop. Sometimes the myocardium and valvular system of the heart are affected, manifesting as myocarditis or endocarditis. Moreover, these pathologies develop even despite the use of antibiotics. It is because of such complications that the disease most often ends in death.
Often with Still's disease, the cervical lymph nodes become enlarged and the throat hurts severely.
Symptoms and treatment of Still's disease in adults
Most people with Still's disease have the following signs and symptoms:
Fever. There may be a daily fever of at least 38.9 C for a week or longer. Fever usually peaks in the afternoon or early evening. You may have two bouts of fever each day, and the temperature only returns to normal between bouts.
Rash. The pinkish rash may come and go after a fever. The rash usually appears on the torso, arms, or legs.
Angina. This is one of the first symptoms of Still's disease. The lymph nodes in the neck become enlarged and painful.
Unhealthy and swollen joints. Your joints—especially your knees and wrists—become stiff, painful, and inflamed. Ankles, elbows, arms and shoulders may also hurt. Joint discomfort usually lasts two weeks.
Muscle pain. Muscle pain usually comes and goes with a fever, but the pain may be so severe that you stop doing daily activities.
The signs and symptoms of this disorder resemble other diseases, including lupus and a type of cancer called lymphoma.
When to see a doctor
If you have a high fever, rash, and unhealthy joints, see your doctor. Also, if you have Still's disease and develop a cough, difficulty breathing, chest pain, or other unusual symptoms, call your doctor.
Causes
There is no certainty about what causes Still's disease. Some researchers suggest that it is caused by a viral or bacterial infection.
Risk factors
Age is the main risk factor for the disease, which appears twice: from 15 to 25 years and again from 36 to 46 years. Men and women can get sick equally.
Complications
Most complications from Still's disease result from chronic inflammation of organs and joints.
Joint destruction. Chronic inflammation can damage your joints. Knees and wrists are usually affected. Your neck, legs, fingers and hip joints may also be affected, but less frequently.
Inflammation of the heart. Still's syndrome in adults can cause inflammation of the lining of the heart (pericarditis) or the muscle part of the heart (myocarditis).
Excess fluid around the lungs. Inflammation may cause fluid to build up around the lungs, making it difficult to breathe deeply.
Macrophage activation syndrome. This rare but potentially fatal complication of adult Still's disease can cause low blood cell counts, very high triglyceride levels and abnormal liver function.
Diagnosis
No single test defines Still's syndrome. Imaging can show the damage caused by the disease, while blood tests can help rule out other diseases with similar symptoms.
Treatment
Doctors use many medications to treat Still's disease. The type of medication you take depends on the severity of your symptoms and whether there are any side effects.
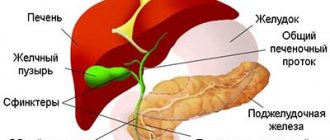
Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter NSAIDs such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve) may help with mild joint pain and inflammation. Stronger NSAIDs are available by prescription only. NPP can damage the liver, so you may need regular blood tests to check your liver function.
Steroids. Most people with Still's disease require treatment with steroids, such as prednisone. These powerful drugs reduce inflammation, but may reduce your body's resistance to infection and increase your risk of developing osteoporosis.
Methotrexate. Methotrexate is a drug that is often used in combination with prednisone, which allows the dose of prednisone to be reduced.
Biological response modifiers. Drugs such as infliximab (Remicade), adalimumab (Humira), and etanercept (Enbrel) have shown some improvement, but their long-term benefits are still unknown. If other medications haven't helped, your doctor may suggest trying anakinra (Kineret), tocilizumab (Actemra), or rituximab (Rituxan).
Diagnostics
Since there are no pronounced symptoms on the basis of which a diagnosis can be made immediately, the patient often has to be observed for a long time and examined to exclude other diseases. Typically, blood tests reveal an accelerated ESR, elevated protein levels, anemia, and increased liver enzyme activity in the patient. These signs are common to all infectious diseases, but a feature of blood tests for Still's disease is the absence of microorganisms.
An x-ray examination of the joints is also carried out for diagnosis, which can show swelling of the soft tissues and osteoporosis of the bones. Synovial fluid shows signs of an inflammatory process. To rule out other diseases, it is often necessary to do a lymph node biopsy, chest X-ray, ECG, ultrasound and other examinations. It is necessary to differentiate Still's disease from rheumatoid arthritis, tuberculosis, lymphoma, infective endocarditis, rheumatism, sepsis, sarcoidosis, and vasculitis.
It is very important to differentiate Still’s disease from other diseases in time and prescribe the correct treatment
Methods of therapy
The goals of treatment for Still's disease are:
- pain relief;
- prevention of systemic lesions;
- improving the patient's quality of life;
- prevention of re-development of pathology.
They are achieved through a complex effect on the disease. It includes:
- General recommendations that include:
- weight loss;
- exercise therapy;
- quitting smoking and alcohol;
- prevention of acute infectious diseases.
- Medication prescriptions.
- Physiotherapeutic procedures: electrophoresis, magnetic therapy.
- Therapeutic massage when the acute inflammatory process subsides.
Only a rheumatologist determines a treatment regimen with specific medications, dosages and frequency of administration! For medicinal effects on the manifestations of Still's disease, 3 groups of drugs are used:
- Non-steroidal anti-inflammatory NSAIDs:
- Nimulid, Nise, Nimika;
- Movalis;
- Naproxen;
- Aertal.
Prescribed for a long term at all stages of the disease. If there is a history of peptic ulcer disease, then they are combined with proton pump inhibitors (Omez, Lancid).
- Glucocorticosteroids – Metypred, Prednisolone. Indications for their use:
- advanced and late stage;
- intolerance to NSAIDs;
- exacerbation of gastric or duodenal ulcer;
- ineffectiveness of the main therapy.
The duration of their use varies individually, but on average is up to 3 months. Abrupt discontinuation of this group of medications is contraindicated, which is associated with a high risk of worsening the condition. The dosage is reduced gradually.
Rheumatologists call the administration of hormones at the same time as starting basic medications as bridge therapy.
- Immunosuppressive drugs are prescribed in the presence of systemic lesions and severe joint deformities for a long period. For Still's disease it is recommended:
- Methotrexate, Methoject (at the same time, taking folic acid is indicated, which reduces the risk of developing undesirable effects);
- Cyclophosphamide;
- Remicade (has fewer adverse reactions and a high price category).
The listed drugs are called basic. When taking them, laboratory monitoring of general blood parameters is required. If there is a marked decrease in red blood cells, hemoglobin, platelets or leukocytes, then medications are temporarily discontinued.
ARVE Error: id and provider shortcodes attributes are mandatory for old shortcodes. It is recommended to switch to new shortcodes that need only url
Of secondary importance is the use of metabolic drugs that improve blood circulation and nutrition in damaged structures. These include injections of Pentoxifylline, Trental, Nicotinic acid. They are used in hospitals in the absence of contraindications.
Treatment
There are no specific drugs against Still's disease. Antibacterial therapy, which is often used in the initial stages of the disease, turns out to be ineffective. Therefore, it is best to use non-steroidal anti-inflammatory drugs and glucocorticosteroids, which must be taken for at least 3 months. The choice of drug depends on the severity of the disease and the symptoms manifested.
Treatment of Still's disease consists of relieving the symptoms of the disease, alleviating the patient's condition and preventing complications. In the chronic course of the disease, it is important to prevent relapses, so taking medications prescribed by a doctor must be constant. What drugs are most often used to treat Still's disease:
- nonsteroidal anti-inflammatory drugs help relieve pain and reduce fever, these can be Ibuprofen, Ketanov, Naproxen and others;
- for complications of the heart and respiratory system, Methylprednisolone, Dexamethasone or other corticosteroids are prescribed;
- in the chronic course of the disease, Methotrexate is used, sometimes Anakinra;
- in severe cases, Cyclophosphamide, which inhibits cell growth, may be prescribed;
- special drugs are also used to treat complications of damage to the liver, heart and lungs;
- if the patient is refractory to conventional treatment, Etanercept or Infliximab are sometimes used - modern drugs that quickly suppress the inflammatory process.
During treatment, you must follow all the doctor’s recommendations and do not stop taking your medications, even if your condition has stabilized. But with such long-term use of NSAIDs and glucocorticosteroids, it is necessary to monitor liver function. In addition, such drugs reduce immune defense and can cause dysbiosis. It is also very important to ensure additional intake of calcium and vitamin D into the body. Therefore, in addition to taking special vitamin supplements, you also need to follow a special diet rich in dairy products and fish. To prevent the development of joint immobility, physical therapy is necessary.
Sometimes patients with severe joint damage require surgical treatment. The most common operation is hip replacement, because when inflammation affects the hip joint, there is often severe limitation of mobility.
Still's disease often causes complications in the heart and lungs
Pathogenesis
The main mechanism of the pathogenesis of the disease is considered to be increased production of pro-inflammatory cytokines due to the high activity of T-helper type 1 and low suppressive activity of T-helper type 2, which leads to the release of tumor necrosis factor, which stimulates the synthesis of interleukins (IL) IL-1 and IL-6 , acting on the thermoregulatory center in the hypothalamus. Under the influence of IL-1, there is an increase in hematopoiesis, the production of acute phase proteins in the liver and endothelial proliferation, and under the influence of IL-6, osteoclast activation occurs [1]. The main forms of EFS are self-limiting (monocyclic), intermittent (polycyclic) and chronic articular [2].
Forecast
The disease sometimes goes away on its own, but can become chronic or recurrent. The disease lasts a long time, usually from 6 to 10 months. Most patients either recover completely or experience another relapse, which may occur within the next 10 years. But quite often, even after recovery, serious complications occur. Many patients remain disabled due to joint damage.
But a small number of patients suffer from a chronic form of the disease. It is characterized by severe polyarthritis with obligatory damage to the joints of the hands. It is accompanied by severe limitation of mobility, osteoporosis or ankylosis. If left untreated, Still's disease can be fatal. But patients die mainly from complications: amyloidosis, heart failure, tuberculosis, renal failure, bleeding disorders, liver damage, and secondary infections.
Complications of the disease
If Still's disease is left untreated, it can cause serious complications:
- Ankylosis. The articular ends of adjacent bones fuse together, causing the joint to become immobile.
- Contracture. A condition in which it is impossible to bend or straighten a part of the body in one or several articular joints.
- Chronic renal failure resulting from renal amyloidosis. With amyloidosis, carbohydrate-protein metabolism in the kidneys is disrupted, due to which amyloid begins to be deposited in the organ. As a result, nephrotic syndrome develops and the kidney ceases to function normally.
- Osteoporosis. Due to Still's disease, bone density is significantly reduced, making them more fragile and susceptible to fractures.
- Uveitis and subsequent loss of vision.
- Disability. Due to the pathological process in the joints, a person becomes immobile. He loses his ability to work and the ability to move freely without assistance.
High-quality and timely treatment can protect the patient from complications of pathology.
Prevention
Still's disease or its recurrence after recovery can be prevented by hardening the body and strengthening the immune system. We must try to prevent the development of infectious diseases, get vaccinations on time, and sanitize the oral cavity. If a person has suffered from this disease, then he must follow all the doctor’s recommendations. Most often, they include taking special medications in spring and autumn, preventing infectious diseases, and general strengthening measures.
This pathology is quite rare. But since the disease is severe, often causes complications and leads to disability, it is very important to prevent inflammation. And at the first signs, do not self-medicate, but get examined by a doctor.
Set of diagnostic techniques
Although the signs of the disease are numerous, diagnosing it in the early stages is quite difficult. The patient is usually monitored by a rheumatologist. A sufficient number of laboratory tests are carried out. A blood biochemistry test gives a result in which an increase in the amount of proteins can be observed. In this case, factors such as antinuclear and rheumatoid are completely absent. The liver increases its activity, which can be seen by testing it for biochemistry.
On the left is a healthy arm, on the right is one affected by Still's disease. A biopsy of the lymph node shows an uncharacteristic lesion that is metastatic in nature. When performing a puncture of the joint through the synovial fluid, characteristic changes associated with the inflammatory process can be observed. The X-ray picture allows you to determine the presence of tissue swelling, effusion in the joint, and sometimes osteoporosis. There are two types of diagnostic criteria. Several of both types must be present to make an accurate diagnosis. Large:
- Leukocytosis;
- Still's rash or some of its other types;
- Fever that lasts at least a week;
- Manifestation of arthralgia within two weeks.
Small:
- Lymphadenopathy;
- A sore throat;
- Antinuclear or rheumatoid factors are negative;
- Liver dysfunction.
Clinical observation
We presented a clinical observation of a conscript soldier transferred to the faculty therapy clinic of the Military Medical Academy from the infectious diseases department of the hospital. The main purpose of the demonstration was to show how difficult a differential diagnostic search can be to verify the diagnosis in a patient with fever of unknown origin and what are the features of the therapy carried out in patients with autoinflammatory diseases using the example of EFS.
Patient S., born in 1999, was admitted to the faculty therapy clinic of the Military Medical Academy on December 02, 2019 with complaints of a periodic feeling of chills, dry throat, pain in the muscles of the thighs and legs on both sides against the background of an increase in body temperature to febrile levels, weight loss of 4 kg for a month. I considered myself sick since November 7, 2019, when, against the background of absolute well-being, I felt chills and a sore throat. He contacted the medical service of the unit, an increase in body temperature was detected to 37.5 ° C, he was hospitalized in the infirmary with a diagnosis of “acute respiratory disease”, and received treatment: benzylpenicillin 1 million units. 4 rubles/day, antiviral and antipyretic drugs. No positive dynamics were observed. Temperature rises up to 40.2 °C were noted. The patient was transferred to the infectious diseases department of a military hospital, where the diagnosis of an acute respiratory disease of the type of moderate-severe pharyngotracheitis was verified. He received combined antibacterial therapy (cephalosporins, meropenem), symptomatic anti-inflammatory and antipyretic therapy. During treatment, no changes in the clinical picture were noted.
At this stage of the diagnostic search, the following studies were performed: fibroesogastroduodenoscopy (FGDS), computed tomography (CT) of the paranasal sinuses, CT of the chest, CT of the abdominal organs, ultrasound of the abdominal cavity, consultations with a dentist, phthisiatrician, ENT doctor, hematologist, rheumatologist. During the examination, the cause of the fever was not identified. According to CT of the chest, there was a slight increase in intrathoracic (paratracheal and para-aortic) lymph nodes, as well as the presence of pleuroapical and pleurodiaphragmatic adhesions on both sides. During this period, the patient had an episode of small-spotted rashes on the skin of the torso, which resolved on its own. The diagnosis remained unclear. It was decided to transfer the patient for further examination and treatment to the Faculty Therapy Clinic of the V.Med. CM. Kirov, where he was from 12/02/2019 to 12/29/2019. Diagnosis upon transfer: Fever of unknown origin, leukemoid reaction of the myeloid type, mild normocytic anemia, secondary nephropathy of toxic origin, chronic gastritis, functional disorder of the gallbladder.
On the first day (12/03/2019) in the Faculty Therapy Clinic of the VMedA named after. CM. Kirov continued to have febrile fever, which was relieved by taking paracetamol. Also, at the height of the fever, the patient began to complain of pain in the muscles of the thighs and legs. An objective examination revealed single vesicular elements with surrounding hyperemia on the mucous membrane of the soft palate, and local soreness in the muscles of the thighs and legs was determined by palpation.
Changes were noted in the general blood test: leukocytosis - 15.0 × 109/l, neutrophilia - 83%, band neutrophils - 6%, metamyelocytes - 0.5%, myelocytes - 2%, lymphopenia - 6.5%, ESR - 66 mm/h In the general urine analysis, changes were recorded: hyaline casts - 0-1 in the field of view (in the field of view), leukocytes - 5-7-8 in the field of view, changed erythrocytes - 5-10 in the field of vision, epithelial cells - 3- 4 in p/z. Urine sample according to Nechiporenko: erythrocytes - 21.0 × 106 / l, leukocytes - 10.5 × 106 / l. Procalcitonin - 0.220 ng/ml. Also noteworthy was the increase in the level of transaminases (AST - 85.9 U/l, ALT - 101.7 U/l) and creatine kinases (CK - 379.38 U/l, CPK MB - 8 U/l), the latter was considered as a result of multiple intramuscular injections. Dysproteinemia was noted (decrease in albumin level to 29.3 g/l, increase in globulin level to 45.7 g/l with a predominance of the α-2 fraction) and high acute-phase activity: ESR - 66 mm/h, CRP - 175.7 mg/ l, ferritin - 749 ng/ml, fibrinogen - 10.3 g/l. Over the next 4 days, no positive dynamics were observed. During the period of examination and diagnosis, symptomatic antipyretic, hepato- and gastroprotective therapy was carried out. The patient continued to complain of chills and a feeling of heat against the background of periodic febrile fever.
In order to verify the diagnosis, a set of measures was carried out to exclude infectious, oncological, hematological diseases, endocrine and autoimmune pathologies. The procalcitonin level was 0.220 ng/ml; Three times blood culture at the height of fever did not give growth of microflora. The results of the indirect hemagglutination test for coliform bacteria were negative; Diaskintest® was negative. A serological blood test using enzyme-linked immunosorbent assay showed positive results for IgG to the nuclear antigen of the Epstein-Barr virus (Epstein-Barr Virus Nuclear Antigen IgG, EBNA-IgG) and IgG antibodies to the capsid antigen of the Epstein-Barr virus (anti-Epstein — Barr viral capsid antigens IgG, EBV VCA IgG); IgG to Toxoplasma gondii
(70 IU/ml);
IgG to cytomegalovirus (CMV); IgG to herpes virus types 1 and 2 were positive (1:1600). According to the results of urine PCR, no urogenital infections were detected. Studies performed in the infectious diseases department of the hospital were also taken into account. During the examination, no data were obtained for an acute infectious process. At the same time, the detected high titer (1:1600) of IgG to the herpes simplex virus, positive IgG to Toxoplasma gondii
(70 IU/ml) and positive IgG to CMV could be interpreted as a possible trigger for the autoinflammatory process. A PCR blood test taken at this time showed the presence of CMV DNA of 40 copies/105 cells, which was interpreted by infectious disease specialists as a reactivation of a chronic infection during treatment and was clinically insignificant. However, it was impossible not to pay attention to the role of virus carriage, in particular herpes simplex viruses, cytomegalovirus and Epstein-Barr virus, in the activation of the autoinflammatory process. The levels of tumor markers (AFP, hCG, PSA) were within the reference values. A study of the myelogram and cellular bone marrow punctate revealed normoblastic erythropoiesis, the myeloid lineage was expanded to 81.4%, toxic granularity was noted, megakaryocytes in sufficient numbers of varying degrees of maturity with increased platelet formation. As noted earlier, this myelogram pattern is characteristic of EFS. A cytogenetic study analyzed 20 bone marrow metaphases. A karyotype of 46,XY was identified (20). No visible structural disturbances were recorded with 400-band G-banding. Also, the V617F mutation in exon 14 of the JAK2-kinase gene and the expression of the chimeric human oncogene BCR-ABL were not detected, which made it possible to exclude oncohematological diseases. The HLA-B27 antigen was not detected in the lymphocyte phenotype; antinuclear antibodies (Antinuclear antibody, ANA) and antineutrophil cytoplasmic antibodies (Antineutrophil cytoplasmic antibodies, ANCA) were negative; antibodies to the cytoplasm of neutrophils with determination of the type of luminescence (cANCA, pANCA) were also negative. AT to native double-stranded DNA (dsDNA) were within the reference values; Anti-extractable nuclear antigen (ENA/ENA-screen) nRNP/Sm, Sm, SS-A, SS-B, Scl-70, Jo-1 - within reference values; RF was normal. The immunogram revealed an imbalance of the main subpopulations of T-lymphocytes - an increase in the relative number of cytotoxic T-lymphocytes and total T-cells. Analysis of small subpopulations of T cells indicated an increase in the percentage of T cells expressing natural killer markers CD16 and CD56, a decrease in the relative and absolute number of NK cells expressing CD16 and CD56 antigens, and NK cells expressing the α-chain of the CD8 antigen and possessing the ability to repeatedly perform its cytolytic function. Along with this, there was a decrease in the relative and absolute number of total B-lymphocytes. Noteworthy was the increase in the concentration of immunoglobulin G and the level of circulating immunoglobulins (67 units). Based on the results of the studies, no data were obtained for an autoimmune disease.
The patient underwent ultrasound examination of the abdominal organs, kidneys, pelvic organs, scrotum, and thyroid gland; CT scan of the chest and abdominal organs, FGDS. Based on the results of these instrumental studies, no data on the oncological process were obtained. An MRI of the head did not reveal the presence of space-occupying formations, foci in the brain substance, or pathology of the chiasmal-sellar region. Fever of endocrine and central origin was excluded. There was an impression of an autoinflammatory process that could cause febrile fever. In addition, the assumption of rare autoinflammatory diseases associated with genetic defects in the mechanisms of thermoregulation was considered: a defect in the TNF receptor gene (familial periodic fever syndrome, TNF-receptor-associated periodic syndrome, TRAPS syndrome); familial Mediterranean fever (FMF) and mevalonate kinase deficiency (MKD). However, the rather late onset of the disease, the absence of family segregation and typical periodicity of fever, as well as patient assessment using the Eurofever Project classification criteria calculator developed by the Pediatric Rheumatology European Society (PRES), made it possible to exclude these nosological forms with a high degree of confidence [ 7]. Unfortunately, genetic testing of such patients, necessary for more reliable verification of the diagnosis, still remains difficult to access and expensive [8, 9].
After performing a series of studies that allowed us to exclude a number of diseases, and based on the classification criteria of M. Yamaguchi (1992) (with five criteria, two of which are large: fever more than 39 ° C for at least 1 week and leukocytosis more than 10, 0×106/l with neutrophilia more than 80%), three minor: sore throat, lymphadenopathy and splenomegaly, increased ALT and AST levels) was diagnosed with: A special form of rheumatoid arthritis, active Still's disease in adults, systemic clinical form (monocyclic variant) , system score - 6 points (fever, hepatomegaly, splenomegaly, lymphadenopathy, leukocytosis, myalgia), FC I. Complications: Secondary nephropathy of toxic origin (NSAID nephropathy). Mild normochromic normocytic anemia. Concomitant diseases: Chronic gastritis, unstable remission .
After the final diagnosis was made, pulse therapy with methylprednisolone 500–1000–1000 mg/day was carried out for 3 days with a transition to oral prednisolone at a dose of 50 mg/day. Immunosuppressive therapy with methotrexate 20 mg/week was prescribed. Against the background of satisfactorily tolerated pulse therapy with GCS, hepato- and gastroprotective therapy, the patient noted a significant improvement in health, the fever was stopped. Taking into account the presence of chronic viral infection (herpes and cytomegalovirus infection), valacyclovir 1000 mg/day was added to therapy. As a result of the therapy, pronounced positive dynamics were observed in the form of relief of clinical manifestations (arthralgia and myalgia, chills, weakness, sore throat), normalization of laboratory parameters (absence of signs of inflammatory, urinary, cytolytic syndromes). The patient was presented to a military medical commission, by which he was declared unfit for military service and dismissed from the Armed Forces.