Obliterating atherosclerosis is one of the main diseases that causes impaired blood supply to the lower extremities. The disease is associated with the accumulation of cholesterol in the artery wall, forming plaques that block the lumen of the artery. The arteries become hard and their patency is impaired. This pathology can lead to thrombosis of the affected artery with the development of acute ischemia. The disease usually develops in old age, often against the background of diabetes mellitus, although now relatively young patients also turn to a vascular surgeon.
Lack of blood supply leads to dysfunction of the muscles of the limb, this is manifested by fatigue when walking for some distance, and with severe decompensation of blood circulation, gangrene of the leg can develop.
Symptoms of atherosclerosis of leg vessels
The development of the disease occurs gradually and in the first stages there may be nothing to show for it. Subsequently, the patient develops pain in the lower extremities, especially with prolonged walking, and a feeling of numbness in the feet. A decrease in temperature is felt on the legs, pallor and cyanosis are visible, and cramps occur. Over time, a person develops intermittent claudication and trophic changes occur in the form of delamination of nails and the formation of ulcers on the fingers and heels.
- with atherosclerosis, the patient may feel and observe the following:
- muscle pain in the legs, in the later stages even the feet hurt, and the pain cannot be relieved with painkillers;
- limited mobility of the affected leg;
- pain along the affected artery - first during physical activity, then at rest;
- intermittent claudication - after walking some distance, a person is forced to stand up and give his legs a rest, and then he moves on until the next attack of weakness;
- tingling, numbness in the affected area;
- thickening of nails;
- loss or slow growth of hair on the legs;
- paleness when raising the legs and sharp redness when lowering them;
- rapid freezing of feet;
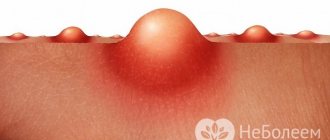
- sores on the skin;
- purple fingers;
- absence of pulsation in the affected artery;
- areas of darkening on the skin are signs of the onset of gangrene in advanced stages;
- coldness of the skin of the leg;
- reduction in the mass and volume of the muscles of the thighs and legs.
At the beginning of the disease, as a rule, one limb suffers, then the process becomes symmetrical - this is a signal that the arteries are affected on both sides. An objective examination reveals the absence of pulsation in the popliteal fossa, thigh and ankle.
Complications
The most common complications of the disease is occlusion (blockage, thrombosis) of the vessels of the legs. This condition is fraught with even more dangerous consequences: gangrene, pulmonary embolism. In the first case, the patient faces amputation of the affected leg. In the case of pulmonary embolism, there is a possibility of sudden death due to pulmonary edema. Therefore, it is important to recognize the signs of complete blockage in time:
- intense pain in the leg against the background of its atypical pallor (the leg seems to be made of wax);
- lack of pulse in the leg;
- paralysis, inability to control the lower limb or rely on it;
- loss of sensation in the leg in the area below the location of the blood clot.
If such symptoms appear, it is necessary to urgently take the patient to the nearest clinic, ensuring the lower limb is rested. Occlusion can be eliminated by two methods: conservative (by intravenous administration of antiplatelet agents, fibrinolytics and thrombolytics), or surgical (endarterectomy, thrombectomy and other methods).
If gangrene develops as a result of acute occlusion or sluggish stenotic atherosclerosis, the doctor in most cases decides to amputate the affected limb in order to prevent sepsis (the so-called blood poisoning with necrotic poisons). n Almost all of the complications listed are the consequences of untreated atherosclerosis of the lower extremities or ignoring the recommendations of the attending physician. To prevent their occurrence, it is enough to follow a diet and take medications prescribed by a specialist, as well as undergo periodic examinations that will help identify processes predisposing to complications and eliminate them in a timely manner.
Risk factors
The development of OA is based on the following most significant risk factors, the degree of influence of which can be different Sources: 1. Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. 2. Podrezenko E.S. The influence of risk factors on the development of obliterating atherosclerosis of the vessels of the lower extremities / E.S. Podrezenko, S.S. Dunaevskaya // Health is the basis of human potential: problems and ways to solve them. - 2012. - pp. 576-578. 3. Fattakhov V.V. Obliterating atherosclerosis of the lower extremities in the practice of a polyclinic surgeon / V.V. Fattakhov // Practical medicine. - 2010. - No. 2 (41). — P. 126-130. :
- male gender (men get sick 10 times more often);
- age (over 40 years);
- poor nutrition;
- overweight (obesity);
- smoking tobacco;
- hypokinesia (insufficient motor activity);
- hypofunction of the thyroid and gonads;
- heredity;
- some concomitant diseases (diabetes mellitus, coronary heart disease, heart rhythm disorders, lipid and carbohydrate metabolism, hypertension);
- exposure to adverse environmental factors.
Causes and mechanism of development
3 main etiological factors of atherosclerosis of leg vessels have been identified:
- high blood cholesterol levels (increased total cholesterol, lipoproteins), which has been observed for many years;
- genetic predisposition – the disease runs in the family;
- impaired metabolism, mainly fats.
Predisposing factors
Prerequisites for the occurrence of the disease include:
- smoking - causes spasm of the arteries, which impairs blood flow;
- addiction to alcohol - disrupts metabolism, in particular fats, in the liver;
- excessive consumption of animal fats;
- obesity;
- hormonal disorders: diabetes mellitus (provokes the occurrence of atherosclerosis of the vessels of the legs even in adolescence), imbalance of sex hormones, hypothyroidism;
- arterial hypertension;
- regular stress (promotes the release of adrenaline, which spasms the arteries);
- age (the risk of developing the disease increases after 40);
- belonging to the Negroid race;
- regular hypothermia of the legs;
- arteritis of the lower extremities;
- physical inactivity.
Stages of development of atherosclerosis of the lower extremities
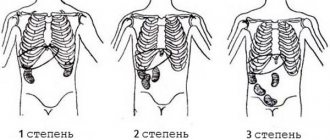
The most detailed is the modified classification of chronic arterial insufficiency of the lower extremities (CANF), which takes into account in detail the phenomena of critical limb ischemia, which is necessary when determining treatment tactics.
| Stage 1 | Muscle pain only during heavy physical activity (when walking over a distance of more than 1 km). Initial signs of stenosis appear - the skin turns pale, there is a feeling of goosebumps, it seems that the legs are always cold, fatigue quickly sets in when walking, excessive sweating is observed |
| Stage 2A | Feeling of fatigue and stiffness in the calf muscles, intermittent claudication after 200-1000 m |
| Stage 2B | Intermittent claudication in less than 200 m |
| Stage 3A | Intermittent claudication after a few steps or pain at rest when it is possible to keep the lower limb in a horizontal position for more than 2 hours |
| Stage 3B | Pain at rest, ischemic edema, inability to keep the lower limb in a horizontal position for 2 hours |
| Stage 4A | Gangrene of the fingers or part of the foot with the prospect of maintaining the supporting function of the limb |
| Stage 4B | Extensive necrotic changes in the limb without the possibility of maintaining its supporting function |
Patient recovery after radical intervention
According to Russian legislation, the person undergoing surgery can remain in a hospital bed for no more than 14 days. He then spends the rehabilitation period at home. A very important point is the mandatory use of medications on an ongoing basis, physical therapy, taking a massage course, using natural mud, clay, essential oils, and undergoing physiotherapy. If an elderly person is surrounded by family, then recovery takes place very quickly, since all necessary procedures are strictly monitored by relatives.
It is more difficult with lonely old people. In this case, it is necessary to send him for rehabilitation to an institution that provides this service. For example, in the “Zabota” boarding house for the elderly, all conditions have been created for restoring health after operations. It is very important for the patient to accept himself, calm down, maintain faith in people and adapt to a new life. Therefore, psychologists and psychiatrists work with such guests, and they are cared for around the clock. The wards are equipped with beds with the necessary equipment. In addition, they will not be allowed to be alone. Communication with peers, walks in the fresh air, holiday concerts, hobby classes, and daily recreational activities will bring them back to life.
What should be the intensity and duration of dosed walking?
After surgery, it is very important for a quick recovery to exercise two to three times a week on a special exercise machine - a treadmill.
Initially, you need to set the minimum speed. As lameness decreases when walking, it gradually increases. The first time is 30 minutes. Next, the duration of the workout gradually increases to one hour.
Very important! Classes should take place in a boarding house or sanatorium under the supervision of a doctor who assesses your well-being by pulse, shortness of breath and, God forbid, chest pain.
Diagnostics
There is a standard diagnostic program for this disease:
- Ultrasound of vessels of the lower extremities (duplex and Doppler scanning);
- coagulogram (determination of the blood coagulation system);
- determination of cholesterol and LDL levels in the blood;
- leg arteriography;
- establishment of pulsation in peripheral arteries;
- MR, MSCT angiography.
If prescribed by a doctor, MRI and CT scans with contrast and rheovasography can be performed.
To make a timely diagnosis of atherosclerosis of the vessels of the lower extremities, consultation with a vascular surgeon or phlebologist and a number of diagnostic measures are necessary.
Due to the systemic nature of the atherosclerotic process, patients with OA of the lower extremities often experience combined damage to various arterial basins, therefore, in such patients, an integral part of instrumental diagnosis is the study of extracranial and coronary arteries. Identification of pathology in them may require a change in treatment tactics or the order of surgical interventions Source: Kuznetsov M.R. Basic principles of diagnosis and treatment of obliterating atherosclerosis of the arteries of the lower extremities / M.R. Kuznetsov // General medicine. - 2008. - No. 1. - P. 3-8. .
Treatment of atherosclerosis of the vessels of the lower extremities
The approach to treatment is determined depending on the stage of the disease and is primarily about choosing the right regimen. It is necessary to adhere to a diet limiting fried and fatty foods, eliminating smoking and alcohol, as well as combating excess weight. The patient should follow a walking and physical activity regimen, choose comfortable and spacious shoes, and treat even the smallest injuries on the skin of the lower extremities. Treatment of concomitant chronic diseases is mandatory.
Medicinal methods include anticoagulants, antiplatelet drugs, agents that improve blood microcirculation, vasodilators, and physiotherapeutic procedures.
In severe cases, surgical treatment may be necessary.
General recommendations:
- normalize weight;
- follow a diet with low cholesterol;
- give up alcohol and smoking;
- wear shoes that fit;
- do not overcool your feet;
- even minor injuries should be carefully treated and treated;
- trim nails carefully without damaging soft tissues;
- engage in moderate physical activity - walking, swimming, cycling or exercising on an exercise bike.
Treating atherosclerosis
- Shishkin A.A.
- Volkov A.M.
- Kabirov A.V.
- Baranov V.S.
Shishkin Andrey Andreevich
Candidate of Medical Sciences. Surgeon, proctologist, phlebologist at SM-Clinic. Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
Read moreVolkov Anton Maksimovich
Phlebologist, surgeon at SM-Clinic. Performs operations with a modern proprietary method of treating varicose veins using a laser (modified endovenous laser coagulation. M-EVLC).
Surgical treatment of varicose veins of any complexity (phlebectomy, miniphlebectomy) More detailsKabirov Alexander Vitalievich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
More detailsBaranov Vladimir Sergeevich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Treats lower varicose veins using non-surgical and surgical methods (aesthetic sclerotherapy, ECHO sclerotherapy, stem sclerotherapy, phlebectomy, miniphlebectomy, EVLT).
More details
Conservative treatment
The patient may be prescribed various medications:
- prevent the formation of blood clots, prevent stroke and heart attack;
- increasing physical activity, improving blood flow in the lower extremities;
- antiplatelet drugs that lower blood cholesterol levels;
- anticoagulants, which prevent blood clotting in blood vessels and prevent blood clots;
- antispasmodics to relieve pain and spasms;
- antimicrobial ointments that need to be used to treat trophic ulcers;
- medications that promote better tissue nutrition;
- vasodilators;
- vitamins.
Also, as part of conservative therapy, physiotherapy is performed - electrophoresis with novocaine, darsonvalization, hyperbaric oxygenation.
Drug therapy
The most important thing is to restore normal blood flow. For this purpose, as a rule, drugs are prescribed that relieve vascular spasms and prevent narrowing, expand the lumen, block thrombus formation, and increase blood flow.
Please note: in order to achieve the most effective result safely for your health, our specialists will select all medications strictly individually, taking into account all the necessary factors - from the severity of the disease to your general condition at the time of treatment.
Surgical techniques
Surgery is a last resort and is usually prescribed for severe ischemia and very severe complications. Nowadays, different types of surgical interventions are performed. Some involve a day hospital, some require a long-term hospital stay under observation. Patient rehabilitation plans and post-operative care vary. Our doctors advise patients in detail on all aspects related to surgical intervention and carefully monitor their health in the pre- and postoperative period.
Surgical treatment of atherosclerosis of the lower extremities:
- bypass surgery - an additional “bypass” path for blood flow is created around the area of narrowing of the artery;
- stenting - a special tubular spacer is placed in the affected vessel, which ensures the required diameter of the artery;
- balloon angioplasty - similar to stenting, only a balloon is inserted into the vessel cavity rather than a spacer, which expands its lumen;
- autodermoplasty - if trophic ulcers are poorly treated conservatively, they are operated on and covered with the patient’s own skin;
- endarterectomy - removal of the affected part of the artery in which the atherosclerotic plaque is located;
- prosthetics – replacement of the affected vessel with the patient’s own vein, taken from another place, or with a synthetic prosthesis;
- amputation - prescribed in severe cases when gangrene occurs, after which prosthetics are performed.
In 75-85% of cases, after surgery, blood circulation is completely restored for an average of 5-8 years.
Indications for surgery:
- an aneurysm that may rupture;
- chronic ischemia of critical stage;
- hemodynamically significant carotid artery stenosis or plaque accompanied by symptoms of cerebral ischemia;
- decompensation of blood circulation in the leg due to embolism, trauma, thrombosis.
Contraindications to surgical treatment:
- wet gangrene with sepsis;
- severe disruption of vital organs - renal and liver failure, circulatory disorders in the brain, myocardial infarction, heart failure, etc.
Possible risks associated with the disease
The disease is insidious in that it is impossible to predict its course and symptoms. Approximately 20% of patients over 65 years of age, having severe plaques, do not feel any discomfort. The seriousness of the progressive course of OA ANC is also due to the fact that after the appearance of the first symptoms, 10-40% of patients develop gangrene within 3-5 years, which leads to amputation of a limb or death Source: Kazantsev A.V. A new approach to surgical tactics for obliterating atherosclerosis of the arteries of the lower extremities / A.V. Kazantsev, E.A. Korymasov // Saratov Medical Scientific Journal. - 2010. - T. 6. - No. 4. - P. 850-856. .
Atherosclerosis can be complicated by arterial thrombosis. This complication, if not immediately sought by a doctor, leads to loss of a limb or embolism of other arteries. If the clot detaches and enters the coronary artery, a myocardial infarction may develop, and if it migrates to the carotid artery, a stroke may occur.
Some information about the disease
Atherosclerosis of the leg arteries is a dangerous vascular disease that is considered most common in patients over 50–60 years of age. The first symptoms of pathology appear already at the stage of insufficient supply of oxygen and nutrients to the tissues, but the development of atherosclerosis from the first to the last stage takes about ten years.
In order for all internal organs and tissues to function fully, they need a high-quality supply of blood. All tissues are stuffed with capillaries, and if they are clean, then the organs receive the required amount of oxygen and necessary substances. When the lumen of the vessel is contaminated and blocked by cholesterol deposits, signs of an inflammatory process appear.
With the systematic deposition of a substance on the walls of the arteries, plaques are formed, which over time become stone due to the deposition of calcium salts. A blood clot can break away from the plaque, which will slow down blood flow or completely block an important artery. And this is already fraught with dangerous consequences, even death.
Prevention methods
For prevention purposes, you need to start controlling the levels of lipids, sugar and cholesterol in the blood as early as possible. Even with a slight increase in numbers relative to the norm, you should consult a doctor. It is also recommended to regularly do ultrasound of the lower extremities - once every 1-2 years.
It is important to watch your diet, because the reason for the increase in “bad” cholesterol in the blood is the saturated fats that we consume in food. These are products of animal origin - fatty meat, lard, butter. There is a lot of cholesterol in eggs, or rather in the yolks. All these products should be consumed in the smallest possible quantities.
Use of traditional medicine
Atheroskerosis cannot be cured using traditional medicine alone. However, they show effectiveness in the prevention of thrombosis, atherosclerosis and hypertension when prescribed in addition to drug therapy. Folk remedies have few contraindications, but are not combined with all medications. Therefore, their use should only be in consultation with a doctor.
The most popular recipes for the treatment of OA:
- Grind with a blender or mince 5 lemons and the same number of heads of garlic, mix with kg of honey. Take once a day, tbsp. Course - 1 month;
- Pass 50 g of garlic through a press, pour in 0.2 liters of vodka. Leave for 7-9 days. Take 7-10 drops three times a day, diluted in a spoonful of milk or water;
- Pour 200 g of hawthorn berries into 0.2 liters of alcohol. Leave for 3 weeks. Filter and take tsp. 30 minutes before breakfast;
- 25 g of bindweed leaves and flowers are poured into 0.1 liters of alcohol. Wait a week. Strain and take 1/2 tsp twice a day for two weeks;
- Horse chestnut juice relieves swelling and strengthens artery walls. Drink it twice a day, 25 drops per glass of water;
- Drink 100 ml of cucumber juice before breakfast. Course - 3 weeks;
- Tbsp. crushed dill seeds pour a glass of hot water. Leave for about 20 minutes, and divide the entire volume into 4 doses.
- A medicinal mixture of red clover, sweet clover and burdock root is boiled over low heat for about 2 minutes, after which the bowl is wrapped in a warm towel. Leave the infusion for 20-30 minutes, then filter. Drink 1/3 glass three times a day. The course is designed for a month, after which a break of 2 months is taken.