Surgeon
Bohyan
Tigran Surenovich
Experience 36 years
Surgeon of the highest category, Doctor of Medical Sciences, member of the International Association of Surgeons, Gastroenterologists and Oncologists
Make an appointment
An abscess is an accumulation of purulent contents in various tissues. Purulent inflammation is usually caused by a bacterial infection. In this case, in the process of melting the tissue, a cavity is formed. The occurrence of an abscess is caused by bacteria entering the tissue from the outside - through abrasions and injuries or from other infected tissues and organs. This disease differs from other similar diseases in the formation of a capsule that prevents the spread of inflammation.
Based on the location of the pus, there are superficial accumulations in the subcutaneous fatty area and deep ones inside organs and deep tissues. Depending on the method of penetration of pathogenic microorganisms, there are exogenous accumulations (from the external environment) and endogenous (migration within the body of one person).
Causes of abscess and risk factors
The cause of the abscess is pyogenic microflora, which enters the patient’s body through damage to the mucous membranes or skin, or is carried through the bloodstream from another primary source of inflammation (hematogenous route).
The causative agent in most cases is a mixed microbial flora, in which staphylococci and streptococci predominate in combination with various types of bacilli, for example, E. coli. In recent years, the role of anaerobes (clostridia and bacteroides), as well as associations of anaerobic and aerobic microorganisms in the development of abscesses, has increased significantly.
Sometimes there are situations when the pus obtained during opening of an abscess, when inoculated on traditional nutrient media, does not give rise to the growth of microflora. This indicates that in these cases the disease is caused by uncharacteristic pathogens, which cannot be detected by conventional diagnostic techniques. To a certain extent, this explains cases of abscesses with an atypical course.
The main cause of an abscess is the penetration of pyogenic microflora through the skin and mucous membranes
Abscesses can occur as an independent disease, but more often they are a complication of some other pathology. For example, pneumonia can be complicated by a lung abscess, and purulent tonsillitis can be complicated by a peritonsillar abscess.
With the development of purulent inflammation, the body's defense system seeks to localize it, which leads to the formation of a limiting capsule.
Forms of the disease
Depending on location:
- subphrenic abscess;
- retropharyngeal;
- paratonsillar;
- peripharyngeal;
- soft tissues;
- lung;
- brain;
- prostate gland;
- periodontal;
- intestines;
- pancreas;
- scrotum;
- Douglas space;
- appendicular;
- liver and subhepatic; and etc.
Subcutaneous tissue abscesses usually result in complete recovery.
According to the characteristics of the clinical course, the following forms of abscess are distinguished:
- Hot or spicy. Accompanied by a pronounced local inflammatory reaction, as well as a violation of the general condition.
- Cold. It differs from a regular abscess in the absence of general and local signs of the inflammatory process (fever, redness of the skin, pain). This form of the disease is characteristic of certain stages of actinomycosis and osteoarticular tuberculosis.
- Natechny. The formation of an area of pus accumulation does not lead to the development of an acute inflammatory reaction. Abscess formation occurs over a long period of time (up to several months). Develops against the background of the osteoarticular form of tuberculosis.
Complications
In the absence of timely and adequate treatment, complications of abscesses are very dangerous for the life and health of the patient:
- phlegmon;
- neuritis;
- osteomelitis;
- internal bleeding of the walls of blood vessels;
- peritonitis,
- sepsis as a result of purulent abscess of the appendicular region;
- purulent meningitis and others.
Contacting the clinic
A purulent accumulation is fraught with dangerous consequences, therefore, if the slightest sign of the presence of an accumulation of pus in tissues or organs appears, you should immediately consult a doctor. The ideal solution would be to call an ambulance.
At (academician Roitberg’s clinic) you will receive the necessary assistance in treatment. In addition, JSC “Medicine” (academician Roitberg’s clinic) has the ability to accommodate patients in a 24-hour hospital and has the function of calling a doctor at home around the clock.
Abscess symptoms
The clinical picture of the disease is determined by many factors and, above all, the location of the purulent process, the cause of the abscess, its size, and the stage of formation.
Symptoms of an abscess localized in the superficial soft tissues are:
- swelling;
- redness;
- severe pain;
- increase in local, and in some cases general temperature;
- dysfunction;
- fluctuation.
Abdominal abscesses are manifested by the following symptoms:
- intermittent (intermittent) fever with a hectic type of temperature curve, i.e., subject to significant fluctuations during the day;
- severe chills;
- tachycardia;
- headache, muscle and joint pain;
- lack of appetite;
- severe weakness;
- nausea and vomiting;
- delayed passage of gas and stool;
- tension in the abdominal muscles.
When the abscess is localized in the subphrenic region, patients may experience shortness of breath, cough, pain in the upper abdomen, which intensifies during inspiration and radiates to the scapula and shoulder.
With pelvic abscesses, reflex irritation of the rectum and bladder occurs, which is accompanied by the appearance of tenesmus (false urge to defecate), diarrhea, and frequent urination.
Retroperitoneal abscesses are accompanied by pain in the lower back, the intensity of which increases when the legs are bent at the hip joints.
Symptoms of a brain abscess are similar to the symptoms of any other space-occupying formation (cysts, tumors, hematomas) and can vary very widely, ranging from a minor headache to severe cerebral symptoms.
A lung abscess is characterized by a significant increase in body temperature, accompanied by severe chills. Patients complain of pain in the chest, worsening when trying to take a deep breath, shortness of breath and a dry cough. After opening the abscess into the bronchus, a strong cough occurs with copious discharge of sputum, after which the patient’s condition begins to quickly improve.
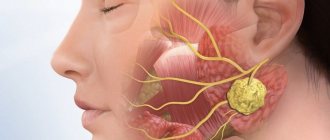
Abscesses in the oropharynx (retropharyngeal, paratonsillar, peripharyngeal) in most cases develop as a complication of purulent tonsillitis. They are characterized by the following symptoms:
- severe pain radiating to the teeth or ear;
- sensation of a foreign body in the throat;
- muscle spasm that prevents mouth opening;
- soreness and swelling of regional lymph nodes;
- increased body temperature;
- insomnia;
- weakness;
- nasal voice;
- the appearance of an unpleasant putrid odor from the mouth.
Diagnosis of an abscess
Superficially located soft tissue abscesses do not cause diagnostic difficulties. With a deeper location, it may be necessary to perform an ultrasound and/or diagnostic puncture. The material obtained during puncture is sent for bacteriological examination, which allows identifying the causative agent of the disease and determining its sensitivity to antibiotics.
Oropharyngeal abscesses are identified during an otolaryngological examination.
Abscesses can occur as an independent disease, but more often they are a complication of some other pathology. For example, pneumonia can be complicated by a lung abscess, and purulent tonsillitis can be complicated by a peritonsillar abscess.
Diagnosis of abscesses of the brain, abdominal cavity, and lungs is much more difficult. In this case, an instrumental examination is carried out, which may include:
- Ultrasound of the abdominal and pelvic organs;
- magnetic resonance or computed tomography;
- radiography.
If the abscess is deep, an ultrasound and diagnostic puncture are performed.
In a general blood test, at any location of the abscess, signs characteristic of an acute inflammatory process are determined (increased number of leukocytes, shift of the leukocyte formula to the left, increase in ESR).
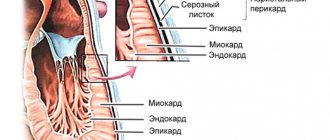
Pathological anatomy
An abscess always occurs either in already dead tissues, in which microbial-chemical processes of autolysis increase (for example, during injury), or in living tissues that are exposed to strong microbial influence (for example, during infections). According to the nature of the course, an abscess can be acute or chronic.
In the initial period of formation of an abscess, a limited area of tissue is infiltrated with inflammatory exudate and leukocytes. Gradually, under the influence of leukocyte enzymes, the tissue undergoes melting, and a cavity is formed filled with purulent exudate. The shape of the cavity can be either simple round or complex, with numerous pockets.
Rice. 1. Acute abscess. An area of tissue infiltrated with purulent exudate. Accumulation of leukocytes along the periphery of the abscess (1). Rice. 2. Chronic lung abscess. The wall of the cavity is formed by a pyogenic membrane, consisting of two layers: 1 - inner layer (granulations and scraps of necrotic tissue); 2 - outer layer (mature connective tissue).
The walls of the Abscess in the early stage of its formation are covered with purulent-fibrinous deposits and fragments of necrotic tissue. Subsequently, a zone of demarcation inflammation develops along the periphery of the Abscess; its constituent infiltrate serves as the basis for the formation of a pyogenic membrane that forms the wall of the cavity (Fig. 1). The pyogenic membrane is a vascular-rich layer of granulation tissue. Gradually, in that part of it that faces the tissues surrounding the Abscess, granulations mature. Thus, if the Abscess becomes chronic, two layers are formed in the pyogenic membrane: the inner one, facing the cavity and consisting of granulations, and the outer one, formed by mature connective tissue (Fig. 2).
Abscesses in various organs have certain features that reflect the unique structure and function of these organs. So, with a liver abscess, its contents contain an admixture of bile; areas of epithelization of the pyogenic membrane appear.
ABSCESS, as a rule, ends with spontaneous emptying and release of pus to the surface of the body, into hollow organs or into body cavities. A breakthrough of the Abscess onto the surface of the body or into a hollow organ, provided that the purulent cavity is well drained and there is no scar capsule, often leads to the elimination of the Abscess cavity through scarring. Relatively rarely, an abscess undergoes encapsulation. In this case, the pus thickens, cholesterol crystals fall out, and a thick scar capsule containing xanthoma cells forms around the abscess. Sometimes ABSCESSES that arise around animal parasites undergo petrification.
If the communication of the Abscess with the surface of the body is insufficient or there are other reasons that prevent the collapse of the walls of the Abscess cavity, then after its emptying a fistula (see) is formed - a narrow canal lined with granulation tissue or epithelium, which connects the A. cavity with the surface of the body or with the lumen of the hollow organ. A fistula often occurs in cases where the Abscess cavity contains foreign bodies or sequesters.
In some diseases, due to the characteristics of the pus, it can actively melt the surrounding tissues, spread through intertissue cracks and accumulate in places remote from the primary localization of the ABSCESS, for example, the so-called cold abscesses (leaks), characteristic of tuberculosis, which can also be emptied through the fistulous tracts.
Abscess treatment
In the initial stage of development of abscess of superficial soft tissues, anti-inflammatory therapy is prescribed. After the abscess has matured, it is opened, usually on an outpatient basis. Hospitalization is indicated only in severe general condition of the patient and the anaerobic nature of the infectious process.
It is recommended to use Elon ointment as an aid in treatment, as well as to prevent complications of abscesses of subcutaneous fat. The ointment should be applied to the affected area under a sterile gauze bandage or patch. Depending on the degree of suppuration, the bandage must be changed once or twice a day. The duration of treatment depends on the severity of the inflammatory process, but, on average, to obtain a satisfactory result, you need to use the ointment for at least five days. Elon K ointment is sold in pharmacies.
Ointment Elon K
Treatment of a lung abscess begins with the prescription of broad-spectrum antibiotics. After receiving an antibiogram, antibiotic therapy is adjusted taking into account the sensitivity of the pathogen. If there are indications, bronchoalveolar lavage is performed to improve the outflow of purulent contents. The ineffectiveness of conservative treatment of an abscess is an indication for surgical intervention - resection (removal) of the affected area of the lung.
Abdominal abscesses are removed surgically
Treatment of brain abscesses in most cases is surgical, as they can lead to brain dislocation and cause death. A contraindication to the removal of abscesses is their localization in deep and vital structures (subcortical nuclei, brain stem, thalamus). In this case, they resort to puncture of the abscess cavity, removal of purulent contents by aspiration, followed by washing the cavity with an antiseptic solution. If repeated rinsing is required, the catheter through which it is carried out is left in the cavity for some time.
With brain abscesses, the prognosis is always very serious, death is observed in 10% of cases, and 50% of patients develop permanent disability.
Abdominal abscesses are removed surgically.
Local remedies
Local medications can be used to treat abscesses. For example, if an abscess has formed in a child, Bepanten ointment will be an effective treatment, which quickly copes with the inflammatory process and accelerates wound healing.
For an adult, ointments such as Levomekol, Vishnevsky, Ichthyol are perfect. The first (Levomekol) has a powerful anti-inflammatory effect, as well as an antiseptic. The advantage of the medicine is the elimination of both the symptoms of the abscess and its cause. The ointment has few side effects.
Vishnevsky ointment is used in the treatment of abscesses, as well as carbuncles and boils, trophic and varicose ulcers. The only contraindication is hypersensitivity to the components of the drug. There are no other contraindications, as well as side effects from use.
Triderm ointment is an excellent remedy in the fight against fungal pathologies.
In case of a fungal infection, the use of ointments with an antifungal effect is prescribed. This could be Triderm, Mycozolon, etc.
Prevention
Prevention of the development of abscesses is aimed at preventing the entry of pathogenic pyogenic microflora into the patient’s body and includes the following measures:
- careful adherence to asepsis and antisepsis when carrying out medical interventions accompanied by damage to the skin;
- timely primary surgical treatment of wounds;
- active sanitation of foci of chronic infection;
- increasing the body's defenses.
Video from YouTube on the topic of the article: