© Author: Z. Nelly Vladimirovna, laboratory diagnostics doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
Bilirubin in the biochemical blood test (BAC) claims to have a central place, since it is prescribed in almost all cases requiring laboratory diagnostics: clinical examination, examination of workers engaged in hazardous work, pregnancy and various diseases associated with the hemostatic system, liver and gallbladder function , as well as persons with a family history. In a word, this analysis can be called almost universal, because it is prescribed much more often than others. However, many people are not satisfied with just the word (bilirubin) and its norm; they want to know what this substance is and how it is formed, how to reduce it if the values have crossed acceptable limits. This is what we will talk about today.
What is bilirubin, meaning
The content of the article
The bilirubin molecule consists of 4 pyrrole rings connected to each other. The molecular weight of the molecule is 548.68. Pure bilirubin is a sparingly soluble crystalline substance.
Being a breakdown product of red blood cells, bilirubin is toxic. Its indirect form is constantly formed in tissues and blood and is not excreted from the body. The liver processes the toxic substance and converts it into a direct form that is soluble in water. The direct form is excreted in feces or urine, turning them brown.
Of great importance in diagnosis is the study of the relationship between bilirubin levels in the blood, urine and feces. Even if a blood test shows total bilirubin is normal, but the absolute values and the ratio of pigment fractions have deviations, a differential diagnosis of the disease should be made.
The sum of the fractions can give an overall normal value of total bilirubin, but it often happens that primary bilirubin is elevated and conjugated bilirubin is below normal. This fractional ratio is observed in the initial forms of liver enzyme deficiency and the threat of excessive accumulation of toxic indirect bilirubin in the tissues.
Signs of elevated bilirubin
As is known, the primary role in the metabolism of bilirubin belongs to the liver, and jaundice is a characteristic syndrome that reflects its damage and also manifests itself in cases where the amount of bilirubin exceeds the functional ability of the liver to bind its excess, or there are obstacles to the outflow of bile and, accordingly, the excretion of conjugated bilirubin from the body.
Sometimes it happens that the severity of jaundice does not correspond to the levels of bilirubin in the serum. For example, with obesity and edema, jaundice is less noticeable, while in thin and muscular people it is more pronounced.
The reasons for high bilirubin in the blood are very diverse and are associated either with its increased formation in the cells of the reticuloendothelial system, or with a disturbance in one or several metabolic links in the hepatobiliary system.
From a clinical point of view, it is important to note that the degree of hyperbilirubinemia affects the staining pattern of various tissues:
- So, most often the sclera is the first to acquire a jaundiced tint.
- Oral mucosa
- Then the face, palms, soles and finally the entire skin turn yellow
It must be remembered that yellow discoloration of the skin is not always a consequence of hyperbilirubinemia. For example, when eating food containing a large amount of carotene (carrots, tomatoes), diabetes mellitus, hypothyroidism (decreased thyroid function), the skin may acquire a yellow tint, but in these cases the sclera will be of normal color (intact).
Bilirubin norms by age
| Type of bilirubin | Children: first 3 days after birth, µmol/l | Children: from 3 to 6 days of life, µmol/l | Children: over 1 month, µmol/l | Adults, µmol/l |
| General | 24 — 190 | 28 — 210 | 3,5 — 20,4 | 8 — 20,5 |
| Straight | 0,5 — 10,2 | 1 — 12,4 | 0 — 5,1 | 0 — 5,1 |
| Indirect | 23,5 — 179,8 | 27 — 197,6 | Up to 16.5 | Up to 16.5 |
Diagnostics
Doctors diagnose elevated bilirubin in combination with other laboratory tests (alkaline phosphatase, aspartate aminotransferase (AST), alanine aminotransferase (ALT)) associated with liver problems.
Blood test for bilirubin
The outcome of treatment for any disease largely depends on the accuracy of the diagnosis. Quite often, the doctor has to carry out differentiated diagnostics, analyzing the indicators of laboratory, instrumental and instrumental studies, since different diseases may have similar symptoms.
First of all, the doctor focuses on a biochemical blood test due to the universality of the characteristics of this complex test. Among the basic indicators, one of the most important is the content of bilirubin in the blood, which assesses the functioning of the liver, pancreas and gall bladder. The special significance of the “bilirubin” indicator and its relationship with other blood characteristics will be confirmed by any medical forum with numerous questions on this topic.
Increased bilirubin in the blood - what does it mean?
If the test results indicate an increase in bilirubin in the blood, this may indicate the presence of serious diseases and pathological conditions:
- hereditary or caused by other diseases liver enzyme deficiency;
- liver cirrhosis and hepatitis;
- diseases of the biliary tract and gallbladder;
- hemolytic anemia;
- cancer or metastases to the liver from other organs;
- vitamin deficiency B12;
- injuries with multiple hematomas.
An exception is infant physiological jaundice, which occurs due to the restructuring of the newborn’s body after intrauterine development. In all other cases, it is necessary to determine the exact cause of high bilirubin levels.
It is not always possible to identify the true disease based on one indicator, so the doctor compares the values of different indicators, obtaining more detailed information about the pathological process.
Indications for the study
A blood test for direct bilirubin is carried out during the diagnosis of liver pathologies. Its results are required to confirm diseases of the bile ducts, hepatitis, and hereditary liver diseases. The test is mandatory if there are characteristic symptoms of liver problems (jaundice, pain in the right hypochondrium, etc.). Its results are interpreted in conjunction with data from other studies. In most cases, a comprehensive examination is required for accurate diagnosis and selection of an effective treatment method.
How is bilirubin related to other blood parameters?
Bilirubin and hemoglobin
. Hemoglobin and bilirubin are substances connected by a single chain of chemical reactions, which increases interest in comparing their values in blood tests and serves as additional information in diagnosing diseases. Hemoglobin breaks down during the process of red blood cell renewal into globin chains and heme, which is converted by enzymes into toxic indirect bilirubin.
Therefore, high levels of hemoglobin and bilirubin indicate hemolytic anemia or injuries with contusions and bruises with a large number of destroyed red blood cells. If low hemoglobin and high unconjugated bilirubin are observed, then the pathology may be associated with a lack of albumin, which is responsible for moving the yellow pigment to the liver.
Bilirubin and cholesterol
. Increased cholesterol and bilirubin may indicate an incorrect dietary pattern, as a result of which the biliary system suffers, and fatty liver hepatosis is possible. As a rule, such a diagnosis is clarified after considering bile pigment fractions, other indicators from a detailed biochemical blood test, and ultrasound of the abdominal organs.
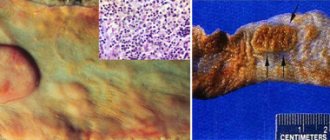
Prehepatic jaundice
An increase in the level of total bilirubin due to its unconjugated fraction is observed with intensive breakdown of red blood cells circulating in the bloodstream (hemolytic anemia), which is typical for conditions combined into the group of suprahepatic jaundice:
- Hereditary abnormalities of the red blood cells themselves (thalassemia, sickle cell anemia) and acquired variants (B12 deficiency anemia);
- Severe infectious processes (malaria, septic condition, typhoid fever);
- Ingestion of toxic substances into the body that cause destruction of red blood cells and hemolysis (salts of heavy metals, snake venom, toxins contained in toadstool and other poisonous plants);
- Extensive hematomas as a result of massive hemorrhages;
- Incompatible blood transfusion (AB0 system and Rhesus - first of all) and Rhesus conflict during pregnancy (HDN - hemolytic disease of the newborn);
- Malignant blood diseases and other neoplasias.
Hemolytic anemia is a rather serious condition: a painful appearance, pale lemon-yellow color of the skin, and an enlarged spleen immediately indicate a sick person. In addition to blood, other laboratory tests are also restless: there is a significant excess of uro- and stercobilin in urine and feces.
Table: common types of jaundice and their characteristics
Urine tests for bilirubin: bilirubinuria
In healthy people, the urine of the bile pigment bilirubin may be contained in small quantities and is not determined by standard laboratory methods. Therefore, the norm of bilirubin in urine is
is the absence of bile pigment.
Increased bilirubin in urine
In various diseases, direct and indirect bilirubin fractions can be detected in urine samples. This condition is called bilirubinuria.
Indirect bilirubin appears if its content in the blood significantly exceeds the norm and at the same time the permeability of the glomerular membrane is increased. This occurs in the following diseases:
- glomerulonephritis of various etiologies.
- Ga nephropathy (Berger disease)
- systemic lupus erythematosus;
- Henoch-Schönlein purple
- periarteritis nodosa;
- hemolytic-uremic syndrome (HUS);
- idiopathic thrombocytopenic purpura (ITP).
The cause of increased direct bilirubin in urine is jaundice. A positive reaction is detected already in cases where the bilirubin content in the blood is within 30–
34 µmol/l. This indicates a violation of the excretion of bile into the duodenum and an excess of bilirubin in the plasma in adults and children. If the general blood test for bilirubin is normal, there will be no this pigment in the urine.
The presence and absence of this bile pigment in urine in various forms of hepatitis is shown in the table:
| Type of jaundice | Try |
| Normal (healthy person) | Negative |
| Hemolytic | Negative |
| Parenchymatous, at the onset of the disease | Weakly positive |
| Parenchymatous, at the height of the disease | Strongly positive |
| Parenchymatous, in the recovery stage | Weakly positive |
| Obstructive | Positive |
How are tests done for bilirubinuria?
To determine bilirubin in urine, special tests are performed:
Gmelin's test (Rosenbach's modification) is carried out as follows: add 1-2 drops of acetic acid to 100–150 ml of urine and filter the solution several times through a paper filter. After this, the wet filter is left on the Petri dish to dry, after which a drop of a mixture of nitrous and nitric acids is applied to its surface. Increased bilirubin in the urine causes the paper to stain in the form of multi-colored concentric rings, including green, blue, purple, red on the outside and yellow in the center. Without the presence of a green ring, the sample is considered negative.
Rosin's test is carried out by adding a few drops of a 1% alcohol solution of iodine or Lugol's solution to 9–10 ml of urine taken for research. If there are bilirubin fractions in the sample, a persistent, noticeable green ring forms at the liquid interface.
To determine the amount of direct bilirubin fraction, a screening test on standard strips is also used. The level of content of this pigment is determined after applying urine to it and assessing the resulting color using the attached scale.
Testing your urine for the presence of this liver enzyme provides excellent opportunities to:
- for early detection of hepatitis and differential diagnosis of various types of jaundice;
- to determine the effectiveness of treatment in the treatment of many liver diseases;
- in the diagnosis of kidney pathologies accompanied by an increase in the permeability of the glomerular membrane;
- to monitor the presence of pigment in urine during pregnancy and preventive examination of persons working with harmful substances;
- as a quick test for liver condition in patients taking drugs that can cause liver dysfunction.
Urine tests for bilirubin are very simple, but quite informative.
List of diseases accompanied by high levels of bilirubin in the blood
Diseases in which direct bilirubin is increased:
- Acute viral hepatitis (hepatitis A, B, hepatitis in infectious mononucleosis)
- Chronic hepatitis (hepatitis C), autoimmune hepatitis
- Bacterial hepatitis (brucellosis, leptospirosis)
- Toxic (poisoning with toxic compounds, fungi), medicinal (taking hormonal contraceptives, NSAIDs, anti-tuberculosis, anti-tumor drugs)
- Jaundice of pregnancy
- Liver tumors
- Biliary cirrhosis
- Hereditary jaundice - Rotor, Dabin-Johnson syndrome
Diseases in which indirect bilirubin increases:
- Congenital hemolytic anemias - spherocytic, non-spherocytic, sickle cell, thallasemia, Marchiafava-Michele disease
- Acquired autoimmune hemolytic anemias develop against the background of systemic lupus erythematosus (symptoms, treatment), rheumatoid arthritis, lymphocytic leukemia, lymphagranulomatosis (symptoms, treatment), etc.
- Infectious diseases - typhoid fever, sepsis, malaria
- Drug-induced hemolytic anemia - provoked by taking cephalosporins, insulin, aspirin, NSAIDs, chloramphenicol, penicillin, levofloxacin, etc.
- Toxic hemolytic anemia - poisoning with poisons, insect bites, snake bites, mushroom poisoning, lead, arsenic, copper salts (copper sulfate)
- Gilbert, Crigler-Najjar, Lucy-Driscoll syndromes.
Stool test for bilirubin
The bile pigment, bilirubin, is normally found only in the stool of very young children who are breastfed. The presence of this pigment in the feces of infants gives the feces a greenish tint. This is an absolutely normal phenomenon and has nothing to do with high bilirubin in the blood of a newborn or newborn and with infantile jaundice, which is characterized by increased indirect bilirubin.
By the fourth month, microflora begins to appear in the baby’s intestines, partially metabolizing this pigment to stercobilinogen, and around nine months this substance is completely metabolized in the intestines to stercobilin and stercobilinogen.
Reasons for the presence of bilirubin fractions in stool
- In older children, positive bilirubin should not be detected in the stool, although small amounts of this substance are sometimes observed in the feces during the first year of a child's life. This is due to the instability and underdevelopment of the children's intestinal microflora.
- In adults in coprogram, bilirubin readings should be negative. Its presence, especially in combination with a decrease in the concentration of stercobilinogen, indicates the existing dysbiosis (overt or hidden) and the presence of pathogenic and microflora in the intestines.
- Another reason for the appearance of this substance in feces is dyspepsia. In the event of gastrointestinal pathologies accompanied by frequent stool disorders, the microflora is “washed out” and traces of bilirubin appear in the stool. This condition is observed in acute and chronic disorders of the gastrointestinal tract or conditions accompanied by impaired digestion of food. In such cases, in a biochemical blood test, the rate of bilirubin fractions is also increased.
- This substance may appear in the results of coprograms in acute poisoning. In this case, the functioning of the gastrointestinal tract and liver is disrupted, due to which the content of bilirubin compounds in the body increases and the evacuation of intestinal contents is accelerated. As a result, a large amount of this pigment enters the intestinal lumen and it leaves the intestine too quickly, not having time to be metabolized into stercobilin and stercobilinogen, and is found in the feces. In this case, indirect bilirubin in the blood is often increased.
How is bilirubin in stool determined?
The content of bilirubin pigment in feces is determined using the Fouche reaction; for this, a reagent is made from 100 ml of distilled water, 25 g of trichloroacetic acid and 10 ml of a 10% ferric chloride solution. A piece of feces is ground with water in a ratio of 1:20 and the reagent is added drop by drop. If there are traces of bilirubin, the test sample turns blue.
The sublimate reaction can also detect the content of bilirubin in feces, but it is less sensitive. To do this, a small lump of feces is ground in a mortar with 3–4 ml of a solution of mercury bichloride (mercuric chloride) and left in a fume hood for a day. The color of stool indicates the presence of bilirubin. Normally, the biomaterial should turn pink or reddish, however, with a positive reaction, the color of the stool turns greenish.
If even a small amount of this pigment is detected in the feces of an adult, consultation with a gastroenterologist and an infectious disease specialist is necessary, especially if at the same time the total bilirubin indicator in the blood test is increased.
Preparation and delivery
A test for bilirubin is carried out as part of a standard biochemical blood test. Therefore, the measures will be approximately the same.
- Physical activity is limited during the day. It is necessary to avoid intense exercise. It makes sense to maintain a rest regime. Because this will somewhat slow down the process of processing red blood cells. And that means bilirubin. Doctors will be able to examine the indicators as they should be.
- Two days before the test, a simple diet is prescribed. Diet changes are minimal. You need to give up fatty foods, fried, salty, smoked foods. Also from canned food and semi-finished products. Preference is given to plant foods. This way doctors will get the most accurate clinical picture.
- If possible, X-rays and CT examinations are abandoned a week in advance. This is necessary so as not to artificially increase the concentration of the substance.
- The analysis is carried out on an empty stomach. You should not eat anything for several hours before the test.
Delivery occurs using the standard method:
- The patient arrives at the appointed time to the laboratory or treatment room.
- The specialist treats the elbow bend with an alcohol solution.
- Applies a tourniquet to gain access to the vessel.
- Then he makes a puncture in the vein and draws blood.
- The sample is placed in a test tube. Containers with biomaterial are marked. Then they are sent to the laboratory for testing.
As for the analysis itself, it takes about a day. The results are delivered to your hand. You need to contact the specialist who referred them for diagnosis. Usually - to a gastroenterologist.
Bilirubin and acute and chronic liver failure (hepatargia)
Liver failure occurs with pronounced changes in the liver parenchyma (fibrous, dystrophic or necrotic). Depending on the speed of occurrence, acute and chronic forms are distinguished.
With hepatargia, the detoxification function of the liver sharply decreases, due to which endotoxins, which should have been eliminated, penetrate into the blood and cause poisoning of the body. In the blood, direct and total bilirubin increases to critical levels (260–350 µmol/l), which causes damage to the central nervous system. The mortality rate is 50–80%. Liver failure can be acute or chronic. The degree of danger is determined through tests for bilirubin.
Causes of hepatargia
- The condition is often a consequence of the development of viral hepatitis and liver cirrhosis. In this case, the presence of slowly progressive hepatargia is characteristic. Hepatitis and cirrhosis can be asymptomatic for a long time, and the norm of direct bilirubin in the blood may not be exceeded for a long time;
- Sometimes the cause is infection of a person with Epstein-Barr viruses, herpes, adenovirus, etc. When a woman is infected with cytomegalovirus, intrauterine infection of the fetus occurs and its death. In this case, total bilirubin is increased during pregnancy.
- The most common cause of this condition is exposure to poisons and medications. In some cases, poisoning occurs due to the use of drugs in the wrong dosage, and sometimes it is a consequence of a failed suicide. In this case, the process develops acutely and is accompanied by nausea, vomiting, hemorrhagic syndrome, “hepatic” bad breath, neuropsychiatric disorders, and increased total bilirubin in the blood.
- Very often this condition is associated with the presence of malignant tumors in the body. Both the main focus and metastasis to this organ can be observed in the liver. In cancer, symptoms increase gradually, accompanied by severe jaundice, nausea, vomiting and cachexia. At the beginning of the development of the tumor process, there may be a normal level of bilirubin - 7-18%, but gradually its concentration in the blood increases and it begins to exceed the norm by 10-15 times.
- Another cause of liver failure is alcohol and drug abuse. In this case, the process can proceed either quickly or slowly, it all depends on the specific version of the “predilection”. However, over time, the increased bilirubin still exceeds the norm many times over.
Symptoms of hepatargia
With this pathology, they gradually increase; jaundice, edema, weight loss, fever, telangiectasia, and dull abdominal pain. “Liver signs” appear on the body: palmar erythema, hemorrhages, Chistovich’s stars, varicose veins of the abdomen in the form of a “jellyfish head”.
Later they are joined by: severe bad breath, neurosis, apathy, and unstable emotional state. Slurred speech, writing problems, finger tremors, and poor coordination may occur. A general blood test and biochemistry show significant deviations from the norm.
With further progression of failure, hepatic coma occurs. Its precursors are: drowsiness, lethargy, rigidity of skeletal muscles, confusion, muscle twitching, convulsions, uncontrolled urination. Very high levels of liver tests are observed in the blood. A general blood test for bilirubin can show up to 500 µmol/l. Patients fall into a coma and die.
In order not to become victims of this disease, you need to take care of your liver, monitor your health, periodically get tested, and if the biochemistry is “bad” and total bilirubin is increased, the reasons for this phenomenon need to be found out. You should not self-medicate, because only a doctor knows exactly what bilirubin and other blood parameters should be.
The dangers of hyperbilirubinemia and how to eliminate it
Products of bilirubin metabolism have toxic properties to body tissues. Toxic damage to the brain and heart deserves special relevance. The severity of pathological influences is directly proportional to the degree of hyperbilirubinemia. A marked increase in the level of total bilirubin (more than 170 µmol/l) threatens the development of hepatic encephalopathy, renal and cardiopulmonary failure. Hyperbilirubinemia greater than 300 µmol/l can be fatal.
Treatment methods for disorders of bilirubin metabolism depend on the specific type of jaundice and can be represented by detoxification therapy, massive infusions, diuretics, hepatoprotectors, glucocorticoid hormones and surgical treatment.
Author of the article:
Gorshenina Elena Ivanovna |
Gastroenterologist Education: Diploma in General Medicine received from the Russian State Medical University named after. N. I. Pirogova (2005). Postgraduate course in the specialty "Gastroenterology" - educational and scientific medical ]Our authors[/anchor]
Physiological and pathological jaundice in newborns
Jaundice (jaundice) in newborns is associated with the breakdown of fertile hemoglobin in the first days of life. It can be physiological and pathological. With physiological jaundice, its manifestations go away on their own and the general condition of the newborn does not suffer. The concentration of total bilirubin is normal in children in this case; it increases only due to its unbound fraction. To determine the extent of the problem, children are tested for bilirubin.
Severe physiological jaundice
If the norm of free bilirubin is significantly exceeded, the general condition of the child may suffer. Such babies are lethargic, lethargic, suck poorly, they may develop a fever and vomit. However, the condition of the newborn should be judged not by these signs, but by the bilirubin level.
When total bilirubin in newborns exceeds the norm significantly, albumin produced by the children's liver cannot completely conjugate it and it penetrates the central nervous system through the blood-brain barrier. In this case, this pigment, which is, in fact, poison, has a toxic effect on the brain. As a result, the baby may subsequently develop paralysis, mental retardation, deafness and blindness.
What happens to bile pigment after it is formed?
Thus, red blood cells, when destroyed, “release” their contents - hemoglobin, the molecule of which also disintegrates with the formation of a toxic substance, the hemoglobinogenic pigment - bilirubin. The liberated bilirubin in this state cannot accumulate, be stored in organs or circulate in the blood, so it must be sent to a place where it will be converted into a water-soluble form that can leave the human body. Everything here is provided by nature:
- To transport the “newly created” toxin to the liver, not to lose it along the way and thereby prevent its excessive accumulation in tissues, you need a strong assistant. This role in the body is played by one of the most important blood proteins - albumin, which immediately captures bilirubin and forms a strong complex compound with it (albumin-bilirubin complex). In short, albumin becomes a carrier for bilirubin, delivering it to its destination “safe and sound.”
diagram: metabolism of bilirubin in the body - Delivered to the liver as part of a complex, bilirubin cannot enter hepatocytes, therefore, on the membrane of the liver cell, it leaves its “vehicle”, becomes independent and is able to freely penetrate the membranes of the endoplasmic reticulum of hepatocytes.
- In the endoplasmic reticulum of the liver cells, glucuronic acid awaits “our hero”, with which it interacts and binds to it (conjugation), forming a new water-soluble species called bilirubin-diglucuronide and capable of being excreted in bile and urine.
- The further fate of bilirubin is associated with the excretion of conjugated bilirubin with bile into the intestine (excretion), where it is converted into urobilinogen. Those who are “lucky enough” to have hepatitis know that there is such a test as stool for stercobilin - this is the end product of bilirubin metabolism.
Based on these transformations, we can conclude that all bile pigment (total bilirubin) consists of:
- Indirect (unbound, free, unconjugated), which appears during the destruction of red blood cells and the breakdown of heme components;
- Direct (bound, conjugated), formed in the liver as a result of a reaction with glucuronic acid.
The condition when bilirubin is elevated is called hyperbilirubinemia
. Total bilirubin can increase due to any of its fractions (bound, free), so blood tests provide methods for their determination.
Video: bilirubin metabolism
Treatment of jaundice
In order to prevent such complications, in case of severe and protracted jaundice, it is necessary to carry out specific treatment.
Previously, children were infused with various solutions to normalize bilirubin levels, but this has now been abandoned. Now light therapy is carried out, during which the newborn’s skin is illuminated with a special installation. Under the influence of light, the pigment decomposes and is removed from the body. Such children are monitored by neonatologists until direct bilirubin returns to normal. Most often, it is possible to normalize bilirubin in 9 days or less.
A great way to overcome jaundice is to start breastfeeding your baby as early as possible, because colostrum helps to pass meconium and cleanse the newborn’s intestines.
It has been noted that this condition is more often observed in children born prematurely, with multiple pregnancies and difficult births. Children born to mothers suffering from chronic diseases such as diabetes are susceptible to jaundice. Contrary to popular belief, an increased bilirubin level in the mother during pregnancy and yellowing of the skin in the newborn baby are absolutely unrelated.
Bilirubin tests reveal pathological jaundice
This type of pathology in newborns manifests itself in the first days of life. Such a baby may have: acholic feces, dark urine, hemorrhages and bright yellowness of the skin and sclera. In contrast to physiological hyperbilirubinemia, when it occurs pathologically, the norm of direct bilirubin in the blood is noticeably exceeded. In this case, a comprehensive examination and treatment is necessary.
The causes of the phenomenon are most often known:
- Incompatibility of the blood of mother and baby by group and Rh factor can cause hemolysis of red blood cells and icteric staining of the sclera of the newborn.
- Sometimes a child becomes infected with the hepatitis virus or protozoa from the mother and develops an infection. In this case, specific therapy is carried out for mother and baby, since the rate of total bilirubin in a woman is also increased in this case due to infection.
- Due to congenital abnormalities of the liver and biliary tract, obstructive jaundice may occur, characterized by an increase in direct bilirubin levels by 6 or more times. Only surgeons can help here.
- There is a large group of hereditary hyperglobulinemias (Crigler-Najjar, Dabin-Johnson, Rotor syndromes), which are caused by genetic metabolic defects. In this case, you need to prepare for long-term diagnostics and lifelong maintenance therapy.
Only a doctor can accurately diagnose jaundice in newborns and find out its cause. The diagnosis can only be made based on test results.
Total bilirubin is reduced: reasons
If total bilirubin is low, this may mean the patient has:
- anemia (decrease in red blood cells and hemoglobin), except hemolytic;
- acute leukemia (blood tumor);
- tuberculosis infection;
- chronic renal failure.
Violations of the rules for donating and storing blood cause a decrease in indicators:
- drinking alcohol, coffee before analysis;
- taking medications (sedatives, antibiotics, hormones, anticonvulsants, painkillers);
- The serum was exposed to light before measurement.
If total bilirubin is low, but there is yellowing of the skin, then the test must be repeated, and the diagnosis must be repeated again if the activity of liver enzymes increases.
Why does total bilirubin increase in an adult?
If total bilirubin is elevated in an adult, this may indicate several types of problems, for example:
- Abnormal breakdown of red blood cells (eg, reaction to blood transfusion (intravascular administration of whole blood or its components from a healthy person to a sick person));
- Scarring of the liver (occurs when there is an overgrowth and restructuring of the connective tissue structure in the large digestive gland, in diseases such as cirrhosis and liver fibrosis);
- Inflammatory processes (cause hepatitis A, B, C);
- Penetration of pathogenic (disease-causing) microorganisms into the body;
- Dysfunction of the common bile duct;
- Gallstones, or calculi;
- Malignant neoplasms (cancer, tumors) arising from the epithelium of glandular tissue or pancreatic ducts
Reasons for low value
A substance in the blood that does not reach the average level can be caused by:
- Medications and supplements that reduce overall levels (vitamin C, phenobarbital and theophylline).