The inflammatory process in the area of venous structures is often accompanied by the formation of a blood clot. Pathological changes are characteristic of thrombophlebitis of the extremities. The disease is accompanied by the development of serious complications, which in some cases can cause death. Treatment of thrombophlebitis of the lower extremities is recommended at the initial stage of development of dysfunctions - when primary symptoms appear. In order to get a more accurate idea of this disease, you can read real reviews of people who had to go through it.
What is thrombophlebitis
Thrombophlebitis
(acute thrombophlebitis, superficial vein thrombosis, TPV) is an inflammation of the venous walls with further formation of blood clots. The thrombus is tightly attached to the inflamed vessel. If treatment is started in time, the blood clot will resolve, the inflammation will go away, and the venous lumen will be restored and will not affect blood flow.
The incidence of thrombophlebitis is determined by many factors, one of which is age. Thus, superficial vein thrombosis debuts annually in 0.3-0.6 per 1000 people under 30 years of age and in 0.7-1.8 per 1000 elderly patients. There are also gender differences. In men under 30 years of age, acute thrombophlebitis occurs in 0.05 cases per 1000 patients annually. For women, these figures are significantly higher. Thus, in the first 30 years of life, the onset of TPV is detected in 0.31 per 1000 women, but with age the detection frequency increases to 2.2 per 1000 patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
In 3-11% of patients, thrombophlebitis is localized on the lower extremities. The system of the great saphenous vein is affected in 60-80% of cases, the small saphenous vein - in 10-20%, and bilateral TPV occurs in 5-10% of cases i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
Against the background of varicose veins, thrombophlebitis occurs in 4-62% of patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
Thrombosis - treatment with folk remedies
The possibility of treating thrombosis with folk remedies should be discussed with your doctor. Patients with a tendency to form blood clots need to eliminate the causes of leg swelling. Regular physical activity prevents congestion in blood vessels. The most beneficial for varicose veins and venous insufficiency are walking, cycling, and swimming.
Overheating and prolonged exposure to the sun should be avoided. To relieve tension from diseased vessels, you need to raise your legs up so that they are above the level of the heart with support along the entire length of the lower leg.
Types (classification) of disease
Thrombophlebitis is divided into several types, taking into account the origin and origin of the disease, the localization of the lesion, and the extent of the lesion.
Venous thrombophlebitis is divided according to the affected area into:
- Migratory
. A blood clot appears in one place. Over time, it disappears and appears in another area. The condition is dangerous and requires prompt medical attention. - Local
. A blood clot forms in a specific area. It doesn't have to be the shins. For example, thrombophlebitis of the hand is diagnosed.
Depending on the presence or absence of pathogens, subcutaneous thrombophlebitis occurs:
- Septic
. The infection spreads quickly through the bloodstream, so there is a risk of developing sepsis. Diagnosed after childbirth, surgery and erysipelas. Treated with antibiotics. - Aseptic
. There is no infection, the disease occurs after injury. Most often, varicose thrombophlebitis is diagnosed due to improper or absent treatment.
Depending on the size of the blood clot, the disease can be:
- Occlusive
. The lumen of the vein is completely blocked, so the outflow of blood is impaired. There is a risk of necrosis (tissue death), so immediate surgery is required. - Non-occlusive
. An attached blood clot partially blocks the venous lumen. Blood circulates.
Based on the extent of the pathological process, the following is revealed:
- Thrombophlebitis of the superficial veins
. Symptoms appear immediately. The patient complains of pain along the vein. The surrounding skin turns red and thickens. Over time, swelling forms, which is difficult to eliminate. The temperature is kept within 39 °C. Treated with medication. - Deep vein thrombosis
. This form is detected less frequently and is more severe. The symptoms are the same, but their severity is stronger. The limbs become very swollen and turn blue. If there is a high risk of developing pulmonary embolism, surgery is performed.
First, thrombophlebitis of the superficial veins of the lower extremities develops. If left untreated, the disease develops into deep vein thrombosis, thrombophlebitis of the great saphenous vein.
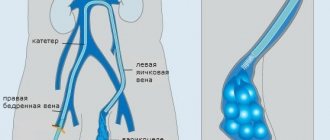
Deep vein thrombosis of the lower extremities: diagnosis
At the appointment, the specialist visually assesses the patient’s condition and also applies special diagnostic methods. If symptoms of deep vein thrombosis are detected, a special test is performed. The person is asked to raise his foot towards himself: if his lower leg hurts, the diagnosis is indirectly confirmed.
Diagnosis of deep vein thrombosis
Two main methods are used in diagnosing the disease. This is a blood test through blood sampling and duplex examination. Rarely, duplex scanning does not give an accurate result, especially if the thrombus is located too high; X-ray contrast venography is used, injecting special drugs into the vein. This method allows you to reliably determine where the blood clot is located. Sometimes additional diagnostic methods are used if the diagnosis needs to be confirmed.
!
At the first stage, ultrasound diagnostics of the veins is usually performed.
Stages
The sequence of development of the disease is as follows:
- Acute stage
. Clinical signs of thrombophlebitis are bright and appear unexpectedly. The temperature rises, the skin around the affected area turns red, and the patient shudders. If treatment is started within two weeks, the development of the disease can be avoided. The blood clot will dissolve. The duration of exacerbation is up to one month. - Subacute stage
. Lasts up to two months. Signs of the disease subside, but do not fade away. The skin remains red and the swollen veins turn blue. The swelling goes away, but the seals remain. - Chronic stage
. Diagnosed two to three months after the disease is detected. Symptoms are either absent or worsened. During remission, the limbs remain swollen, quickly become tired and itchy, but there is no pain. Discomfort occurs in the lower extremities when walking for a long time.
Massage
Massage for thrombophlebitis of the lower extremities. In the acute stage of thrombophlebitis or phlebothrombosis, massage is contraindicated due to the risk of developing pulmonary embolism. Massage is useful during the rehabilitation stage and as a prevention of thrombosis. It affects blood capillaries, improves overall lymph and blood flow. The main massage techniques for venous insufficiency are stroking and rubbing the limb.
Stroking should be performed along the vein, starting from bottom to top. It helps increase blood flow, has a training effect on blood vessels, and reduces swelling. An auxiliary element of stroking - rubbing - is also used along the flow of lymph. Techniques are performed with both hands, clasping the limb on both sides in the shin area, gradually moving to the groin area.
How is thrombophlebitis different from varicose veins?
Varicose veins are increased pressure in thinned and inelastic veins, and thrombophlebitis is an inflammation of the venous walls with subsequent formation of blood clots. Most often, the diagnosis of thrombophlebitis is a consequence of varicose veins.
Thrombophlebitis differs from varicose veins in the following symptoms:
| Sign | Varicose veins | Thrombophlebitis |
| Pain | pulling | bursting and stabbing |
| Convulsions | Yes | No |
| Changing the appearance of your legs | noticeable tortuosity and bulging of veins | compactions and lumps when palpated |
| Change in skin color | pale skin, blue veins | red skin |
| Burning feeling | Yes | No |
Both pathologies develop as a result of impaired hemostasis, but inflammation of the venous walls is more often associated with the entry of an infectious agent. The difference is the absence of local inflammation. With varicose veins, the veins do not become inflamed. In this case, only the blood circulation is disrupted.
Exercises
If you have a “standing” or “sedentary” job or suffer from varicose veins, then be sure to perform several exercises daily to prevent thrombophlebitis.
- Unloading of veins. Place your feet on the pillow so that they are elevated at a 20-degree angle. Stroke them from the feet to the thighs. This exercise is suitable even for pregnant women and patients who are forced to remain in bed.
- Bike. Lying on your back, pedal imaginary bicycles.
- Rotation of the feet. Lying on your back, lift your legs vertically up. Rotate your feet alternately or simultaneously.
- Scissors. Lying on your back or sitting on a chair, raise your legs. Alternately cross and breed them.
- Move your fingers. Straighten your legs while sitting or lying down. Bend and straighten your toes.
- Calf raise. Stand straight, feet together, palms pressed to your thighs. While inhaling, rise onto your toes, and while exhaling, lower to the starting position.
Perform each exercise 3-5 times in the morning and evening.
Causes and risk factors for the development of thrombophlebitis
Thrombophlebitis of the lower extremities rarely begins spontaneously. Most often, the disease becomes a complication of leg diseases. The development mechanism is associated with improper outflow of lymph and blood through the veins and vessels. After injury to the inner layer of the vein, bleeding begins. In response to this, a blood clot forms. It prevents blood loss, but over time it grows and completely blocks the lumen of the vessel, preventing blood from circulating.
The following factors precede this process:
- Damage to the vascular wall. This group includes mechanical injury to veins due to trauma and compression of the limbs. Venous walls are damaged when injections are performed incorrectly, frequent and long IVs, or operations.
- Deterioration of blood supply to certain areas of the body. The blood flows poorly due to wearing a cast for a long time, bed rest and physical inactivity. Less commonly, slowing of blood flow occurs as a result of heart failure.
- Improper flow of blood in the veins due to venous insufficiency. The complication develops against the background of pregnancy and diseases of the pelvic organs.
- Increased blood clotting. The viscosity and homogeneity of blood and plasma change with long-term use of hormonal drugs, discrepancies in the levels of estrogen and progesterone, and infections.
Other causes of thrombophlebitis may be:
- obesity;
- allergic reactions and sensitization;
- a history of venous thromboembolic complications (VTEC);
- taking a number of medications (diazepam, amiodarone, vancomycin, chemotherapy drugs, heroin addiction).
Acute thrombophlebitis often develops against the background of some autoimmune diseases, such as systemic lupus erythematosus, vasculitis, Behcet's and Buerger's diseases. In particular, in Behçet’s disease, TPV is detected in 53.3%, and DVT in 29.8% of patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
The risk group includes:
- Patients with heart disease - chronic heart failure, ischemic stroke. Limbs swell, motor activity decreases, and after a stroke there may be paralysis, which impedes the flow of blood through the veins.
- Patients with concomitant phlebological diseases - varicose veins, venous thrombosis. The speed of blood movement in the veins decreases, the blood stagnates, forming a blood clot.
- Bedridden patients, people with complex fractures. Their mobility is impaired and the likelihood of blood clot formation increases.
- People with a hereditary predisposition. Hemostasis disorders are transmitted genetically. The likelihood of the disease is increased if blood flow pathologies are detected in first-degree relatives.
Causes
Thrombophlebitis is more common in women aged 40-50 years. During this period, there is a sharp deterioration in the condition of vascular structures, which increases the risk of developing inflammation. The disease can also occur in young people. The lower extremities are most often affected, since they bear the main load.
Thrombophlebitis has a complex pathogenesis, in which the following factors take part:
- slow blood flow and varicose veins of the lower extremities;
- addition of a secondary infection and pelvic tumor;
- increased coagulability, blood viscosity and obesity;
- damage to the venous walls or valve apparatus;
- pregnancy and postpartum period, trauma;
- use of hormonal contraception and alcoholism;
- systemic pathologies and long-term venous catheterization.
Photo: Thrombophlebitis of the extremities - symptoms and treatment
Separately, the cause of thrombophlebitis of the extremities should be highlighted as a sedentary lifestyle. In the absence of proper physical activity, muscle structures weaken. In this case, blood clots can reach large sizes. This is fraught with disruption of blood circulation processes. When physical damage to venous structures occurs, when a catheter or needles are inserted, chemical or bacterial irritants enter the bloodstream, which is fraught with the development of pathological changes.
Emergence process
These factors lead to the formation of a blood clot, which consists of red blood cells, fibrin strands and a small number of platelets. One side of the blood clot is attached to the venous wall, and the other is free floating. As the disorders occurring in the body progress, the length of the blood clot increases to 15-20 cm. The head is fixed mainly in the area of the venous valve. The tail can fill almost the entire length of the vein. In this case, the thrombus is called floating (floating).
In the first day after the formation of a blood clot, there is a high risk of its rupture, which is fraught with pulmonary embolism, which in 15% of cases ends in death. After 5-6 days, inflammation occurs, which strengthens the blood clot, thereby reducing the likelihood of separation.
Symptoms
Signs of thrombophlebitis appear immediately. The disease can be suspected based on the following clinical picture:
- the limb swells;
- the skin over the inflamed vein turns red, and the vessel itself darkens and is clearly visible under the skin;
- a compaction is felt to the touch along the course of the vessel;
- there is a feeling of heaviness in the legs and bloating of the veins;
- in a supine position, the patient cannot lift his leg and rotate his foot;
- The leg is cold to the touch.
At the initial stage, the symptoms are local, that is, the general condition does not change. As the disease progresses, mobility becomes impaired. The patient notes weakness in the legs and cannot stand for a long time. When bending the foot, he feels tension in the lower leg and thigh. Temperatures range from 37°C to 39°C.
Distinctive signs of thrombophlebitis of the lower leg are that the calf muscle turns blue and the veins on it swell. The pain is so severe that the patient cannot step on his foot.
Thrombosis of the iliofemoral vein is manifested by pain in the lumbosacral spine, pain in the groin and the lower third of the abdomen on one side.
Femoral vein thrombosis is characterized by swelling of the veins in the upper thigh and discomfort in the groin area.
Traditional therapy
Photo: Folk remedies for thrombophlebitis - honey
Treatment of thrombophlebitis of deep and superficial veins can be carried out using alternative medicine. Please note that this approach to combating the formation of blood clots in the veins can only be used in the initial stages of progression or in combination with medications.
The most effective methods of traditional therapy:
- Bee products. Dead bees and natural honey remove blood clots well. It is recommended to use dead fruit in the form of an alcohol compress, and fresh beekeeping product - for oral consumption, 1-2 tbsp. l. per day.
- Apple cider vinegar. The product should be homemade. It should be used to rub the affected area, diluted with water in a ratio of 1:3.
- Herbal infusions. It is recommended to take medicinal herbs such as exuzan, clover and nettle orally. Infusions have a beneficial effect on the circulatory system, strengthen and restore the entire body.
Before using traditional medicine, be sure to consult your doctor. This eliminates the possibility of complications.
Diagnosis of thrombophlebitis
Diagnosis of the condition of the lower extremities includes:
- Vascular ultrasound in Doppler mode
. The blood flow of the superficial and deep veins is analyzed. Areas of narrowing of the vascular lumen and slowing down of blood flow are identified. - CT venography
. The transition of the femoral vein to the iliac vein is poorly visualized on ultrasound, so computed tomography shows a splash of blood after slow passage through a certain area. It is carried out with contrast enhancement, that is, a dye is injected into the vein. - D-dimer assay
. When a blood clot forms, the amount of fibrin breakdown products in the blood increases. The analysis is performed after an ultrasound. - Blood analysis
. The diagnosis is confirmed by high coagulogram (clotting test) values. The presence of C-reactive protein indicates inflammation. Leukocytes also grow, ESR increases, and the number of rods in the blood increases.
Complications and prognosis
Complications of superficial thrombophlebitis occur extremely rarely. It is dangerous when a blood clot breaks off and leads to thromboembolism.
However, unlike deep vein thrombosis, which is rarely accompanied by inflammation, superficial thrombophlebitis is usually accompanied by an acute inflammatory reaction, causing the clot to adhere to the vessel wall. The likelihood of it breaking off and entering the bloodstream is very low. In addition, superficial veins, unlike deep veins, are not surrounded by muscles, the contractions of which contribute to compression and displacement of the blood clot, which can lead to its separation. For these reasons, superficial thrombophlebitis is rarely complicated by thromboembolism. However, the possible complications of superficial thrombophlebitis are as follows.
Be sure to tell your doctor that despite treatment for superficial thrombophlebitis, the symptoms do not decrease or increase. Also report any new symptoms such as fever, chills, paleness, or swelling of the extremity. A change in skin color at the site of thrombophlebitis may remain noticeable for a long time after treatment; this is not a pathological symptom.
Treatment of thrombophlebitis
Therapeutic actions are aimed at suppressing inflammation, resolving blood clots and thinning the blood.
Drug treatment
venous thrombophlebitis involves taking:
- anticoagulants to thin and prevent blood clotting, in the acute phase are prescribed by injection;
- antibiotics for the infectious nature of the disease;
- angioprotectors to increase the tone of the veins, reduce venous stagnation;
- disaggregants for breaking down cells that form a blood clot;
- phlebotonics to strengthen and increase the elasticity of the walls of blood vessels;
- non-steroidal analgesics to relieve acute pain.
Compression therapy
using bandages, elastic stockings or class 2 sleeves accelerates blood flow in the superficial and deep veins, thereby preventing the growth of a blood clot. In addition, compression has an analgesic effect.
Physiotherapy
– an effective method of treating venous thrombophlebitis. After acute symptoms have been relieved, a course of magnetic therapy, infrared radiation, ultraviolet radiation, or darsonvalization of your choice is prescribed. The procedures reduce inflammation, increase blood circulation, and accelerate the regeneration of the internal walls of veins.
Surgical intervention
is prescribed if the blood clot grows and the threat of blocking the lumen of the vessel increases. There are several types of operations for thrombophlebitis:
- crossectomy – access to the saphenous vein through the groin and an incision in the thigh;
- thrombectomy – access to the thrombus through one incision;
- invagination stripping - with the help of a probe, the vein is everted, the blood clot is removed;
- stenting – the vein is expanded mechanically by installing a special balloon.
Prevention
When the disease is diagnosed, timely treatment and prevention of disease progression are important. To do this, you need to contact a specialist in time and undergo a course of treatment.
Prevention is also:
- active lifestyle and sports;
- timely treatment of varicose veins;
- rejection of bad habits;
- balanced diet and limiting the consumption of fatty foods;
- identification and elimination of foci of infection in the body.
A favorable outcome of the disease is possible only if you consult a doctor and undergo appropriate treatment.
Recommendations and contraindications for thrombophlebitis
The doctor advises you to follow a diet and wear low-heeled shoes with a comfortable last.
Forbidden:
- wear stilettos and heels higher than 3 cm;
- massage limbs;
- go to the gym and lift weights;
- remove leg hair with wax or epilator;
- go to the bathhouse and sunbathe;
- wear socks, stockings, and knee socks with a thick elastic band.
It is necessary to exclude the use of hormonal drugs and choose a different method of contraception.
Dietary recommendations
Photo: Diet for thrombophebitis
Among the most common causes of thrombophlebitis of the extremities, obesity should be highlighted. Persons with a predisposition to disease of venous structures should limit the consumption of certain foods. For the period of treatment or as a preventative measure, it is recommended to avoid spicy, fatty and fried foods. It is best to eat dietary meat (rabbit, chicken and turkey). Every day the menu should include vegetables and fresh fruits, except bananas. Among the unacceptable products are legumes (beans, peas).
During the spring-winter period, it is recommended to take a multivitamin complex. Every day, as a preventive measure, you can eat 1 clove of garlic, and be sure to include onions in your diet.
Thrombophlebitis of the extremities is a dangerous disease that can be prevented. Adhere to the right lifestyle - walk, give up alcohol and smoking, eat right and follow a daily routine. To maintain the tone of blood vessels, you should drink cranberry juice or St. John's wort tincture. Avoid static tension (staying in one position for a long time), drink at least 1.5-2.0 liters of water per day. In the initial stages of thrombophlebitis of the extremities, do not visit the bathhouse or sauna. Wear the most comfortable shoes possible, preferably orthopedic. When resting, try to elevate your legs, for example, by placing a pillow under them.
Sources
- Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23.
- Kuzmichev D.E. Pathomorphological findings. Thrombophlebitis / D.E. Kuzmichev [et al.] // Health care of Ugra: experience and innovations. - 2020. - No. 1. - P. 53-56.
- Marushchak E.A. Modern methods of ultrasound diagnosis of venous thrombosis of the inferior vena cava system / E.A. Marushchak, A.R. Zubarev // Outpatient surgery. Stationary replacement technologies. - 2014. - No. 3-4 (55-56). — P. 38-47.
Examination methods
An important aspect in identifying the disease is differential diagnosis to exclude:
- manifestations of lymphangitis caused by inflammation of lymphocapillary vessels;
- erysipelas; inflammatory processes;
- subcutaneous purulent phlegmon;
- inflammatory diseases of subcutaneous adipose tissue – erythema nodosum;
- manifestations of allergic dermatitis.
Diagnostic research includes visual, laboratory and instrumental examination.
Laboratory diagnostic methods are based on examination of blood from veins and capillaries, and the coagulogram method.
- The study of capillary blood gives a picture of inflammatory processes and reveals the ability of the hematopoietic organ (bone marrow) to continue to produce blood cells normally. Indicators of the leukocyte form and the quantitative indicator of platelets determine the causative factor of possible blood thickening. Biochemical indicators of venous blood provide an answer about the presence of concomitant diseases.
- The coagulogram method (hemostasiogram) diagnoses any disorders in blood clotting.
- The instrumental diagnostic method - Doppler sonography, is the most reliable examination, giving a complete picture of venous lesions.
Dietary nutrition for illness
There is no diet as such for thrombophlebitis. But doctors identify a number of foods that are useful for patients with this diagnosis, and a number that need to be excluded from the diet.
For thrombophlebitis, it is recommended to increase the consumption of the following foods:
- some types of vegetable oils (olive, sesame, flaxseed);
- fruits and vegetables rich in vitamin C;
- fermented milk products (yogurt, fermented baked milk, kefir);
- in the absence of gastrointestinal diseases, garlic and onions.
An increased consumption of foods containing magnesium and fiber is recommended - oatmeal, cashews, soy, buckwheat.
Minimize or, if possible, eliminate the consumption of foods containing vitamin K, as it reduces the effectiveness of anticoagulants. You should also stop eating fried foods and switch to steamed or boiled foods.
It is mandatory to completely avoid drinking alcoholic beverages and smoking, as this can worsen the condition of the veins and also reduce the effectiveness of therapy.
Contrast venography
A method of direct staining of deep veins using the injection of a contrast agent under x-ray control. Phlebography is performed immediately before endovascular intervention for venous thrombosis. In our clinic, the study is carried out with a safe contrast agent - carbon dioxide, which does not have a harmful effect on the kidneys. Phlebography allows you to answer questions about the localization of blood clots, the mechanical reasons for their formation, and the condition of bypass tracts. During phlebography, the surgeon can perform interventions such as installing a vena cava filter to prevent pulmonary embolism, dissolving blood clots, or installing a stent in the area of narrowing of the deep vein.