Rheumatoid arthritis is a systemic pathology of connective tissues with autoimmune pathogenesis and unclear etiology, predominantly affecting small joints as erosive-destructive polyarthritis. The clinical picture of the disease contains both articular and extra-articular signs. Rheumatoid arthritis is characterized by symmetrical involvement of joints in the pathological process, leading to their severe deformation. The disease manifests itself as serositis, the formation of subcutaneous nodules, lymphadenopathy, and vasculitis.
To diagnose rheumatoid arthritis, instrumental and biochemical studies are performed. The most informative is radiography, the results of which allow one to assess the degree of damage to connective tissue and bone structures. Conservative treatment consists of a long course of taking drugs from various clinical and pharmacological groups. As the pathology progresses, surgical restoration of the joints is required.
Etiology of the disease
The etiology of rheumatoid arthritis is not fully understood. However, studies have shown that hereditary predisposition plays a major role in its occurrence. Considering that with rheumatoid arthritis, a general blood test shows an increase in ESR and the number of leukocytes, the process is infectious in nature.
According to many scientists, the disease occurs due to the entry into the body of infectious agents that disrupt the functioning of the immune system and form immune complexes with antibodies or viruses in individuals who have a genetic predisposition to this. These immune complexes are deposited in the joint area, causing joint damage. Rheumatoid arthritis in most cases leads to disability of patients, and sometimes can even cause death (if infectious complications and renal failure occur).
Respiratory diseases (including influenza and tonsillitis) in 40% of cases precede an exacerbation of rheumatoid arthritis and are its provocateurs. Sometimes the appearance of inflammation is preceded by injury, general hypothermia, hormonal changes, heavy physical activity, stress (dismissal from work, health problems, divorce, death of loved ones), overwork, and other adverse environmental factors.
Nutrition
A specialized diet followed during illness will help reduce the size of the inflammatory process and regulate metabolic failures.
To begin with, you should limit your consumption of foods that can cause food allergies. Such products include citrus fruits, potatoes, eggplants (little blue ones), tomatoes, peppers, cow's milk, and cereals.
With this pathology, eating meat leads to a worsening of the condition. Therefore, it is recommended to exclude meat dishes from the diet.
An alternative to meat can be dairy products and fatty fish, or even prefer vegetarianism. Fruits and vegetables should be included in your diet in unlimited quantities.
Following a diet for this type of disease makes it easier to withstand treatment with medications. That is why patients are advised to exclude products that have a negative effect on the normal functioning of internal organs.
Excluded: spices, canned food, strong broths, fats, food additives, coffee, black tea, chocolate, cocoa, and carbonated drinks. Avoid fried, salty and spicy foods. It is better to give up nicotine and alcoholic beverages forever.
Due to a decrease in physical activity, the patient often becomes overweight, which has an adverse effect on diseased joints. Therefore, it is worth reducing the amount of refined carbohydrates consumed, contained in flour products, granulated sugar, margarine, and taking less meals containing a large amount of fat.
The diet should include dishes containing large amounts of calcium.
Main symptoms
Rheumatoid arthritis has distinct individual symptoms that prevent it from being confused with other diseases:
- The appearance of inflammatory swelling of the metacarpophalangeal joints of the index and middle fingers of both hands, and inflammation of the wrist joints is also possible. The damage to the joints is symmetrical (appears almost simultaneously on both hands).
- The appearance of pain in the joints, which intensifies at night and closer to the morning. Joint pain usually bothers patients in the first half of the day; in the afternoon it decreases and disappears altogether. At night, at about 3 o'clock, the pain intensifies and does not go away until the morning.
- There is symmetrical damage to the small joints of the legs (usually at the base of the toes) with pain when pressing the pads of the toes.
- As the disease progresses, inflammation of larger joints (knees, shoulders, elbows, ankles) occurs. It should be noted that some forms of arthritis occur with damage not to small, but to large joints, which are later joined by damage to small joints (more common in older people).
- Patients with rheumatoid arthritis are characterized by morning stiffness in the affected joints (a feeling as if the joints are “stiff” or are in tight gloves or boots). The feeling of stiffness is noted for several hours after waking up, after which it completely disappears or decreases.
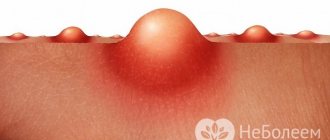
- In the area of the bends of the elbows, feet, and hands, dense subcutaneous formations appear - rheumatoid nodules, which usually do not exceed the size of a pea. Rheumatoid nodules are a cosmetic defect; they usually do not cause concern to the patient and can change their size over the years, disappear and reappear.
- Symptoms of rheumatoid arthritis are characterized by signs of intoxication of the body (feeling of weakness, decreased appetite, increased or decreased body temperature, weight loss).
- The pronounced picture of rheumatoid arthritis is accompanied by persistent deformation of the hands and fingers. The so-called ulnar deviation of the hands appears - the hands and fingers deviate outward, mobility in the joints is limited, and they become fixed in an incorrect position. Over time, blood circulation and innervation of the hands become impaired, skin becomes pale and muscles atrophy.
As the disease progresses, inflammation affects more and more joints. The more joints are involved in the inflammatory process, the more severe the stage of the disease. Particularly troublesome is caused by the inflammatory process in large joints, in which the feeling of discomfort is manifested by particular stiffness and the inability to carry out active full movements.
Over time, patients may develop a Baker's cyst - a formation in the knee joint caused by the accumulation of excess fluid in the joint capsule, which causes it to stretch. Rheumatoid arthritis can manifest itself with other, additional symptoms, such as:
- burning sensation in the eyes;
- inflammation of the salivary glands with insufficient saliva production;
- chest pain that occurs when breathing;
- numbness or increased sweating of the hands and feet;
- the appearance of pain when sitting for long periods of time;
- chronic fatigue;
- frequent signs of ARVI;
- the occurrence of frequent outbreaks of morbidity;
- muscle pain;
- prolonged depression.
Articular signs
The leading clinical manifestation of rheumatoid arthritis is articular syndrome. Bilateral lesions of the joints are most often diagnosed. The patient complains of periodic pain in the x
joints, fatigue, morning stiffness, usually disappearing within an hour. A psychopathological disorder gradually develops, expressed in fatigue, weakness, and drowsiness. Sweating increases, body temperature rises to subfebrile values (within 37.1-38.0°C). Typically, rheumatoid arthritis debuts with the change of seasons, after entering a certain physiological period (menopause, puberty, postpartum). Provoking factors include trauma, hypothermia, respiratory, gastrointestinal, and urogenital infections.
If the pathology debuts acutely or subacutely, then the clinical picture is complemented by a febrile state, severe myalgia and arthralgia. With the slow progression of rheumatoid arthritis, the intensity of the symptoms almost does not change, as does the functional activity of the joints, which are gradually involved in the pathological process:
- first, the joints of the hands, feet, and wrists (usually the wrist joints) are affected;
- then the inflammatory process affects the shoulder, elbow joints, and ankles;
- at the last stage, tissue destruction is observed in the hip and knee joints.
Damage to the temporomandibular joints is less common. Pathological exudate accumulates inside the joints, they swell and are painful on palpation. Movement is limited, the skin turns red and becomes hot to the touch due to overfilling of blood vessels. Inflammation of the tendon sheaths provokes the development of tunnel syndrome as a result of compression of the median nerve. In this case, sensitivity and mobility of the fingers decrease, and the resulting pain radiates even to the forearms. The pathology can occur as Steele's disease, accompanied by osteoarthritis, Felty's syndrome, or polyarthritis.
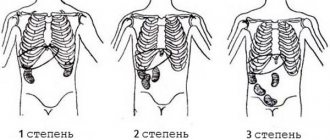
Rheumatoid arthritis has three stages
- the first is manifested by swelling of the synovial bursae of the joints, pain, redness of the joints
- the second stage is characterized by active cell division, causing thickening of the joint lining
- the third is manifested by joint deformities, increased pain, decrease or loss of motor functions in the joints.
There are different options for the clinical course of rheumatoid arthritis, among which are:
- classic version of the flow;
- mono- or oligoarthritis (which affects large joints);
- arthritis with pseudoseptic syndrome (manifested by fever, weight loss, anemia, vasculitis);
- Felty's syndrome (polyarthritis is present, the disease is accompanied by an enlarged spleen);
- Still's syndrome;
- juvenile forms of arthritis (manifested by allergic reactions, joint damage and symptoms of damage to internal organs);
- visceral-articular forms (severe damage to joints and internal organs).
Extra-articular manifestations
Systemic signs are more pronounced in the seropositive (presence of rheumatoid factor in the blood) form of the pathology. Skeletal muscles are always involved in the inflammatory process - interosseous, forearm extensors, rectus femoris and gluteal muscles. Severe atrophy is observed, muscle strength and tone decrease. The skin becomes dry, the epidermis becomes thinner, and hemorrhages into the soft tissue and subcutaneous tissue become more frequent. Gangrene of the distal phalanges occurs as a result of the formation of small necrotic foci in the subungual area.
A specific extra-articular manifestation of the disease is the formation of subcutaneous connective tissue nodules measuring 5-20 mm. They are dense, round, mobile, multiple or single, painless on palpation. The location of the nodules is symmetrical or asymmetrical on the forearms and in the occipital region. Formations are often found in the myocardium, lungs, and heart valves. The formation of nodules indicates a rheumatic attack, and their resorption indicates the achievement of a stable remission. Rheumatoid arthritis is characterized by extremely severe damage to internal organs:
- lymphadenopathy (enlarged lymph nodes);
- gastrointestinal pathologies - enteritis, colitis, amyloidosis of the rectal mucosa;
- neuropathies, polyneuritis, diffuse fibrosis, pneumonitis, alveolitis, bronchiolitis;
- glomerulonephritis, amyloidosis.
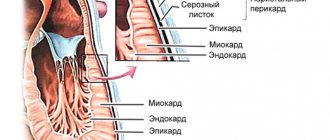
Involvement of the main blood vessels causes the development of myocarditis, granulomatous aortitis, pericarditis, endocarditis, and coronary arteritis. In rheumatoid arthritis, vasculitis and visceropathy are not uncommon. Clinically, they are manifested by a polymorphic rash, ulcerations, nasal and uterine bleeding, and thrombotic syndrome.
How does an exacerbation manifest itself?
Rheumatoid arthritis has two phases. Remission is a period of relative well-being when the symptoms of the disease become less pronounced or disappear completely. On the contrary, during an exacerbation, not only signs of joint inflammation appear, but also general reactions.
Exacerbation of rheumatoid arthritis is manifested by the following symptoms:
- Severe pain in the affected joints. It becomes constant and does not depend on the time of day. NSAIDs most often do not have any effect;
- Increasing the temperature to 37-38.5°C
- Severe weakness and apathy;
- Loss of appetite;
- Chest pain, difficulty breathing, discomfort in the eye area, and decreased vision may occur.
It is important to recognize an exacerbation of arthritis as early as possible, since during this period all the patient’s organs suffer. Special treatment is required to relieve all symptoms and return the disease to remission.
Diagnostics
Making a diagnosis of rheumatoid arthritis is quite difficult, since the symptoms of various joint diseases can be similar to each other. To confirm or refute the presence of this disease, laboratory and instrumental diagnostic methods are used.
Laboratory diagnostics
Clinical blood test
Rheumatoid arthritis is a disease of the entire body, not just a few joints. Therefore, signs of an inflammatory process can be found in the blood:
- A large number of immune cells (leukocytes) – more than 9*109/l;
- Acceleration of ESR – above 15 mm/sec;
- An increase in eosinophils in the blood - more than 7% of the number of leukocytes.
In some cases, there may be a decrease in the number of red blood cells (less than 3.7*1012/l in women; less than 4.5*1012/l in men) and hemoglobin (less than 120 g/l). These signs often indicate severe arthritis or an exacerbation of the disease.
Biochemical analysis of venous blood can also indicate the presence of arthritis. The amount of C-reactive protein (abbreviated as CRP) increases significantly with this disease, rising above 10-15 mg/l.
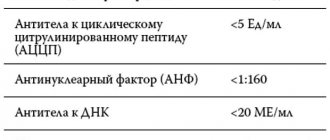
Rheumatoid factor test
The most specific method of laboratory diagnostics. It allows you to assess not just the presence of inflammation, but also confirm its autoimmune nature (when the patient’s antibodies attack his own cells). Normally, rheumatoid factor is not found in the blood, or its minimal concentrations are detected (up to 10 U/l). With arthritis, this figure increases several times.
Instrumental diagnostics
X-ray
To this day, the method has not lost its significance. This is a cheap and fairly accurate way to diagnose rheumatoid arthritis. Changes in the image can be seen within 1-3 months after the onset of the disease. The earliest radiological symptom is osteoporosis (decreased calcium concentration) of the bones that form the joint.
As arthritis progresses, new signs of the disease appear on the x-ray:
- Erosion on parts of the bones that face the joint cavity;
- Destruction of these bone sections;
- “Overgrowth” of the affected joints, which leads to limitation of their mobility.
It is important to carry out repeated x-rays at different stages of treatment, which will allow one to assess the dynamic condition of the joints and the adequacy of the therapy.
Densitometry
This is a way to study bone density. Currently, densitometry is carried out using ultrasound, which makes the method completely safe and quite accurate. The study helps to identify the initial signs of rheumatoid arthritis, at the stage of development of osteoporosis.
Other tests such as arthroscopy, biopsy and scintigraphy are rarely used to diagnose rheumatoid arthritis. They allow you to determine the presence of damage in the joint, but such specific signs as with radiography cannot be detected.
Where do the roots come from?
It is believed that the first signs of rheumatoid arthritis may appear in those who have a weak immune system, as well as in survivors of various injuries. Infection in the body also poses a serious risk to joint health.
Arthritis is a joint pathology that is provoked by the production of autoimmune bodies that quickly divide in healthy tissues. Arthritis is often provoked by hepatitis and angina. Negative changes in joints characteristic of the disease are, in some cases, irreversible.
Drug treatment
Rheumatoid arthritis is difficult to treat and is often almost impossible to cure. The disease lasts throughout life, accompanied by periodic exacerbations, which are followed by periods of remission. Treatment of the disease is based on pain relief, inhibition of disease progression and restoration of joint function through surgery. The earlier a disease is detected, the greater the chance of reducing the harm it causes.
To treat rheumatoid arthritis, 4 main groups of medications are needed:
NSAIDs
NSAIDs (diclofenac, ibuprofen, nimesil, movalis, indomethacin, list of non-steroidal anti-inflammatory drugs) have an anti-inflammatory effect; these drugs inhibit the activity of the enzyme that causes the destruction of articular cartilage, reduce signs of inflammation and reduce joint pain. NSAIDs must be prescribed with caution; with long-term use and the combined use of several drugs in this group, the risk of side effects increases significantly.
Basic drugs
Basic drugs for the treatment of rheumatoid arthritis (sulfasalazine, methotrexate, aminoquinoline drugs, leflunomide, azathioprine, cyclophosphamide, cyclosporine, Remicade, timodipressin, etc.) in combination with hormones help reduce the activity of rheumatoid arthritis. Treatment with basic drugs is prescribed for a period of no more than 6 months. In total, there are five groups of basic drugs for the treatment of rheumatoid arthritis: gold drugs, cytostatics, antimalarial drugs, sulfonamides and D-penicillamine.
GCS (corticosteroids)
Glucocorticosteroids (hormonal drugs) (prednisolone, dexamethasone, methylprednisolone, triamcinolol) are prescribed both in the presence of systemic manifestations of the disease and in their absence. Today, in the treatment of rheumatoid arthritis, treatment is practiced with both small and large doses of hormones (pulse therapy). Corticosteroids are excellent for pain relief.
Biological agents
Biological drugs (halofuginone, etanercept, Humira, Actemra, rituximab, Orencia) have a protein base and are developed through genetic engineering. Their main purpose is also to suppress inflammation due to their effect on special components of the human immune system.
Modern drugs for the treatment of arthritis
The latest generation of drugs against rheumatoid arthritis are drugs that selectively reduce the activity of inflammatory substances in the body: interleukins, tumor necrosis factor (TNF) and others. They have proven their effectiveness not only in pharmacological trials, but also in real clinical practice. Another advantage is the rare occurrence of adverse reactions.
The main representatives of this group of drugs:
- Infliximab (synonyms: Remicade, Flammegis);
- Etanercept (synonym: Enbrel);
- Adalimumab.
Why are these drugs not widely used? It's a matter of price. The cost of 20 ml of the drug, on average, is 45,000-50,000 thousand rubles. Not every hospital or patient can afford this.
Physiotherapy
The severity of the inflammatory process in rheumatoid arthritis can be controlled not only with medications. For this purpose, physiotherapy is used, which, in addition to the anti-inflammatory effect, stimulates blood circulation in the affected joints. Good blood flow contributes to the gradual restoration of cartilage and normalization of the production of intra-articular fluid (synovium).
The following methods are highly effective:
- Electrical stimulation according to Gerasimov is a new method of physiotherapy, the principle of which is to stimulate the tissues around the joint with low-frequency current. The course of treatment is 3-6 procedures, and the effect lasts for several years. After therapy, patients note a decrease in the severity of pain, stiffness and signs of inflammation (swelling and redness of the joints);
- Galvanic currents;
- Irradiation of the joint with ultraviolet waves;
- Diathermy is the application of low-frequency current to the joint area in order to warm it up.
In addition to classical physiotherapy, traditional methods of treatment can be used to treat rheumatoid arthritis: warm compresses, trips to the bathhouse with “steaming” the joint area, poultices.
It should be noted that physiotherapy does not replace drug treatment, but only complements it. Otherwise, rheumatoid arthritis will steadily progress and lead to damage and curvature of the joints.
Lifestyle change
In the treatment of rheumatoid arthritis, lifestyle correction is of great importance. It is necessary to find a balance between the load on the joints and their rest. Let's explain with an example.
If the patient works in production and is forced to carry heavy objects every day or are in the same position (welders, assemblers and other professions), excessive stress will be placed on the joints, which contributes to their destruction.
The opposite situation is that a patient with rheumatoid arthritis works as an office worker who does not exercise. His joints receive virtually no stress, which is why little blood flows to them, fewer anti-inflammatory substances are produced, and they are more quickly damaged by the disease.
How to make lifestyle changes with rheumatoid arthritis
- Lose weight – if your mass index (calculated as weight/height2) is greater than 25, you should take steps to reduce weight. Most often, a diet limiting fatty, fried, starchy foods, fast food, and physical exercise is sufficient;
- Avoid static loads - when a person stays in one position for a long time or holds an object, the load on the joints increases several times. This leads to progression of the disease. To reduce the impact on your joints, it is recommended to take “dynamic breaks” regularly. Within 3-5 minutes, change your position several times and perform a few simple movements to warm up your joints;
- Exercise – moderate stress on the joints helps normalize blood flow and has a slight anti-inflammatory effect. You should not strive for athletic achievements, as this can lead to negative consequences. Swimming is the best option for physical exercise for patients with rheumatoid arthritis;
- Follow the doctor's recommendations - therapy for rheumatoid arthritis is always accompanied by taking potent medications that have side effects. However, they should not be canceled without the doctor’s permission. This will lead to the progression of the disease and the rapid development of deformities.
What else can I use?
Traditional medicine knows quite a few recipes recommended for arthritis. For example, you can treat yourself with chestnuts. When the tree blooms, collect the flowers and fill them with vodka: 300 g of inflorescences account for 200 ml of alcoholic beverage. Instead of vodka, you can take alcohol pre-diluted with clean water. The tincture is placed in a dark place for 2 weeks, after which for 10 days in a row, drink a tablespoon three times a day before meals.
Another recipe involves using bay leaves. 30 g of dry leaves are thoroughly crushed, poured with half a liter of boiled water and allowed to brew for half a day. The drink is drunk before meals every day for ten days in a row. Dose – 100 ml.
Sabelnik helps eliminate the signs of rheumatoid arthritis. The plant is dried, crushed, and filled with vodka per liter per 200 g of herb. As an alternative, you can use homemade moonshine. The mixture is infused for 3 weeks, filtered, and used in food, one tablespoon at a time before meals. The duration of the course is two weeks. Instead of cinquefoil, you can take elderberry, birch buds or willow bark.
Surgery
Currently, the help of surgeons in the treatment of rheumatoid arthritis is resorted to only in cases of severe joint deformities. Most often, the following options are observed:
- “Walrus fin” - the entire hand deviates towards the body and cannot return to its normal position;
- Boutonniere fingers – strong flexion of the fingers in the initial sections and normal position of the final phalanges;
- “Swan neck” - the fingers on the hand are curved in a wave-like manner;
- “Spindle” finger – white thickenings (rheumatoid nodules) are noted in the area of the knuckles of the finger.
In addition to the hand, the joints of the foot and knee may also be affected. If they are so altered that the patient cannot take care of himself normally, he is offered prompt correction of the defect. Surgeons can replace the entire joint, reconstruct the affected part, or realign the bones without the use of foreign bodies.
Diagnostic tests
Knowing the characteristics of the disease and anticipating possible complications of rheumatoid arthritis, you should immediately consult a rheumatologist for advice. To determine the correct diagnosis, you should donate blood for biochemical and immunological tests.
To check the extent of joint destruction, fluoroscopic examination, magnetic resonance imaging or arthroscopy is required.
In case of existing complications of rheumatoid arthritis, you should contact a specialized specialist. Let's look at the consequences of the disease.
How to treat an exacerbation
The most dangerous phase of rheumatoid arthritis is an exacerbation. At this time, the symptoms of the disease manifest themselves most strongly (pain, fever, swelling and redness of the joints, etc.), and the joints are damaged much more intensely than during remission.
During an exacerbation, doctors use a special treatment regimen that can quickly stop rheumatic inflammation:
- Pulse therapy. The principle of the method is to prescribe high doses of glucocorticosteroid hormones (Prednisolone, Hydrocortisone, Methylprednisolone) for 3 days. A short period of therapy does not allow the development of pronounced adverse reactions, and a large amount of the drug, most often, allows to relieve most of the symptoms of the disease;
- Correction of basic therapy - doctors must figure out why the patient experienced an exacerbation while taking medications. If necessary, the patient changes the dose of cytostatics or their regimen;
- NSAIDs – These are used as a supplement to hormones. As a rule, Diclofenac or Ibuprofen are used.
The doctor must inform the patient about the prognosis, course and nature of his disease, the treatment monitoring scheme, the duration and complexity of therapy, as well as unwanted side effects of drugs and their combination with other drugs. Also that during treatment, exacerbation of chronic infections is possible, and immunosuppressive drugs should be temporarily discontinued. Treatment of rheumatoid arthritis is prescribed by an experienced rheumatologist and periodic monitoring of both disease activity and response to treatment is assessed.
Features of drugs
Of all the drugs that show greater or lesser effectiveness in arthritis, Methotrexate is the most widely used. The drug is cytostatic, pharmacological, prevents the destruction of healthy cells, fights malignant ones. For arthritis, the use of this remedy is the standard treatment.
It is unacceptable to self-prescribe medications against joint diseases. The dose, course duration, and specific drug are selected by a qualified doctor, taking into account the individual characteristics of the patient’s body. Methotrexate has contraindications and is not used in the presence of infectious diseases in chronic, acute forms, ulcers, or pregnancy. It should not be used if the immune system is weak and the kidneys and liver are insufficient.