Pulmonary sclerosis is a disease in which lung tissue is replaced by connective tissue. Pulmonologists at the Yusupov Hospital, based on a comprehensive examination, identify the cause of sclerosis of the lung tissue and carry out effective therapy for the disease that caused it.
Pulmonary sclerosis can be local or diffuse. Pathological changes often form in the following diseases or accompany them:
- chronic obstructive pulmonary diseases;
- infectious, viral and fungal diseases of the lungs;
- pneumoconiosis;
- genetically determined lung diseases;
- injuries and consequences of penetrating chest wounds.
If their treatment is ineffective, prerequisites for the development of sclerosis arise in the lung tissue. Among the provoking factors of the disease, heart failure, pulmonary thrombosis, the influence of ionizing radiation, and dysfunction of the immune system should be noted.
With incomplete resolution of the inflammatory process in the lungs, connective tissue grows, which leads to pneumosclerosis. Similar changes in lung tissue are observed after pulmonary tuberculosis. Diffuse sclerosis develops in patients suffering from Hamman-Rich syndrome. In this case, the lung resembles a honeycomb. With mitral valve stenosis and cardiac left ventricular failure, fluid leaks from the blood vessels, which leads to cardiogenic pulmonary sclerosis.
General information
Pulmonary pneumosclerosis is a condition characterized by the proliferation of connective tissue in the lungs, leading to the gradual replacement of pulmonary connective tissue.
Accompanied by impaired lung function caused by changes in the elasticity of the lung tissue and gas exchange in areas with pathological changes. Replacement and pronounced proliferation of connective tissue leads to compaction of the lung tissue and causes deformation of the bronchial tree. In fact, pneumosclerosis is the outcome of a number of diseases of both the bronchopulmonary system and diseases of other organs and systems. It should be noted that pneumosclerosis is a constantly developing process of restructuring of the lung tissue, in which lesions of the interstitium, alveoli and perialveolar tissue, and pulmonary capillaries gradually increase. Such pathological changes contribute to excessive fibrosis formation and gradually destroy/deform lung tissue, forming pulmonary pneumosclerosis. Some authors believe that there is a genetic predisposition in individuals to the development of diffuse lung diseases, developing as a response to nonspecific damage to the lung epithelium.
The course of the disease, the severity of clinical manifestations and its prognosis are determined by the degree of impairment of respiratory function and gas exchange, which in turn is determined by the prevalence of the pathological process. Changes in the lungs at the level of local lesions occur predominantly without respiratory distress and asymptomatically, and a diffuse process affecting a significant part of the lung tissue is accompanied by impaired ventilation in the lungs of an obstructive/restrictive type with the development of hypertension in the pulmonary circulation or its absence and is manifested by rapid fatigue, chest pain, progressive shortness of breath and cough.
A diffuse process in the lungs, as a rule, leads to a number of disabling complications and a significant deterioration in the patient’s quality of life, and in severe cases, it reduces life expectancy. In the structure of pneumosclerosis, focal and diffuse forms occur in approximately equal proportions. Sometimes patients ask whether pneumosclerosis is contagious or not? The disease itself is not contagious, but some diseases that underlie its development can be contagious, for example, tuberculosis .
Pathogenesis
The pathogenesis of pneumosclerosis depends on its etiology. However, regardless of the etiological forms, the leading pathogenetic mechanisms of the disease are: impaired ventilation of the lungs, decreased drainage function of the bronchi, and blood/lymph circulation disorders. The process of proliferation of connective tissue is directly caused by a violation of the structure and destruction of the morphofunctional elements of the lung parenchyma.
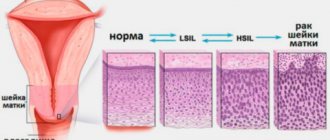
Inflammation is of greatest importance in the development of the disease. The histogenesis of pneumosclerosis of inflammatory origin is based on edema, inflammatory infiltration , carnification , development of granulation tissue, sclerosis of the walls of bronchioles with subsequent fibrosis of foci of interstitial inflammation of the interalveolar septa, promoting the development of a honeycomb lung with the destruction of the interalveolar septa and the formation of multiple cavities.
Under conditions of infectious inflammation, increased production of elastase , which causes destruction of the connective tissue matrix and alveolar walls with the formation of common cavities. fibroblasts are activated , which contributes to the increased development of connective tissue in the lung parenchyma and the formation of fibrosis.
Classification
Based on etiology, they are distinguished:
- Infectious specific (mycotic, tuberculous, parasitic, syphilitic) and nonspecific (post-traumatic, post-aspiration).
- Toxic (reaction to exposure to toxic substances).
- Pneumoconiotic (occupational pathology).
- Dysplastic (developing as a result of congenital enzymopathies or malformations of the lung).
- Dystrophic (due to ossification, radiation pneumonitis, amyloidosis ).
- Allergic (exogenous - from inhalation of fungal spores, medicinal) and endogenous (for collagen diseases, Hamman-Rich syndrome, for idiopathic pulmonary hemosiderosis , for allergic granulomatosis).
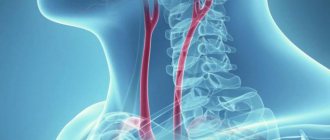
- Cardiovascular (for congenital/acquired heart defects, accompanied by hypertension of the pulmonary circulation, embolism/thrombosis of the pulmonary circulation).
According to pathomorphological characteristics:
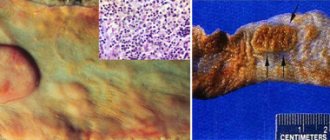
- Local (limited) small- and large-focal - characterized by the formation of individual foci of sclerosis . Macroscopically it represents a limited area of compacted pulmonary parenchyma with a reduced lung volume in this part. The local focus of pneumosclerosis does not have a significant effect on the elasticity/gas exchange function of the lungs.
- Diffuse pneumosclerosis. What it is? This form of the disease is characterized by extensive perivascular/peribronchial growths of connective tissue in the form of a mesh with large cells (reticular pneumosclerosis) or diffuse sclerosis of predominantly interalveolar septa (interstitial pneumosclerosis). The diffuse process is characterized by a picture of a rigid lung with reduced ventilation.
Pathogenetically, inflammatory , atelectatic , lymphogenic and immune pneumosclerosis .
Depending on the prevalence of the affected structural elements of the lungs alveolar , interstitial , perivascular , perilobular and peribronchial in the mediastinal zone are distinguished ( hilar pneumosclerosis ). Based on the affected segments, hilar pneumosclerosis of the lungs is distinguished, this is when the pathological process is concentrated in the hilar areas of the lung and basal pneumosclerosis, when any basal segment of the lungs is involved in the pathological process (anterior, medial, lateral and posterior basal segments).
Causes
Pneumosclerosis can be the outcome of a number of inflammatory/destructive lung diseases (chronic pneumonia, abscesses, pleurisy ), specific diseases ( tuberculosis ), fibrosing alveolitis, occupational diseases ( pneumoconiosis ), radiation injury, traumatic damage to lung tissue, etc.
Lung diseases:
- Pneumonia . Among infectious lung diseases, the leading role belongs to chronic pneumonia of various origins (bacterial, mycotic, tuberculous etiology, Legionnaires' disease, cytomegalovirus infection, chlamydial pneumonia), which are often complicated by pleural empyema , lung abscess , resolving with the formation of pneumosclerosis.
- Chronic obstructive pulmonary disease, including bronchial asthma , in which the inflammatory process is accompanied by a pronounced change in the structure of the bronchial wall with the development of pneumosclerosis.
- Dust occupational lung diseases ( pneumoconiosis ). Caused by prolonged inhalation of various types of aggressive dust: silicon/coal dust ( silicosis ); cement, asbestos, talc, kaolin dust ( silicates ); dust of aluminum, beryllium, iron ( metalloconiosis ), etc. Occurs in the initial stages of the disease as chronic bronchiolitis/progressive alveolitis, turning into pneumosclerosis .
- The pulmonary form of sarcoidosis is accompanied by gross disturbances in the structure of the lungs, the formation of bronchiectasis and bronchial stenosis with the gradual development of widespread pneumosclerosis with severe respiratory failure.
- Allergic lung diseases (allergic exogenous alveolitis , hypersensitive pneumonitis ). Diseases of an immunopathological nature that develop when inhaling an antigen, often organic dust or vapors - heavy metal salts, polyurethane, dyes, fungicides.
- Idiopathic fibrosing alveolitis . It is characterized by a progressive disruption of the structure of the pulmonary structures, diffuse thickening of the interalveolar septa, and the formation of cystic cavities leading to the development of diffuse pneumosclerosis .
- Lung operations, the complication of which is excessive diffuse sclerosis of the interalveolar septa.
Diseases of other systems and organs:
- Active chronic hepatitis .
- Systemic autoimmune diseases: systemic lupus erythematosus , scleroderma , ankylosing spondylitis , rheumatoid arthritis . Systemic diseases are, in principle, characterized by fibrotic changes due to an increase in the function of fibroblasts in the tissues of various organs, including the lungs.
- Diseases of the heart and blood vessels (congenital/acquired heart defects, accompanied by pulmonary hypertension) - they are characterized by diffuse pneumosclerosis of cardiovascular origin.
Common reasons:
- Radiation therapy , one of the complications of which is post-radiation pulmonary pneumosclerosis. It develops more often in breast cancer/lymphogranulomatosis after irradiation of the mediastinal area. The frequency of complications is determined by the total focal dose. Persons aged 65-70 years have complications 1.5 times more often than patients aged 40-60 years.
- Toxic damage (inhalation of toxic substances). Toxic diffuse pneumosclerosis often develops when exposed to toxic warfare gases, oxygen and ozone in high concentrations, smog, industrial pollutants, and prolonged inhalation of cigarette smoke. At the same time, not only the inhalation of toxic substances matters, but also their exposure and individual sensitivity to them.
- Taking medications: Methysergide , Methotrexate , Proctolol , Amiodarone , Propranolol . Pneumosclerosis can develop as a long-term complication.
Prevention
To prevent the development of pneumosclerosis, it is recommended:
- timely treatment of diseases that can lead to pneumosclerosis;
- giving up bad habits (including avoiding passive smoking);
- annual preventive fluorography;
- refusal of irrational use of medicines;
- increasing immunity: rational nutrition, sufficient physical activity, proper rest;
- avoiding lung injuries.
Video from YouTube on the topic of the article:
Symptoms of pneumosclerosis
Pneumosclerosis has no characteristic clinical signs. More often in the clinic, the symptoms of diseases that caused the development of the disease ( chronic pneumonia , bronchiectasis , tuberculosis , etc.) come to the fore. With focal damage to the lungs, symptoms are mild or may be absent altogether. The main manifestation of diffuse forms of the disease is a violation of the ventilation function of the lungs, which can manifest itself in an obstructive or restrictive type, which is manifested first by shortness of breath during exercise, and later at rest and cyanosis. General symptoms of pulmonary sclerosis are manifested mainly by fatigue, weakness, dry cough, low-grade fever, and weight loss. Auscultation at the height of inspiration reveals crepitus in the posterior lower regions.
When large fibrous nodes form against the background of pleurisy, there may be complaints of chest pain and tingling between the shoulder blades. In chronic bronchitis - cough with sputum. Subsequently, as pneumosclerosis progresses, the phenomena of pulmonary hypertension , hypoxia , respiratory and right ventricular heart failure increase.
Medicines
Photo: proizjogu.ru
Medicines are not able to relieve the patient of pneumosclerosis; they only alleviate the symptoms of the disease. Cough with pneumosclerosis is unproductive; to correct this, expectorants and mucolytics are prescribed. Ambroxol is the most common drug due to its low cost and sufficient effectiveness. The drug achieves its effect by stimulating the glands of the bronchial mucosa. This increases the content of the mucous component of sputum, which facilitates its release. The drug is well tolerated, side effects are extremely rare. For example, in case of individual intolerance to the components of the drug, an allergic reaction develops, which can manifest itself as urticaria or angioedema. Other side effects observed less frequently are: nausea, vomiting, diarrhea, abdominal pain, headaches, general weakness.
Bromhexine is another drug that is used to thin phlegm. Not for use in children under 3 years of age and pregnant women (1st trimester). In all other cases, there are no strict contraindications to the use of the drug. People who have an allergic reaction to the active substance, bromhexine hydrochloride, should be treated with caution. Such people should notify their doctor in advance about the presence of an allergy to a previous drug intake, so that the doctor can select another drug with the desired effect.
Tests and diagnostics
The main diagnostic methods are radiography, fluorography and computed tomography of the lungs.
In pneumosclerosis, the X-ray data of the lungs are variable and reflect changes in the lungs characteristic of the underlying disease, against the background of which, in addition, signs of diffuse pneumosclerosis are determined: fine mesh deformation of the pulmonary pattern, a decrease in the size of the lung, emphysema, less often - changes in the “honeycomb lung” type.
High-resolution computed tomography allows you to more clearly determine the nature, severity, extent and dynamics of changes.
If necessary, a pulmonary function test and transbronchial cryobiopsy are performed.
Lifespan
The more effective the treatment for pneumosclerosis, the higher the life expectancy. Life expectancy is also influenced by the patient’s condition and his attentive attitude to his health. It is an unhealthy lifestyle and decreased immunity that leads to a decrease in quality of life.
It is important to follow not only preventive methods, but also comprehensive treatment. It is imperative that you do not use medications uncontrollably. Since this not only leads to diseases, but worsens the course of the underlying pathology.
Life expectancy is higher if the patient follows the doctor’s instructions. Under no circumstances should you treat yourself. This not only shortens life expectancy, but also leads to irreversible complications!
Forecast
The prognosis of diffuse pneumosclerosis is determined by the course of the underlying disease and the rate of progression of sclerotic changes in the lung tissues. An unfavorable prognostic sign is the formation of a “honeycomb lung”, pulmonary heart and the addition of a secondary infection. It is impossible to say exactly whether life expectancy changes with pulmonary pneumosclerosis or not, since everything is individual. With the local form of the disease, patients live their usual lives without any restrictions, while significant deterioration in the patient’s quality of life accompanies diffuse pneumosclerosis . It is also difficult to answer how many people live with this. Some patients live to a ripe old age, others live with disabling complications, and some patients die due to bacterial infection , tuberculosis , or pneumomycosis .
Treatment
Photo: sanatoriy-kirova.ru
To prevent the development of pneumosclerosis, you should promptly treat respiratory diseases, take precautions when interacting with pneumotoxic substances, and do not delay going to the doctor if characteristic symptoms occur. When working in hazardous industries, it is important to use respirators that prevent dust and chemicals from entering the respiratory tract. In addition, the immediate production management must take care of the proper operation of exhaust ventilation.
When diagnosing pneumosclerosis, treatment begins with lifestyle changes. First of all, it is recommended to stop smoking, as cigarettes can aggravate bronchial obstruction. All family members must understand that there is a concept of passive smoking, so it is important not only for the patient himself to forget about cigarettes, but also for the people living in the same living area. Meals should be fractional, complete, sufficiently filled with vitamins and microelements. Despite the fact that pneumosclerosis is accompanied by shortness of breath, especially when playing sports, you should not completely give up physical exercise. It is necessary to arrange long distance walks and perform therapeutic exercises.
Considering that with pneumosclerosis, the lungs cannot fully provide the body with the necessary amount of oxygen, oxygen therapy is used. This treatment helps saturate the blood plasma with oxygen, which leads to a decrease in the severity of shortness of breath. However, safety rules should be observed, since frequent or excessive use of pure oxygen or inhalation mixtures with high oxygen concentrations can lead to oxygen intoxication.
For the symptomatic treatment of cough, expectorants are used to promote the separation of sputum. For the same purpose, mucolytic agents are prescribed, which dilute sputum, thereby facilitating its removal.
List of sources
- Kogan E.A., Korenev B.M., Popova E.N. and others / ed. ON THE. Mukhina. Interstitial lung diseases. Practical guide. - M.: Litterra, 2007. - 432 p.
- Shmelev E.I. Differential diagnosis of interstitial lung diseases // Handbook of a practical physician. - 2005; 5:6: 3-16.
- Aisanov Z.R., Kokosov A.N., Ovcharenko S.I., Khmelkova N.G., Tsoi A.N., Chuchalin A.G., Shmelev E.I. Chronic lung diseases. Federal program. RMJ, 2001; No. 1: p. 9 – 33.
- Ivanova A. S. Fibrosing processes / A. S. Ivanova, E. A. Yuryeva, V. V. Dlin. M.: Overlay, 2008. 196 p.
- Avdeeva O.E., Avdeev S.N. Idiopathic fibrosing alveolitis: modern approaches to diagnosis and therapy // Consilium medicum. 2002; 4 (4): 195-201.