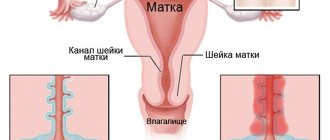
Cervical dysplasia is pathological changes in the epithelial layer of the cervix, which can lead to the formation of a malignant tumor. Analogue names: cervical intraepithelial neoplasm, cervical intraepithelial neoplasia - abbreviated CIN or CIN.
Dysplasia is a reversible transformation of cervical tissue into an abnormal state. The transition occurs gradually and unnoticed by the woman - this is the main danger of the pathology.
The epithelial layer of the cervical mucosa is a sequence of basal, intermediate and superficial layers. In the basal one, cell division occurs, in the intermediate one they mature, and the superficial one performs a barrier function. With dysplasia, atypical cells appear among normal cells: multinucleated, irregular in shape, size and abnormally located in relation to the basement membrane. As a result, thickening (hyperplasia) and cell proliferation (proliferation) develop in the epithelial layers. Because of this, normal cell renewal, maturation, aging and cell rejection are impossible. Up to a certain point, dysplasia is not dangerous. However, if neglected, it can lead to serious problems - the development of a cancerous tumor. Therefore, timely diagnosis and treatment of dysplasia prevents the development of cancer in the cervix.
Types of cervical dysplasia
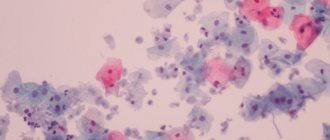
After a cervical biopsy, a specialist will examine the histological structure of the material taken under a microscope. If pathology is present, abnormal epithelial cells with many small nucleoli or an excessively large shapeless nucleus with unclear boundaries will be detected. Next, it is necessary to determine the depth of the lesion and the condition of the cells in the corresponding layers.
Stages (severity) of cervical dysplasia indicate the depth of distribution of altered cells in the cervix. The calculation to determine the thickness of the lesion in the epithelial layer of the organ is carried out from the basement membrane:
- Stage I - the anomaly extends to 1/3 of the thickness of the epithelial layer. Only 10% of patients with the development of dysplasia at the first stage are predisposed to the transition of the pathology to moderate or severe dysplasia in the next 2-4 years. In most cases (90%), grade 1 neoplasia goes away on its own;
- Stage II - spread of atypical cells over 2/3 of the thickness. Precancerous condition. At this stage, active treatment is necessary; wait-and-see tactics are inappropriate: there is a high risk of pathology developing into severe dysplasia and cervical cancer;
- Stage III - more than 2/3. Doctors use the term carcinoma in situ, CIS (carcinoma in situ) or “carcinoma in situ,” a non-invasive cancer. This is the name of a malignant tumor in the first stages of development, which is characterized by an accumulation of histologically altered cells without germination into the underlying tissue.
The mild stage quite rarely turns into a moderate or severe stage: this is facilitated by an unhealthy lifestyle, weak immunity and lack of periodic examinations by a gynecologist. Time of transition to cancer in the deep tissues of the cervix:
- with a mild form and predisposition - approximately 5 years;
- with moderate form - 3 years;
- in case of severe dysplasia - 1 year.
Stages
As already mentioned, in the vaginal part of the cervix, a boundary is formed between squamous columnar epithelium, rich in glands, and stratified epithelium. With dysplasia, round mononuclear cells turn into shapeless multinucleated epithelial cells. In addition, the layer-by-layer structure of tissues is disrupted. Doctors classify the stages of dysplasia depending on the depth of cellular deformation.
Degrees of pathology:
- The first stage (mild dysplasia), characterized by changes in the lower parts of the stratified epithelium. The morphology of the cells is practically unchanged.
- Second stage. Dysplasia gradually spreads in the middle part of the stratified epithelium.
- The third stage, which is also called early stage carcinoma (severe dysplasia). In this case, changes affect all layers of squamous epithelium. In this case, malignant cells do not spread to muscles, blood vessels and connective tissues, so we are talking about non-invasive cancer.
Determining the stage of cellular changes during diagnosis is very important for selecting effective treatment.
Causes of cervical dysplasia
The main reason for the formation of atypical cells in the cervix is oncogenic strains of the human papillomavirus (HPV16 and HPV18). The test for the detection of this virus is positive in 95-98% of cases of cervical dysplasia. Therefore, HPV is considered to be a trigger in the formation and development of the disease.
Papillomavirus is a sexually transmitted infectious disease that affects the skin. Its most common manifestations are papillomas and warts.
When diagnosing even a mild form of neoplasia, the doctor pays attention to the following factors:
- duration of existence of the virus in the body (more than a year - the basis for starting treatment);
- the general condition of the patient’s body and health;
- a woman’s lifestyle, the presence of bad habits and characteristics of sexual life.
Causes of dysplasia:
- endogenous (internal) - pathology is caused by hormonal disorders and/or reduced immunity;
- exogenous (external) - these include HPV, other viruses and infections.
At risk:
- women whose close relatives had cancer;
- patients who have been taking oral contraceptives for a long time - this leads to changes in hormonal levels;
- patients with chronic infectious and inflammatory processes in the organs of the reproductive system;
- women who began sexual activity early;
- women who have undergone many births or abortions (the cervix is subjected to repeated trauma).
A state of immunodeficiency can lead to the development of cervical dysplasia and its transformation into a cancerous tumor. Therefore, the doctor needs to know about the frequency of inflammatory processes in the human body and the presence of chronic diseases. You also need to tell your doctor about your diet, stress, and treatment with drugs that reduce immunity.
For a long time it was believed that dysplasia is a “disease of the young”, and that girls aged 20-30 are susceptible to it. However, modern data show that cell transformation in the cervical epithelium can begin at any age, including after 70 years.
Symptoms
Dysplasia cannot be diagnosed by specific symptoms or signs except in rare cases (see below). Pathology can only be identified based on the results of an examination by a doctor and tests.
But you should seek additional examination from a specialist if:
- atypical vaginal discharge;
- intermenstrual bleeding or blood after sexual intercourse;
- pain in the lower abdomen.
Only the third degree of neoplasia has pronounced but not obvious symptoms:
- pain during and after sexual intercourse;
- itching, burning and irritation on the external genitalia;
- vaginal discharge is profuse and has a strong odor;
- periodic pressing or aching pain in the lower abdomen.
Signs of cervical dysplasia
Only a gynecologist can know that a woman’s cervix is affected by dysplasia. To make a diagnosis, a specialist will be guided by laboratory test results and external manifestations - epithelial damage is characterized by a specific change in cell color. The affected areas have a light, often yellowish tint.
In mild forms of CIN, the epithelium appears smooth and uniform in color;
With moderate dysplasia, tissues are distinguished by obvious changes in cell structure, which are determined visually and by palpation. This is why doctors often call dysplasia erosion, so that the patient can understand what is happening to her organ and what it looks like at the moment. But still, these pathologies have a significant difference: erosion - erosion of tissue, dysplasia - pathological transformation of tissue.
Severe CIN is characterized by damage to the mucous membrane of the vaginal cervix. In addition, in women over 40 years of age, pathological processes can also occur in the cervical canal.
Clinical picture
Most often, dysplasia does not manifest itself in any way, and in 10% it is generally an accidental finding during examination. There are no characteristic signs of the disease, complaints appear only when a secondary infection is connected (bacteria, fungi or viruses), in which case the patient begins to worry about increased vaginal discharge, sometimes with an unpleasant odor, a feeling of itching and discomfort, spotting or bloody discharge after sexual intercourse, use tampons.
In severe cases of the disease, nagging painful sensations in the lower abdomen may appear. Since dysplasia is often combined with sexually transmitted infections, genital warts of the vulva and vagina, anus, erased gonorrhea or chlamydia are often diagnosed.
Diagnostics
In order to prevent cervical dysplasia, it is necessary to periodically visit a gynecologist, undergo a screening examination and be tested for HPV. Once every three years, it is recommended to undergo a cytological analysis, especially if the woman is at risk. Also a preventive measure for girls is vaccination against the HPV virus: it can be carried out at the age of 11 to 26 years (but not younger than 9 years and older than 26).
Methods for diagnosing cervical dysplasia
Instrumental and clinical:
- examination in mirrors - visual diagnosis of color changes, smoothness of the surface of the cervix, spots or epithelial growth, etc.
- Colposcopy is an examination using an optical device that magnifies the image tenfold.
Laboratory techniques:
- Pap test or Papanicolaou smear - collection of cytological material for its subsequent examination under a microscope. Detection of abnormal cells requires the following examination - a biopsy.
- cervical biopsy - during examination with a colposcope, a small amount of material is pinched off from the affected area of the cervix, which is further examined in the laboratory. A biopsy allows you to determine the thickness of the layer and the severity of tissue damage.
- HPV test is a scraping from the surface of the cervix.
- immunohistochemistry with tumor markers - an analysis performed in case of suspected oncology.
Which specialists should you contact?
Naturally, the first specialist in this field is a gynecologist - only he can diagnose dysplasia, conduct the necessary tests and examination. However, CIN is rarely caused by the papillomavirus alone. Therefore, it is necessary to undergo examination and, if necessary, treatment from the following doctors:
- endocrinologist - hormonal changes can significantly affect the development of abnormal processes in the genitals;
- infectious disease specialist - in addition to HPV, the body may contain other microorganisms that reduce the body’s resistance;
- immunologist - immunity can decrease due to a huge number of factors and various diseases.
Postoperative period
Recommendations in the postoperative period depend on the type and volume of intervention that was performed. The woman should be at rest, which will promote faster tissue healing.
Doctors recommend that within 2-3 months after surgery you avoid:
- Moving heavy objects.
- Physical education classes.
- Visits to baths, saunas.
- Sexual contacts.
To monitor the healing process, it is important for a woman to regularly visit a gynecologist after each menstrual cycle. If bleeding does not stop within 6 weeks after the intervention, an unpleasant odor, itching and burning are observed, this indicates the presence of complications. In this case, the recovery period may be delayed, and the uterine cavity will become scarred.
Treatment
The degree and depth of the lesion, as well as the duration of the disease, determine the treatment tactics for cervical dysplasia.
Common features can be identified for all stages of CIN:
- There is currently no effective drug treatment;
- all known treatment methods are based on the removal or destruction of affected areas of tissue.
The treatment method is selected by the doctor based on:
- degree of cervical infection;
- patient's age;
- a woman's desire to have children.
Treatment methods depending on the degree of infection
Mild degree - wait-and-see tactics are used and general restorative drugs are used. At this stage, it is necessary to prevent infectious and inflammatory diseases, and also to regularly appear for examination by a gynecologist.
Medium degree - depends on the depth of the lesion and the speed of spread: in 70%, shallow penetration is cured on its own, however, if HPV is detected, treatment begins immediately.
Usually at this stage drug treatment is required:
- douching, antiviral suppositories and tampons;
- antiviral drugs;
- immunostimulating agents.
If conservative treatment is ineffective, as well as if the disease persists, surgical intervention is performed:
- cauterization of the cervix with solkovagin;
- laser vaporization or conization;
- removal of pathologically changed areas using radio waves (using the Surgitron device);
- cryodestruction (cauterization with liquid nitrogen).
Severe degree - treatment is carried out using the same methods as when diagnosing moderate dysplasia. At this stage of the disease, treatment must be carried out urgently. As a rule, conization of the cervix is used as a surgical method.
Methods of surgical treatment
Knife conization
This is an old and almost a thing of the past method of removing tissue affected by dysplasia using a scalpel. In fact, it is not used due to the high efficiency and safety of other methods.
Cauterization with electric current
This method is also known as loop electroexcision, diathermocoagulation. The mechanism is to remove transformed tissue through electric current. The method is effective, but is not recommended for young and nulliparous women: after the procedure, scars remain on the cervix, which can lead to infertility or premature birth.
Cauterization is performed on an outpatient basis—there is no need to go to the hospital. The procedure is painless, since before the operation the doctor will administer an anesthetic injection.
Laser removal
Laser radiation is safer than using electric current because it does not leave scar deformities on the cervix. There are laser vaporization and laser conization of the cervix.
Laser vaporization means vaporizing infected areas without removing healthy tissue. The procedure is painless and safe for young nulliparous women planning to have children. The operation takes about half an hour and is performed on an outpatient basis.
Laser conization is a method of cutting off affected tissue with a laser beam. This method is also used to conduct a histological examination of cells affected by dysplasia. The procedure is performed under general anesthesia, as it requires precision in targeting the beam, otherwise healthy areas of the cervix may be damaged.
Radio wave method
One of the most popular and accessible ways to get rid of dysplasia, recommended for young and nulliparous patients, it is considered a safe and effective method. In this case, the Surgitron device is used.
Cryodestruction
Destruction of foci of dysplasia by freezing them with liquid nitrogen. The method is safe because it does not affect healthy areas of the organ. The procedure is performed on an outpatient basis and does not require painkillers. After cryodestruction, the patient may experience watery, transparent discharge of a yellowish tint.
To exclude relapse after treatment, patients need regular examination by a gynecologist and undergo a preventive examination (cytology smear, HPV tests, colposcopy).
Treatment of dysplasia during pregnancy
Cervical dysplasia does not adversely affect conception, gestation or fetal development. Therefore, it is recommended to postpone surgical intervention until the postpartum period.
You also need to remember the risk of premature birth in women who have undergone treatment for dysplasia through cervical conization.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Colposcopy | 1 800 |
| Taking a biopsy for diseases of the cervix using radiosurgery (excluding the cost of histological examination) | 5 000 |
| Coagulation using radiosurgery in the treatment of cervical diseases | 3 000 |
| Coagulation using radiosurgery in the treatment of cervical diseases with simultaneous biopsy taking (excluding the cost of histological examination) | 7 500 |
| Appointment with a surgical doctor (primary, for complex programs) | 2 700 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions