What is meningitis? Causes
Meningitis is a neuroinfection caused by viruses, bacteria or fungi. It affects the meninges, cerebrospinal fluid and is transmitted by airborne droplets. The infection is dangerous due to toxic shock, which occurs due to the rapid proliferation of viruses (bacteria) - pathogens and the effect of endotoxins produced by bacteria on the body. Basically, the causes of childhood meningitis lie in contact with a sick person or a carrier of meningococci. The causative agents of meningitis infection are classified according to the age of the child:
- Escherichia coli strain K, group B streptococci, and Lactobacillus monocitogenes are dangerous for a child’s body before the age of 1 month.
- Neisseria, pneumatic streptococci, hemolytic infection, streptococcus B most often affect children aged 1 to 3 months.
- For meningococci, hemolytic infections, and pneumstreptococci, the peak vulnerability of children occurs between the ages of 3 months and adulthood.
In addition, viral meningitis is a consequence of a child being infected with enteroviruses, adenoviruses, echo viruses, rubella viruses, herpes, encephalitis, and measles. Bacterial meningitis in children is caused by pneumococci, meningococci, salmonella, staphylococci, Haemophilus influenzae serous group B, and enterobacteria. If the neuroinfection was caused by microscopic fungi, then most often it is malarial plasmodium, spirochetes, candida or rickettsia. Fungal meningitis often accompanies endocrine or autoimmune pathologies of other body systems. In some cases, meningitis in a child occurs due to protozoan infestation. These are mainly amoebas and toxoplasma. This form of meningitis in children is less common than others. The most common forms are viral and bacterial.
Before the age of 28 days, the following factors increase the chance of developing the disease:
- Fetal hypoxia during pregnancy;
- History of concomitant infections;
- Severe prematurity;
- Complications during childbirth;
- Deviations during pregnancy.
At the age of 3 to 8 months, the number of babies who develop meningitis is also very high. In infancy, the development of meningitis may be preceded by improper or insufficient care of the baby, severe overheating or hypothermia of the child's body, and a sharp change in surrounding climatic conditions. In preschoolers, the risk of development is increased by purulent diseases of other localization, acute respiratory viral infections, influenza, previous TBI, and concussions.
Description
Serous meningitis is an inflammatory disease that occurs in the brain cavity of a soft texture, the source of which is harmful microorganisms (mainly viral), systemic disorders, the formation of neoplasms and cysts of a cerebral nature. Typically, the anomaly develops acutely with a high increase in body temperature. Patients report regular painful sensations in the head area, a meningeal symptom complex, and in rare cases, the functioning of the cranial nerves is disrupted.
The examinations consist of obtaining epidemiological information, details of a neurological examination, results of testing of the cerebrospinal substance, diagnostics of bacteriological and virological directions. Additionally, an EEG and magnetic resonance imaging of the brain are prescribed. As a therapeutic treatment, doctors use etiotropic techniques, dehydration, and rid the patient of toxins in the body. Doctors prescribe pharmacological agents aimed at eliminating infection, reducing fever, convulsive syndrome, etc.
Types of meningitis
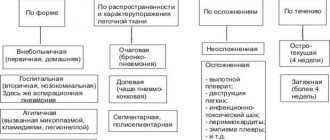
According to its origin, meningococcal infection is divided into the following types:
- Primary;
- Secondary.
The first type of neuroinfection is localized directly in the membranes of the spinal cord or brain. Secondary meningitis results from the spread of an infectious agent from other affected areas. According to the characteristics of the affected cerebrospinal fluid, meningitis in children is divided into the following types:
- Purulent;
- Serous;
- Hemorrhagic.
With purulent meningitis, a large number of bacteria and white blood cells are found in the test fluid. With the serous form of the disease, there are no impurities in the cerebrospinal fluid. And during hemorrhagic meningitis, children experience hemorrhages. Depending on the course of meningitis in a child, it can be chronic (lasting more than a month), subacute (from several days to several weeks), acute (up to 7 days), transient (death occurs in one day). Based on its extent, childhood meningitis is classified into the following types:
- Arachnoiditis is an inflammation of the arachnoid membrane of the brain. Has a specific clinical picture and course characteristics;
- Leptomeningitis - affects the pia and arachnoid membranes of the brain;
- Pachymeningitis - an inflammatory process affecting the hard membrane;
- Panmeningitis - meningitis infection affects all membranes of the brain.
How to protect yourself from illness
All parents should pay attention to the prevention of serous meningitis in children. In the summer, you should listen to local news - if an outbreak of meningitis follows after visiting open water, you should not allow your child to swim there.
Measures to combat the disease are generally reduced to maintaining hygiene rules:
- Drink boiled or specially purified water. This rule should be taken especially seriously by those who live in low-lying areas where wastewater may enter the water intake.
- Follow the rules of personal hygiene - be sure to wash your hands after visiting the toilet and before eating.
- Wash vegetables and fruits before eating (especially in the summer). Products can additionally be doused with boiling water - enteroviruses are afraid of high temperatures.
- Meningitis can develop against the background of other viral diseases - measles, mumps, influenza and even common ARVI. Therefore, be attentive to the follow-up treatment and recovery of your child after any such illness.
- If a baby has a weak immune system, he should not come into contact with rodents (even domestic ones), as they are considered carriers of serous meningitis pathogens.
Meningitis is a complex disease. Due to the carelessness of parents, the disease often has the most disastrous consequences. But if you raise the alarm in time and go to a medical facility, serous meningitis will go away quite quickly - in 10-12 days. And don’t forget about prevention – it’s better not to get sick at all.
When the first symptoms of the disease appear, contact an infectious disease specialist online or at a good infectious diseases hospital.
For more information about meningitis in children, watch the video:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://niidi.ru/dotAsset/e3e1899f-a522-4aa4-acd2-f28dedca3bc0.pdf
Rate how useful this article was
5 Voted by 1 person, average rating 5
Did you like the article? Save it to your wall so you don’t lose it!
The first signs of meningitis in children
The very first signs of meningitis in children are headache, photophobia, severe irritation from loud sounds, touches, repeated vomiting not associated with meals, after which there is no relief. But it is worth remembering that symptoms do not appear immediately after infection. The incubation period for meningitis ranges from 3 to 9 days.
Meningitis in adolescence
In adolescents, meningitis often begins with meningococcal nasopharyngitis - the back wall of the pharynx becomes granular and acquires a bluish-purple tint, which distinguishes this dangerous pathology from the usual viral form of the disease.
Other characteristic features:
- heat,
- weakness,
- drowsiness,
- attacks of dizziness,
- unbearable headache,
- nose is stuffed,
- the voice becomes hoarse.
In many ways, meningitis is similar to the common cold; a cerebrospinal fluid analysis will help make an accurate diagnosis.
Symptoms in children according to age
Up to 1 year and from one to three years
The following symptoms are characteristic:
- Anxiety;
- Severe compaction of the fontanel;
- Diarrhea;
- Convulsions;
- Dehydration;
- The crying or moaning of a sick child acquires a high-pitched sound;
- Lethargy;
- Blue discoloration of the nasolabial triangle;
- Refusal to eat, vomiting;
- Possible fever with cooling of the extremities;
- The child develops a pink rash from the feet to the face;
- A sick baby takes a specific position. He turns to the wall, bending his legs towards his stomach and raising his head;
- The child always bends his legs when tilting his head to his chest;
- Due to a spasm of the muscles in the back of his head, he cannot tilt his head;
- When they try to lift him, taking him under the armpits, the small child throws back his head and pulls his legs towards his stomach.
- At this age, the child’s condition quickly deteriorates, so you should not hesitate to call an ambulance. Any delay is fraught with death.
At the age of 3-4 years
The main symptoms are the same. The child suffers from drowsiness, photophobia, and aversion to any sounds or touches. The baby will be capricious and will completely cease to be interested in his favorite activities and toys. When you press on the area under the cheekbone, his shoulders will involuntarily rise, and when pressure is applied to the pubic bone, both legs will reflexively bend.
From 5 to 10 years
Characteristic complaints include a bursting headache, fever up to 41 degrees and above, a pink rash on the skin and mucous membranes, photophobia, sound fear, enlarged veins on the head and eyelids. Constant vomiting appears, which does not depend on meals. His consciousness becomes confused, a spasm of the eye muscles appears. Convulsions, refusal of food and water, paralysis of some muscles, strabismus, hearing and vision impairment, hallucinations, and difficulty breathing are observed. The key symptom of this age is that the child cannot rest his chin on his chest due to spasm or tension in the muscles of the back of the head. A sick child lies in the meningeal position - bends his legs towards his stomach and throws his head back. At the same time, he usually turns towards the wall. When trying to tilt his head to his chest, he always bends his legs.
During adolescence
Symptoms of meningitis may be accompanied by some symptoms of a cold. Adult children are worried about nasal congestion, very high temperature, severe headache, drowsiness, and constant dizziness. The posterior pharyngeal wall may acquire a bluish or purple tint - the main difference between meningitis and the common cold.
The essence of the problem
The inflammatory process in children is severe, affecting the central nervous system and some internal organs.
This disease occurs most often in childhood and adolescence, and failure to take timely measures can lead to death.
The disease can have a primary and secondary mechanism of infection.
In the first case, direct infection occurs through contact with a carrier of the infection, and in the second, brain damage occurs as a result of complications of diseases of other organs, when the infection is transmitted hematogenously.
Diagnosis of the disease
The disease is diagnosed in a hospital setting. Diagnosis of meningitis in a child consists of a survey about previous viral diseases, the severity of symptoms, the time of their onset, examination of the baby and collection of blood and urine for analysis. Serological methods are used to detect specific antibodies in blood serum. Along with these methods, a marker of damage to the meninges and identification of signs of damage to the meninges by provoking the meningeal position are used for diagnosis. The main diagnostic procedure is to perform a spinal puncture to examine the cerebrospinal fluid. If necessary, a small patient undergoes an X-ray of the skull, MRI, and neurosonography. The last method is used for newborns. If meningitis is suspected, consultation with a pediatrician, infectious disease specialist, pediatric ophthalmologist, or neurologist is necessary.
Consequences
Untimely or inadequate therapy in children leads to serious complications, since pathological processes affect the meninges.
Possible complications of meningitis:
| Name | Description |
| Asthenic syndrome | The child gets tired quickly and is unable to control his emotions. He finds it difficult to do mental and physical work. There is weakness and irritability. Periodically, headaches and cramps occur. |
| Hydrocephalus | The disease is characterized by high intracranial pressure due to the accumulation of large amounts of cerebrospinal fluid. The child's head circumference increases, the cranial sutures diverge, the fontanel becomes tense and swells. Ultrasound examination (ultrasound) will show expansion of the ventricles and cerebrospinal fluid space in the brain area. |
| Brain swelling | The pathological condition provokes a change in consciousness, stupor, stupor and, as a consequence, coma. Seizures and focal neurological signs sometimes occur. |
| Subdural effusion | The cerebrospinal fluid becomes inflamed and accumulates in the subdural space. Pathological foci are most often located in the frontal region of the brain. The child’s general condition worsens, fever persists even after antibiotic therapy. Consciousness is depressed and accompanied by convulsive syndrome. |
| Seizures and epilepsy | Swelling and pressure on the brain provoke disruption of its functioning. Seizures during illness are not evidence of epilepsy. The risk of developing it increases after recovery, as inflammation and swelling damage the brain. |
Complications of meningitis in children also include partial deafness and blindness, paralysis and even death. As a result of the illness, the child experiences delayed mental and physical development and autonomic disorders.
Treatment of meningitis
Treatment is carried out in a specialized infectious diseases hospital, since a child with meningitis requires constant monitoring of his condition and the ability to quickly place him in the intensive care unit if the need arises. Antibacterial therapy is indicated (penicillin, aminoglycosides). It lasts for at least two weeks. For viral meningitis, treatment is carried out with acyclovir, interferons, and immunomodulators. Depending on the origin of meningitis, the patient is administered antimeningococcal gamma globulin. In severe cases, children are placed in the intensive care unit, connected to a ventilator and given oxygen therapy until their condition stabilizes. Therapy should take place in a darkened room. During treatment, you must follow a diet, complete rest and bed rest. It is important to create a favorable psychological environment and calm the baby if he is worried, afraid or crying.
Clinical picture: symptoms, warning signs
Regardless of the etiology, meningitis symptoms in children are quite general and specific to this disease.
General manifestations
Characterized by a certain periodicity:
- prodromal period , which lasts about 1 - 2 days. It is manifested by nonspecific general symptoms, such as headache, general malaise, mild catarrhal symptoms, a slight increase in temperature;
- piritic period , during which there is a high fever of up to 39 degrees.
Meningeal signs
meningeal signs deserve special attention . Their presence often indicates the presence of an inflammatory process in the structures of the nervous system. What is it?
1. General cerebral symptoms : nausea, vomiting, photophobia, hyperacusis (increased sensitivity to sounds), changes in consciousness, children may have febrile convulsions.
2. Rigidity, that is, increased resistance of the neck muscles.
When a doctor checks this symptom, he does it as follows: a child lying on his back is tilted with his head forward so as to reach his chest with his chin. If the symptom is positive, then muscle resistance prevents this from happening.
3. Kernig's sign. For a child lying on his back, the lower limb is bent at a right angle at the hip joint and knee joint, then an attempt is made to straighten it. If the symptom is positive, then due to pain and resistance it is not possible to do this.
4. Brudzinski's symptoms: upper - when the child's head is bent (he lies on his back), then involuntary bending of the legs occurs at the knees and hip joints. Lower - when one lower limb bends at the knee, the other involuntarily bends.
There are also many other meningeal nominal symptoms, but this information is more interesting to doctors, and the doctor will in any case use those that seem most appropriate to him in this particular situation.
Symptoms in children and adults from the autonomic nervous system
- rapid heartbeat or, conversely, slowing of the heart rate (bradycardia);
- increase or, conversely, decrease in blood pressure;
- sweating;
- thirst;
- polyuria (increased urine production).
Complications after meningitis in children
With successful treatment and the absence of complications, the consequences of meningitis may disappear on their own within 5 years after recovery. It can be:
- Chronic headaches;
- Difficulty perceiving information;
- Memory loss.
With purulent complicated meningitis, complications are more serious:
- Mental retardation;
- Problems with vision or hearing;
- Epileptic seizures;
- Recurrence of meningitis;
- Encephalitis;
- Increased intracranial pressure;
- Brain swelling.
Prevention
- Vaccinate your child against rubella and measles. Influenza, meningococcus and other infections.
- When declaring a meningitis epidemic, it is advisable to limit the child’s contact with large numbers of people and visiting crowded places.
- Personal hygiene training.
- If it turns out that the child has been in contact with a patient with meningitis, chemoprophylaxis is carried out with an antibacterial course.
- Periodically give your child vitamin complexes to strengthen his immune system. It is advisable to do this in the autumn and spring.
In general, childhood meningitis can be recognized in time by the following triad: bursting headache, temperature 40-41 degrees, specific meningeal posture.
Komarovsky's advice
A pediatrician with many years of experience advises young parents to first take care of the prevention of meningitis. According to the doctor, it is worthwhile to ventilate the room in which the child is located as often as possible and control the level of air humidity, as well as teach the child to observe basic rules of personal hygiene.
An equally effective preventative measure would be to rinse the nasopharynx with saline solution using a special spray - this is a good way to maintain the moisture of the mucous membranes. Gargling will complement the procedure.
Komarovsky advises refraining from visiting a kindergarten or school with a fever and sore throat, as this can lead not only to infection of other children, but also to a deterioration in the child’s general condition, which will subsequently cause meningitis.
If it was not possible to protect the child from a dangerous disease, the doctor strongly recommends not delaying calling the doctor and following all instructions received.