Do you often experience abdominal pain, nausea, a feeling of heaviness after eating and belching? Perhaps a small but very aggressive enemy has settled in your gastrointestinal tract - the bacterium Helicobacter pylori. Helicobacter pylori is a special type of pathogenic bacteria that infects the stomach and duodenum. These microorganisms are parasites that produce large amounts of toxins that damage the mucous membrane of internal organs. Such damage leads to inflammation and the development of gastritis, ulcers and subsequently even cancer. Helicobacter pylori is cunning and insidious. Most of the microorganisms known today cannot survive in the acidic environment of the stomach, but for this bacterium such an environment, on the contrary, is preferable. Helicobacter pylori has a spiral shape and is equipped with several flagella that help it move along the walls of internal organs. She perfectly knows how to adapt to any conditions, feels “like a fish in water” everywhere, requires very little oxygen and, if necessary, can even change shape - become spherical or oval. Helicobacter pylori was first studied by two Australian scientists, Robin Warren and Barry Marshall, who were awarded the Nobel Prize for this discovery in 2005. And for several years now, doctors from all over the world have known that stomach diseases can be explained not only by genetic predisposition and poor diet, but also by insidious bacteria that have settled in the stomach. It turns out that you can get infected with gastritis and ulcers in the same way as with the flu.
What does Helicobacter pylori mean?
The bacterium Helicobacter pylori is widespread in the human population. There are statistics from which it follows that 60% of people have it. The acidity of gastric juice, which is aggressive for other microorganisms, does not pose any danger to it. This is the usual habitat for the bacterium, in which it exists for many years, destroying the mucous membrane of the digestive tract. Such exposure becomes a factor in the development of stomach and small intestinal ulcers, gastritis, duodenitis, and in complicated cases, combining these diseases. Long-term ulceration can transform into a cancerous tumor.
Not all infected carriers of this disease require antibiotic therapy. A minimal amount of bacteria cannot harm the human body, since they are restrained by the immune system. In some cases, immunity weakens.
Factors weakening protection:
- excessive physical stress;
- psycho-emotional overload;
- infections;
- abuse of bad habits;
- sedentary lifestyle;
- unhealthy diet: inclusion in the diet of smoked meats, marinades, spices, sour foods, which irritate the mucous membrane and create defects on it;
- violation of the diet: rare meals in large quantities, dry food.
In the initial stages of the disease, gastritis develops, which subsequently develops into an ulcer. A peptic ulcer threatens to perforate the wall of the stomach and intestines, causing bleeding or cancer. These transformations entail structural changes in other organs of the gastrointestinal tract: in the liver, in the pancreas.
Until 1970, it was believed that inflammatory processes in the gastrointestinal tract and gastric ulcers were caused by stress factors and poor diet. To prove what Helicobacter pylori infection leads to, its researcher, Australian scientist B. Marshall, drank a concentrate of this culture. During the study, it was found that after a few days he developed gastritis. For their work, Barry Marshall and his team were awarded the Nobel Prize in 2005.
When diagnosing diseases of the stomach and intestines, the gastroenterologist refers the patient for a diagnostic study. The purpose of diagnosis is to find the causative agent of the infection and assess the damage caused by it.
Diagnostic methods:
- analysis of gastric juice;
- biopsy of the gastric mucosa;
- blood test for biochemistry;
- PCR test for detection of antibodies to helicobacter pylori in blood serum.
Polymerase chain reaction will help detect infection even at minimal concentrations of bacteria in the human body.
Mechanism of appearance of skin symptoms
Violation of the functional state of the digestive tract is directly related to the condition of the skin. This nuance is the cause of various skin reactions when infected with Helicobacter pylori. The provoking factor is toxic damage to the body by bacterial waste products. Skin manifestations can occur in the form of acne, dermatitis, acne and other pathologies accompanied by the formation of pimples and redness of the epidermis.
Mechanism of symptoms:
- disruption of the absorption of nutrients provokes a lack of amino acids and vitamins;
- decrease in the protective properties of the skin;
- sebum secretion increases;
- the body tries to remove toxins through the pores;
- the consequence is the active proliferation of bacteria in the epidermis.
Helicobacter symptoms
The main warning symptoms that directly indicate infection with the bacterium Helicobacter pylori are frequently recurring severe pain in the stomach. Often the pain is localized on an empty stomach, decreasing after eating. Such symptoms indicate the formation of ulcers and erosions on the walls.
It should be mentioned that with helicobacteriosis, patients often complain of heartburn and heaviness in the stomach, and poor digestion of fatty meat foods can also be observed. In advanced conditions, nausea and, in rare cases, vomiting may be noted. To determine the presence of bacteria, a special test is used, which, using biochemical reactions, determines the content of immunoglobulins in the blood serum. In addition, endoscopy and a breath test are indicated.
Even if the causative agent of the infection has not yet been found during diagnosis, a person infected with the bacterium notices short-term signs of dyspepsia.
- How does the disease manifest itself:
- Hungry pain of low intensity, decreasing after eating;
- Nausea, less often vomiting;
- Belching;
- Flatulence, bloating.
It is quite possible that the intensity of these manifestations will decrease, and for many years the person will be confident that the tone is healthy, but if the risk factors coincide, the colony of bacteria will intensify its destructive work. These are smoking, alcohol abuse, infectious infection, and other reasons that reduce immunity.
After the discovery of the leading role of Helicobacter in the development of gastroenterological diseases, the frequency of relapses of gastritis and peptic ulcers decreased by 10-12 times. Currently, without diagnosis of the presence of bacteria in the patient’s body, treatment of these diseases does not begin.
Symptoms
The presence of Helicobacter in the human body does not mean that he will definitely get an ulcer. But the occurrence of this disease is quite possible if the patient has predisposing factors such as:
- poor nutrition;
- alcoholism;
- smoking;
- stress.
But chronic gastritis occurs when infected with Helicobacter in almost 100% of cases. It is chronic inflammation of the stomach that is the main manifestation of Helicobacter pylori. In this case, the patient experiences the following symptoms:
- Stomach pain. The localization of the symptom may change and move to the area of the duodenum. The pain can be sharp, aching or dull. A person may experience a feeling of fullness. Discomfort may occur during prolonged fasting, on an empty stomach or after eating.
- Heartburn. This feeling is almost impossible to confuse with any other discomfort. A person feels a burning sensation in the epigastric region, a burning sensation in the esophagus and even the larynx. This may cause chest pain, which is often confused with heart pain. It is also not uncommon for patients to develop an unpleasant sour or putrid taste.
- Belching. This symptom almost always occurs along with heartburn. Belching may taste bitter or sour. In some cases, there is frequent belching of air, which worsens after eating.
- Nausea. This symptom often occurs along with hunger pains. A person may feel sick on an empty stomach or 3 hours after the last meal. If the gastric mucosa is severely injured, nausea may be replaced by vomiting with blood clots.
- Intestinal disorder. Diarrhea is quite rare, but this symptom can also indicate the presence of Helicobacter in the stomach and duodenum of a person. There may be obvious blood in the stool in the form of clots or specks.
If the body is heavily contaminated with Helicobacter, a number of atypical symptoms may occur that indicate significant infection and progression of the disease:
- Decreased appetite to the point of complete absence.
- A sharp decrease in body weight that is not normal.
- Dry mouth and metallic taste.
- Bad breath in the absence of caries.
- The appearance of sticking in the corners of the mouth.
These are the symptoms of Helicobacter that require immediate treatment. If at least one of them appears, it is necessary to quickly seek medical help and begin diagnostics.
Causes of Helicobacter pylori infection
The bacterium cannot live in the open air at all. Typically, it is transmitted through human saliva and mucus through contact. Typically, infection occurs through household means through dishes and standard personal hygiene products, as well as through kissing. It is known that family and friends who often come into contact with the patient are always at risk.
When such a bacterium enters the human stomach through the esophagus, it does not die, despite the action of hydrochloric acid. Bacteria easily penetrate the mucous membranes, destroying tissue, which causes disruption of normal functioning. In this case, the gastric mucosa becomes inflamed, and then erosions, gastritis and ulcers develop. It is believed that if left untreated, the risk of stomach cancer increases significantly.
Since the most likely route for bacteria to enter the human body is through contact with the saliva and mucus of a patient, the following causes of infection exist:
- Kisses;
- Use of common utensils and personal hygiene items;
- Transfer of bacteria from mother to child.
Most often, relatives, friends, and family members of the carrier of the infection are at risk of infection. The transfer of bacteria from one carrier to another increases when basic hygiene standards are not observed and the level of culture is low. Residents of communal apartments, dormitories, social institutions, as well as doctors are at risk. In developed countries, the risk of developing heliobacteriosis is much less than in countries with a low standard of living. In Russia, the social map of the spread of Helicobacter is paradoxical - cases of ulcers and gastritis due to infection with this bacterium are often found in wealthy families.
Consequences of ignoring treatment
Ignoring therapy can lead to a wide variety of consequences that will have a purely negative impact on the human body. It is worth highlighting three main consequences that Helicobacter can lead to.
Peptic ulcer
The main cause of stomach ulcers is Helicobacter. The influence of this pathogenic microorganism on the occurrence of peptic ulcer disease has been proven by medicine. But the risk of developing the disease increases significantly if a person has genetically determined risk factors. Among them:
- Gender. Thus, ulcers occur 4 times more often in men than in women.
- Blood type. According to studies, people with the first blood group are at risk and suffer from ulcers 35% more often than others.
- Ability to detect the taste of phenylthiourea. For some, the substance is completely tasteless, while for others it has a bitter aftertaste.
Signs that an ulcer is caused by Helicobacter are the following:
- Hunger pains that occur 5-6 hours after the last meal.
- Night stomach pain.
- Pain clearly localized in the projection of the ulcerative defect. Usually under the stomach on the right or in the middle.
The onset of ulcers due to Helicobacter is quite rapid, and the occurrence of a perforated ulcer is also possible.
Stomach cancer
This consequence of exposure to Helicobacter is the most dangerous. A pathogenic microorganism leads to type B gastritis. If it is ignored for a long time and there is no competent treatment, the gastric mucosa atrophies and metaplasia occurs. This condition is considered precancerous, because metaplasia quickly becomes malignant.
According to statistics, in 50% of cases, cancer occurs due to the presence of gastritis B in a person. In another 46%, due to the degeneration of ulcers. A malignant tumor of the stomach often develops against the background of a progressive ulcer.
A characteristic sign that a person has cancer is persistent pain. The pain symptom does not occur at any particular period, hunger pains and discomfort after eating disappear. Instead, the person experiences constant pain that is almost impossible to eliminate.
Allergy
The cause of allergic rashes is also very often Helicobacter. This bacterium causes atopic dermatitis in people. This disease is a chronic skin disease. It is characterized by the appearance of rashes on such parts of the body as:
- face;
- neck;
- collarbone;
- elbows and knees;
- palms (back side);
- feet (back side);
- throughout the body (complicated cases).
Atopic dermatitis has characteristic features. One of them is itching. The itching sensation can be mild and subtle or very intense. Discomfort increases at night. In this case, when scratching the skin, short-term relief occurs. But under no circumstances should you scratch the areas of the rash. Thickening of the skin may occur, and if infection enters the wound, suppuration may begin.
But why does Helicobacter cause allergies? There are three reasons for this:
- The presence of bacteria in the body leads to immune-inflammatory reactions.
- Doctors suggest that the body produces immunoglobulin to fight Helicobacter, which often leads to allergies.
- Helicobacter impairs the body's defense response, causing toxins to be absorbed into the blood and leading to inflammation of the skin.
Causes Helicobacter and the appearance of rosacea on the skin of the face.
What does Helicobacter pylori look like?
With such a prevalence of the disease, it is quite natural to wonder what helicobacter pylori is? Here is a brief description of the microorganism: it is a spiral-shaped bacterium with flagella at one end. These flagella help Helicobacter move through the digestive system and attach to the gastric mucosa. The bacterium is able to transform its shape from spiral to oval or round.
The term helicobacter pylori comes from the name of its location - the pyloric part of the stomach. Bacteria are adapted to exist in the acidic environment of gastric juice; they exist without access to oxygen. To prevent the hydrochloric acid of the stomach from damaging Helicobacter, it secretes special enzymes, surrounding itself with it, neutralizing gastric juice. The flagella of the microorganism penetrate through the mucous membrane to the cells of the parietal layer, violating the integrity of the protective environment.
Characteristics of the activity of the bacterium would be incomplete without a description of the pathogenesis of Helicobacter pylori. It is the cells of the parietal layer of the stomach and intestines that provide the bacterium with food. It destroys them, simultaneously releasing ammonia and toxic substances, poisoning the body with the products of its vital activity. The body's defense system in the form of neutrophils seeks to destroy pathogenic microbes, but also directs its energy to the cells of the mucous membrane with which the bacteria have already interacted.
Penetrating through mucosal defects, hydrochloric acid actively acts on tissues that are not adapted to this, causing ulceration. How long do Helicobacter pylori live? The bacterium can exist in the pylorus of the stomach and in its bulb for several decades, until the patient undergoes a course of antibacterial therapy. Outside the human body, it lives for a very short time and dies very quickly.
Risk factors
Residents of large cities are most at risk of infection due to numerous contacts with potential carriers of helicobacter. Working in the same room with infected people, sharing meals and using bathrooms creates additional preconditions for disease transmission to occur.
Fungal diseases, such as the herpes virus, can contribute to the emergence of conditions favorable to Helicobacter.
Alcohol, unhealthy diet and others that injure the gastrointestinal tract can lead to activation of the pathogenic properties of the microorganism. Simply becoming infected with Helicobacter pylori may not be enough to guarantee traumatic consequences for the digestive system, but it is worth knowing how the bacterium can be transmitted in order to minimize health risks.
A diet low in vitamins is also a contributing factor to infection.
Research shows that the prevalence of the disease is noticeably higher in regions with low levels of vitamins in food.
How is the bacterium Helicobacter pylori transmitted?
Helicobacter pylori infection occurs through contact, through the saliva of the carrier. Another nutritional route of infection is quite possible, although much less common: through food or liquid. This infection is not transmitted by airborne droplets. The contact and household route of infection makes it possible to consider Helicobacter a “family microbe”, when if it is detected in one family member, it can be assumed with a high degree of probability (in 95% of cases) that the rest also have heliobacteriosis.
The most likely ways of transmitting the bacterium:
- Iatrogenic – during diagnostic procedures that involve insufficiently well-processed instruments, during endoscopy;
- fecal-oral – when contaminated products or water that have had contact with the feces of an infection carrier enter the human body;
- oral-oral – with kissing, when using someone else’s toothbrush, unwashed cutlery in canteens and cafes.
There is a theoretical possibility of transmission of the bacterium from domestic animals: pigs, cows, cats and dogs, as well as from monkeys.
Prevention of Helicobacter pylori infection
After carrying out therapy for the eradication of a pathogenic microbe, no earlier than a month later, diagnostic procedures should be repeated in order to monitor treatment.
Treatment success can be considered if the percentage of pathogen eradication is 80% or higher based on repeated diagnostic tests.
But even completely getting rid of the microbe does not mean being cured for life. It is possible to become infected with H. pylori again. Immunity to this pathogen is not developed.
To avoid getting infected again, you should follow preventive measures, which include the following rules:
- If a microbe is detected in one of the family members, everyone living with this patient should be examined, and if helicobacteriosis is detected, everyone should undergo a course of treatment. This is very important because transmission within families is extremely high. And in order to avoid re-infection, all family members must be “clean” regarding Helicobacter
- You should follow the rules of personal hygiene: use a separate toothbrush, cutlery, wash your hands thoroughly after visiting the restroom or the street, public places
- Do not finish eating from the baby’s plate or lick the baby’s pacifier or spoon
- Do not eat from reusable catering utensils
How dangerous is the bacterium?
There are two mechanisms of the pathogenic effect of Helicobacter pylori on the human body.
How dangerous is the bacterium?
- Helicobacter pylori endotoxins have a negative effect on tissue, damaging the endothelium lining the inside of blood vessels, affecting smooth muscle muscles;
- when exposed to it, immune-inflammatory reactions are activated and associated pathologies arise.
With the influence of bacteria, the digestive system becomes functionally imperfect, since the protective function of the gastric mucosa is disrupted and substances that previously did not enter it are absorbed into the blood. When Helicobacter pylori persists in the stomach for a long time, gastrointestinal motility is disrupted and the synthesis of hormones that stimulate gastric and intestinal peristalsis is disrupted.
Colonies of bacteria displace beneficial microorganisms of the digestive system, provoking the development of dysbiosis. The long course of chronic gastritis caused by it leads to atrophy of the mucosa and the formation of foci of metaplasia on it, when the typical covering of the wall of the stomach and intestines is transformed into atypical cells. In addition to these changes, the secretion of gastric juice, which performs a protective function that prevents the development of tumors, decreases. All these factors stimulate the development of stomach cancer, and less commonly, intestinal cancer.
The danger of this condition is that the patient may not feel significant pain, especially if cancer occurs against the background of atrophic gastritis. Much more often he experiences an aversion to protein foods, weakness, irritability, depression, and loses interest in his surroundings.
How is prevention performed?
The infection prevention regimen depends on the person’s age. The standard plan for taking a metaprebiotic is as follows:
- Children over 14 years of age and adults: 2 tablets, 3 times a day with meals. The total duration of the course is 30 days. The number of courses is determined for each person individually.
- Children over 3 years old: 1 tablet 3 times a day, during meals.
During clinical trials, it was found that a course of taking the metaprebiotic Stimbifide Plus led to complete eradication of Helicobacter pylori infection . In addition, the ascorbic acid contained in the composition helps strengthen the immune system and fight the inflammatory reaction that could occur during an infectious lesion.
Diagnostics
Some patients with helicobacteriosis may not experience certain symptoms. Special tests are used to determine the presence of bacteria. Histological and special urease analysis is indicated to identify Helicobacter pylori.
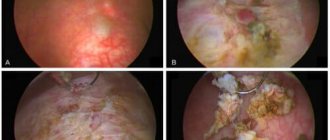
Cytological examination is based on obtaining fingerprint smears, which are taken during endoscopy, and this procedure also requires biopsy samples of the mucous membrane of the special antrum of the stomach. As a rule, a biopsy sample is taken specifically from those areas where deviations from the norm are visually most pronounced. A specialist in such areas may observe hyperemia and swelling. Often, spiral-shaped Helicobacter bacteria are located in the center of the mucus.
Such a cytological study determines three main degrees of contamination of mucous membranes with bacteria. If there are less than 20 microbial bodies, a weak contamination is diagnosed, which does not cause concern for human health. Cellular infiltration is also detected when microorganisms are detected in fingerprint smears and plasma cells.
Depending on the number of certain cellular elements, one can indirectly judge the expressed degree of activity and the inflammatory process. In addition, such a study reveals proliferative processes in the mucous membranes, dysplasia and metaplasia, as well as various malignant formations. However, the cytological method does not provide an idea of the structure of the mucous membranes.
A special urease test is considered an effective rapid method, which is mainly based on the activity of the microorganisms present. It is made using a special gel carrier containing urea, a special bacteriostatic agent and a special phenol-rol as a necessary indicator. This pH indicator allows you to make accurate conclusions about the specific condition of the mucous membranes of the stomach. A mucosal biopsy obtained from endoscopy is also included in this test.
In extremely rare cases, the test shows false negative results, which is possible if the Helicobacter pylori infection is weak. To increase reliability, specialists usually use histological and urease methods. After antibacterial treatment, they should be repeated. If necessary, a repeated course of combination therapy of the anti-Helicobacter type can be prescribed, which will avoid rapid relapses of the disease.
The special breath test is non-invasive and safe. It allows you to easily determine the level of colonization of mucous membranes with these microorganisms. This analysis is considered optimal for complete control of eradication therapy. This test should be performed on an empty stomach. First, special samples of background exhaled air are taken, and then after a light breakfast the test substrate is used.
Various histological methods are designed to quickly detect Helicobacter in biopsies, while simultaneously studying morphological changes. The Giemsa bright coloring method is the most accessible and simplest. With this test, microorganisms are clearly visible on the surface of the epithelium and in the depths of the pits. Another histological method for precise DNA hybridization is sensitive and highly specific. It allows the identification of numerous strains of Helicobacter pylori.
Other methods are also used for diagnosis. These include immunological and microbiological methods, polymerase chain reaction, as well as determination of antigen in feces. Typically, blood tests and endoscopy results are taken, as well as breath and stool tests.
On the subject: Test for Helicobacter pylori: types of tests and interpretation
Skin signs of bacterial infection
Common skin manifestations of Helicobacter pylori include acne, rosacea and seborrheic dermatitis. These pathologies have their own symptoms and development mechanisms. The main reason for their manifestation is considered to be the effect of toxic waste products of bacteria on the epidermis.
Rosacea
Localization of skin reactions with rosacea is observed in the forehead, chin and cheeks. Rashes can vary in intensity and appearance. Pimples are small formations with a dense consistency.
In the absence of therapy, the inflammatory process can spread to the mucous membranes of the organs of vision. The patient will be prone to conjunctivitis.
Acne
Acne is a small formation, the development of which begins with a pink spot. As its size increases, a rod with purulent contents is formed. The opening of the abscess occurs spontaneously. A characteristic crust appears at the site of the purulent formation. Acne can cause bluish spots on the skin, which can be extremely difficult to get rid of.
Seborrheic dermatitis
A distinctive feature of seborrheic dermatitis is the formation of characteristic red spots on the skin of the cheekbones, forehead, eyebrows and nasolabial folds. As the pathology progresses, yellow plaques form in their place. The formations cause discomfort with peeling and itching. Seborrheic dermatitis can cause the development of other skin diseases.
Treatment and prevention of helicobacteriosis
The main treatment of helicobacteriosis mainly involves long-term implementation of the necessary complex therapy, which is aimed at destroying harmful microorganisms in the human stomach (more about the treatment regimen).
It is this condition that is necessary for the complete healing of all erosions and ulcers on the mucous membranes. Even if symptoms of the disease do not appear, this is not a complete cure. Bacteria are capable of not manifesting themselves for a long time, while they remain on the walls of the stomach in a passive state.
It should be noted that the development of this disease is directly influenced by the lifestyle of a particular person. With smoking and alcohol abuse, with poor diet and constant nervous strain, the risk of infection increases significantly. To treat the patient, complex therapy is indicated, including the use of modern antibiotics and special medications to restore the mucous membranes.
Mandatory treatment is indicated for gastric maltoma, atrophic gastritis, gastrectomy for oncological formations, as well as for ulcerative conditions of the stomach and duodenum. It can be used not only during an exacerbation, but also during remission of the disease.
All treatment regimens for this Helicobacter infection must include at least three medications. Typically, these include two carefully selected antibiotics and a special proton pump inhibitor. With a double regimen, treatment will be ineffective in most cases. Therefore, experienced specialists always select a triple eradication scheme. The duration of this treatment is seven days. Pariet is considered one of the fastest-acting pharmacological drugs of the antisecretory and antibacterial type. It is included in complex therapy and is prescribed at least twice a day. Already on the first day of such treatment, a reliable antisecretory effect is noticeable. There is also no need to use this drug before starting antibiotics, which is a definite plus.
To prevent infection with this infection, it is recommended to take rosehip syrup daily for one month. The dosage should be 1 tsp. After the course of treatment, you should take a two-week break and, if necessary, repeat the prophylactic dose of the drug.
Also an equally important step is compliance with strict hygiene rules. You must always wash your hands before each meal and do not use dirty dishes and towels. You should not use other people's personal hygiene products. If helicobacteriosis is detected in one family member, all other family members are subject to mandatory examination.
How to treat Helicobacter pylori in the stomach?
A combination of drugs must be performed to accelerate the positive dynamics of treatment, since the bacterium quickly adapts to the drug effect.
Drug groups:
- antibiotics: Azithromycin, Clarithromycin, Levofloxacin, cephalosporins, Amoxicillin, Flemoxin Solutab, Augmentin, Amoxiclav;
- bismuth preparations to form protection for damaged tissues of the stomach and intestines: De-Nol;
- proton pump blockers to reduce the production of hydrochloric acid: Omeprazole, Omez, Ultop, Pantoprazole, Nolpaza, Rabeprozole.
In addition to the use of drugs, the patient is prescribed a therapeutic diet, which prescribes frequent split meals, excluding spicy, fatty foods rich in spices. It is prohibited to smoke, drink alcohol, or include sweets and carbonated water in your diet.
[Video] Dr. Berg - HELICOBACTER PYLORI: treatment WITHOUT antibiotics. 6 natural remedies for Helicobacter:
Read more: Effective methods of treating Helicobacter pylori
The big picture
Let's start by indicating characteristic information, without which it is impossible to understand how to deal with attempts to infect you. Yes, yes, some situations are conducive to the spread of infection. For example, drinking in . Even pure alcohol is unable to quickly suppress the spread of bacteria. So don’t think that alcohol is sterile, as degenerate alcoholics say.
The infection is extremely contagious and can withstand elevated temperatures well. Therefore, the only chance to get rid of it is to carefully treat the dishes with detergents. If there is at least one patient in the family, then there is a high chance of developing a similar picture in full for everyone. There was only one case of spontaneous disappearance - complete atrophy of the mucosa. When the microbe has nowhere else to live, it leaves, leaving behind an empty stomach.
It is possible that the disease is eliminated by one’s own immunity, but so far no such cases have been recorded. The bacterium has well-thought-out tactics. Invading the epithelium, it releases toxins that modulate the immune response, making it ineffective. Therefore, the antibodies produced do not cope with the situation, but aggravate it. This means that today there are no known cases of self-freedom from infection.
Meanwhile, a host of natural remedies have been discovered to suppress the development of bacteria. First of all, these are onions and garlic, as well as herbs:
- oregano;
- sagebrush;
- chamomile and so on.
What features does this bacterium have?
– The first is its ability to withstand a very acidic gastric environment, while most bacteria and viruses simply die. The second feature is the ability to cause inflammatory processes in the gastrointestinal tract. As it multiplies, it causes slow destruction of gastric cells, and the substances it secretes cause chronic inflammatory processes and gastritis.
You can get rid of the pathology after completing a course of antibiotic therapy. Specific medications are prescribed only by a gastroenterologist, after conducting the necessary examinations and referring the patient to additional instrumental diagnostic procedures.