General information
A dangerous infectious disease, anthrax also has other names - malignant carbuncle , anthrax .
From ancient Greek the word “anthrax” is translated as “coal, carbuncle.” This name of the disease is explained by the fact that the scab in the skin form of the disease has a coal-black color. This dangerous infection, caused by the bacterium Bacillus anthracis, affects animals and humans. The course of the disease can be different, but in humans it occurs, as a rule, in the carbunculous form. The characteristic symptoms of anthrax are intoxication , serous-hemorrhagic inflammatory manifestations on the skin, internal organs and lymph nodes. The disease occurs in cutaneous and septic forms.
As Wikipedia and other sources testify, this disease has been known since ancient times and is described in a number of sources that have come to us since ancient times. In the works of ancient scientists it was called “Persian fire” or “sacred fire”. In 1766, the manifestations of the disease were described in detail by the French physician Moran. Later it received the name “anthrax”, since in the eighteenth century the disease actively spread in Siberia. In his work “On Anthrax,” the doctor S. Andreevsky described the epidemic of the disease in Siberia, proving that the disease can be transmitted from animals to people. Since then it has received this name.
How the disease is transmitted, its characteristic symptoms and treatment are described in this article.
Biochemical properties
Bacillus anthracis produces enzymes that determine the biochemical properties of the microbe. Enzymatic reactions of cells:
- participate in the formation of glucose, dextrin, sucrose, and other substances;
- weak acid formation on bases with the introduction of salicin, glycerin;
- lack of fermentation of raffinose, sorbitol, inulin, arabinose, galactose;
- release of ammonia, utilization of citrates, formation of acetylmethylcarbinol;
- reduction of methylene blue, reduction of nitrates to nitrites;
- individual pure cultures of microbes (strains) produce hydrogen sulfide.
The enzymatic activity of the cells is well expressed, proteolytic properties consist of liquefaction of gelatin, hydrolysis of starch, and slow coagulation of milk.
Pathogenesis of anthrax
Photos of anthrax patients
The causative agent of anthrax, the bacillus anthracis , was first described in the mid-nineteenth century. In 1876, German microbiologist Robert Koch isolated it in pure culture.
Microbiology of the pathogen : Bacillus anthracis is a large gram-positive rod. The pathogen develops well on meat-peptone media and can produce exotoxin. This bacterium demonstrates high resistance to high temperatures and disinfectants. Bacterial spores can persist for many years. Vegetative forms of the bacillus die if they are boiled or exposed to disinfectants.
The gateway to infection is damaged skin, but in rare cases, infection can enter the body through the mucous membranes of the respiratory tract and gastrointestinal tract. As a rule, the pathogen in humans penetrates into the skin of the hands and head, and in more rare cases, the torso and legs. Mainly exposed areas of the skin are affected.
of toxins produced by the pathogen plays an important role in the pathogenesis of the disease After infection, the pathogen begins to multiply in the skin within a few hours. The pathogens form capsules, releasing an exotoxin, which provokes the development of dense edema and necrosis . At the place where the pathogen has penetrated the skin, an anthrax carbuncle . This is a serous-hemorrhagic inflammation with necrosis, around which the tissue swells and regional lymphadenitis . Local pathological changes develop under the influence of anthrax bacillus exotoxin, which leads to significant disturbances in microcirculation, tissue edema and coagulative necrosis.
At the first stage of infection, localized damage to regional lymph nodes occurs. Pathogens reach regional lymph nodes through lymphatic vessels. Further generalization of the process may occur: pathogens spread hematogenously to different organs.
In the cutaneous form of the disease, generalization of the infection, in which anthrax pathogens break through into the blood and develop a septic form, develops very rarely. As a rule, sepsis develops when the pathogen penetrates through the mucous membranes of the gastrointestinal tract and the membranes of the respiratory tract. In this case, the generalization of the process occurs as a consequence of a violation of the barrier function of the tracheobronchial or mesenteric lymph nodes. As a result of toxinemia and bacteremia, infectious-toxic shock may develop.
If aerogenic infection occurs, the spores are phagocytosed by alveolar macrophages. After this, they enter the mediastinal lymph nodes. Where the pathogen multiplies and accumulates, the mediastinal lymph nodes become necrotic. The consequence of this process is hemorrhagic mediastinitis and bacteremia . In turn, bacteremia leads to secondary hemorrhagic anthrax pneumonia .
If a person consumes contaminated meat, the spores enter the submucosa as well as the regional lymph nodes. In this case, the person becomes ill with the intestinal form of the disease. In this form, the pathogen also enters the bloodstream, and the disease becomes septic. Accordingly, any form of the disease can become septic.
The transferred disease leaves behind a strong immunity , although there are descriptions of repeated diseases 10-20 years after the first disease.
How is anthrax transmitted?
Photo of anthrax in animals
The disease is transmitted when a person comes into contact with the skin and fur of a sick animal, as well as by eating contaminated meat.
Anthrax in animals leads to human infection. Its main source is herbivores, in particular large and small livestock. Animals become infected when they eat contaminated food or drink contaminated water.
In turn, those people who work with animals and animal products are most often infected. Anthrax is not transmitted from person to person.
The following routes of transmission of anthrax are known:
- Contact - through damaged skin or mucous membranes, when a person cares for animals, processes carcasses, buries sick animals in cattle burial grounds, etc. Infection can also occur during excavation work in places contaminated with spores.
- Nutritional – when preparing and consuming food from the meat of sick animals.
- Airborne dust - when spores are inhaled.
- Transmissible - through insect bites.
The incubation period can last from a couple of hours to eight days. But in most cases its duration is 2-3 days.
Outbreaks of the disease are still being recorded. So, several years ago there was an outbreak of anthrax in Kazakhstan - the disease was confirmed in residents of the village of Aktogay. Later, outbreaks of the disease were also recorded in Kazakhstan. In 2021, there was an anthrax outbreak in Yamal (Yamalo-Nenets Autonomous Okrug), where more than two thousand animals died. You can read more about outbreaks in feature articles and abstracts.
Pathogen
The causative agent of the disease is Bacillus anthracis, an anthrax bacillus, one of the giants in the world of microbes, 6-10 microns long and 1-2 microns wide. The bacillus itself is very unstable in the external environment - it quickly dies when heated and using conventional disinfectants.
However, it is capable of forming a spore with a powerful capsule - and then the stability of the pathogen increases by an order of magnitude. The spore can remain in disinfectant solutions for hours and can withstand up to 20 minutes of boiling. In this form, the bacillus can survive in the ground for several decades.
It is these features of the anthrax causative agent, as well as the almost one hundred percent lethality of the pulmonary form of the disease, that made it possible to consider the anthrax bacillus as a biological weapon. A genetically modified bacillus, with introduced resistance genes against major groups of antibiotics, becomes a formidable weapon and is very attractive not only to the military, but also to terrorists.
There have been attempts to infect American government agencies with anthrax, but they failed due to terrorists’ ignorance of the specifics of using such bacilli as biological weapons.
But experts still recognize that the anthrax bacillus can serve as a biological weapon for both an individual terrorist and a group, moreover, with a higher probability than many other bacteria.
Classification
Anthrax is divided into two types - cutaneous and general (generalized). In turn, each of these varieties has several more forms.
There are three types of skin forms of the disease:
- Carbunculous - manifestations on the skin change from red spots to nodules, and then to dark ulcers. The patient is worried about weakness, chills, fever .
- Edematous - in the first days of the disease, large swelling appears on the skin. Later, a scab is observed, around which the skin turns red.
- Bullous - the disease begins with the appearance of blisters on the skin. Later they burst, resulting in extensive ulcers. Later, a characteristic black crust appears on their bottom.
The general (generalized) form is divided into three types:
- Pulmonary – the respiratory organs are affected. With this form of the disease, the prognosis is most often unfavorable.
- Intestinal - very difficult, there are signs of gastrointestinal damage and general intoxication. High risk of death, even if the patient is provided with adequate treatment.
- Septic – sometimes develops immediately, sometimes as complications of other forms. There is general intoxication and bleeding in the internal organs. Inflammation of the membranes of the brain and failure of internal organs often occur.
What it is?
Anthrax is an acute infectious disease that occurs predominantly in the cutaneous form, much less often in the pulmonary and intestinal forms with symptoms of sepsis.
Anthrax is widespread in many countries in Asia, Africa and South America. There are outbreaks of it on the territory of Russia - in cattle burial grounds in the Stavropol Territory, Belgorod, Voronezh, Kursk, Samara, Kirov, Rostov, Kurgan and Oryol regions, the republics of North Ossetia, Chuvashia, Buryatia, Chechnya, Tatarstan, etc.
This infection is classified as a zoonotic infection - that is, a person becomes ill either from the infected animal itself, or from its skin and fur. At the beginning of the century, the incidence of anthrax in Russia was widespread. Between 1901 and 1910, this severe infection affected more than 16 thousand people annually.
Currently, with the development of the sanitary and epidemiological service, with the advent of antibiotics, the incidence is only sporadic, manifesting itself only occasionally in isolated outbreaks. In Russia, from 15 to 50 cases of anthrax are registered annually. It should be noted that almost all of them are of a professional nature, that is, people who work with animals suffer.
Symptoms of anthrax in humans
Photo of anthrax symptoms in humans
The incubation period is usually 2-3 days. Signs of the disease depend on its form.
In the cutaneous form of the disease , which develops in 98% of cases, exposed parts of the body are affected. The most common type is the carbunculous variety. The disease is most severe if the carbuncles are localized on the head, mucous membranes of the mouth and nose, and on the neck.
As a rule, one carbuncle appears, but in some cases more such lesions develop - in complex cases, up to 20. At the place where the infection entered the body, a red spot with a diameter of 1-3 mm, of a red-blue hue, first appears. It looks like an insect bite. After a few hours, a copper-red papule develops at the site of the spot. At this time, the feeling of itching and burning is disturbing. About a day later or a little earlier, a bubble with liquid appears in place of the papule. It becomes bloody. When the patient itches, the blister bursts, sometimes this happens spontaneously. An ulcer forms at this site, with raised edges and a dark bottom. Serous-hemorrhagic fluid is separated from it. The ulcer gradually increases, and after a day its diameter can already reach 15 mm. Due to necrosis, after 1-2 weeks a black, dense scab, similar to coal, appears in the center of the ulcer. After 2-3 weeks, the scab separates and a scar appears at the site of the lesion.
In addition to skin manifestations after infection, the patient also experiences general symptoms:
- Increased temperature – chills bother you, the temperature lasts for 5-6 days.
- Weakness.
- Headache.
- Aching pain in the lower back.
In the generalized form of the disease, symptoms depend on its type. But this form of anthrax is very rare.
In the pulmonary form, the respiratory organs are affected. As a result of the inflammatory process in the lungs, disturbances in the function of the cardiovascular system develop. Cardiovascular failure develops. The patient has symptoms of severe pneumonia. This condition is life-threatening.
In the intestinal form, a severe course of the process is observed. Fever and chills, headaches, and dizziness . Signs of gastrointestinal damage also develop - nausea, vomiting with blood, severe abdominal pain, diarrhea with blood. The risk of death with this condition is very high.
In the septic form, due to intoxication of the body, the body temperature rises and pain in various organs of the body bothers us. Bruises appear on the skin, and multiple bleeding occurs in the internal organs. Inflammation of the meninges develops, internal organs fail. Blood pressure drops and heart activity is disrupted. Many anthrax bacteria are found in sputum and blood. Due to bleeding, peritonitis and cerebral edema, death is possible already in the first days of the disease.
Treatment
Anthrax is a bacterial infection that can only be treated with antibiotics. Patients are given powerful antimicrobial therapy with Penicillin or Ciprofloxacin. These drugs are administered intramuscularly for a week until the symptoms of intoxication completely disappear. Parenteral treatment is combined with oral administration of Doxycycline or Levofloxacin. Early use of antibiotics can prevent death. Along with antibacterial agents, patients are administered anti-anthrax immunoglobulin.
Detoxification consists of infusion therapy, administration of Prednisolone and diuretics. Usually colloid and crystalloid solutions, blood replacement fluids, albumin, and glucocorticosteroids are used. The main treatment is supplemented with drugs that support cardiac activity, vitamins, and microelements. Aseptic dressings are applied to the carbuncles. Surgical intervention is prohibited due to the high risk of generalization of infection.
The prognosis of the pathology depends on the clinical form. For skin lesions, it is quite favorable. Generalized forms are often fatal. Therapy started early gives satisfactory results. It is extremely important to see a doctor promptly. Death is possible even with adequate treatment. Persons with anthrax meningitis, pneumonia and sepsis die in 90% of cases.
Currently, specific infection prevention has been developed and is being actively carried out. Pasteur first discovered the anthrax vaccine in 1881. Cattle livestock were regularly vaccinated with this vaccine. Over the years it has been improved and since 1940 it has been used to immunize people. Non-specific preventive measures include: disinfection on farms, control of animal slaughter and meat sales, use of personal protective equipment when working with sick livestock.
Tests and diagnostics
If anthrax is suspected, doctors use a specific diagnostic algorithm based on laboratory and clinical-epidemiological data. Initially, the doctor analyzes the complaints, assessing the order in which they appeared. Also in the diagnostic process, an epidemiological history is important - an assessment of contact with infected animals, as well as contacts with other people after infection.
A general external examination is carried out, during which the doctor determines the presence of external signs of the disease, performs palpation and percussion to identify disorders of the internal organs.
The following laboratory methods are used in the research process:
- bacterioscopic;
- bacteriological;
- immunofluorescence (for early diagnosis).
Allergological diagnostics can also be used, which makes it possible to obtain a positive result after the fifth day of illness.
For laboratory tests, material is taken from carbuncles, and in the general form, blood, sputum, vomit, and feces are examined.
For complex diagnostics, the anthrax allergen is used - anthraxin .
Diagnostic measures
To make a diagnosis of pathology, it is necessary to obtain the results of laboratory tests of the patient’s biomaterial. It is studied under a microscope, inoculated on nutrient media and injected into the body of laboratory animals. Sputum, carbuncle discharge, feces, and blood are taken for analysis. Serological reactions and allergy tests are performed on patients if necessary. All studies with anthrax bacillus are performed by workers in laboratories of particularly dangerous infections.
Diagnostic scheme for anthrax:
- Collection of complaints and study of clinical manifestations,
- Epidemiological history - establishing contact with a sick animal,
- General examination and physical examination,
- Microscopy is an indicative method that allows you to detect gram-positive rods of a characteristic shape in a smear,
- Inoculation of material on special nutrient media in order to isolate a pure culture and identify the pathogen,
- Bioassays on laboratory animals,
- PCR - detection of genetic material of bacilli in a sample,
- Serology - determination of the level of antibodies in the blood by performing a thermoprecipitation reaction or performing a luminescent analysis,
- Allergic intradermal tests with anthraxin.
Despite such a variety of diagnostic methods, the main one is still the bacteriological examination of material from the patient. Sputum or vomit is inoculated on MPA and MPB for initial identification and growth. The dishes and test tubes are incubated for 24 hours at 37 degrees. After incubation, the growth pattern is studied. Rough colonies appear on the plates. From them, smears are prepared for microscopy, in which chains of bacilli are detected. Several typical colonies are subcultured onto agar slants to isolate and accumulate a pure culture. Further identification consists of testing with anthrax bacteriophage, determining the “pearl necklace” and identifying enzymes - lecithinase, phosphatase, hemolytic activity. The results of a classic bacteriological study allow a final diagnosis to be made.
Prevention of anthrax
Disease prevention involves implementing a number of activities at the community level to control the spread of the disease. We are talking about identifying and recording regions that are unfavorable from the point of view of the spread of the disease, routine checks of animals, identifying sick people and their hospitalization. It is mandatory to vaccinate people whose profession is associated with an increased risk of infection. It is important to follow all veterinary rules when caring for animals.
Enterprises and institutions must comply with sanitary and epidemiological rules (SanPiN). There should be a corresponding reminder there.
Important preventive measures should also be taken on an individual basis:
- Meat and meat products should only be purchased from places where they are carefully controlled.
- It is very important for those involved in the processing and sale of such products to adhere to all hygiene rules.
- When caring for animals, all veterinary and sanitary standards must be followed.
- It is important to vaccinate animals against anthrax.
- People who come into contact with sick animals or contaminated meat should receive emergency antibiotic prophylaxis.
- Get vaccinated if necessary.
- At the first warning symptoms, consult a doctor.
Toxins
The antigenic structure of anthrax bacilli includes polysaccharide and protein antigens. The somatic antigen is located in the wall of the microbial cell, has high heat resistance, and antibodies are not produced against it. The capsular antigen structure provides the antiphagocytic effect of cells.
One of the most important factors in the pathogenicity of the ulcer pathogen is the presence of capsular antigen. Penetrating into a living host organism, the bacterium is “wrapped” in a capsule shell, which protects it from various negative influences, including the action of phagocytic cells. The next important parameter of the high pathogenicity of anthrax bacillus is the complex toxin complex:
- Edematous edema factor, associated with the cua gene, the product of which is adenylate cyclase, causes tissue edema.
- The pag gene, a protective antigen, interacts with cell membranes and induces (promotes the manifestation) the synthesis of protective antibodies.
- The lethal factor associated with the lef gene leads to a fatal outcome of the disease.
The toxicity factors of a pathogenic cell act synergistically - together effectively. Plasmids take part in the synthesis of anthrax bacillus capsules. The first factor of the three-component exotoxin has a protein-carbon structure, the second and third are purely protein in nature.
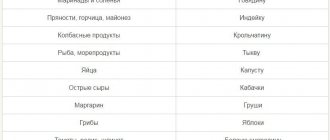
Diet
Diet 13 table
- Efficacy: therapeutic effect after 4 days
- Time frame: no more than 2 weeks
- Cost of products: 1500-1600 rubles per week
Patients are recommended to follow Diet 13 table . Recommended dishes include lean meat and fish, slimy soups and low-fat broths, dairy products, eggs, cereal porridges, vegetables, fruits, tea, rose hip decoction, etc.
A number of products are prohibited from consumption. This list includes:
- Spicy dishes.
- Fat meat.
- Fresh bread and pastries.
- Sausages and canned food.
- Fat cheeses and sour cream.
- Products that increase gas formation - legumes, cabbage.
- Coffee, alcohol.
More detailed information is contained in the “diet” presentation.
Consequences and complications
Anthrax can lead to serious complications, including:
- Brain swelling.
- Inflammation of the membranes of the brain.
- Bleeding in internal organs.
- Intestinal paresis.
- Inflammatory process in the intestines and abdominal cavity.
- Pneumonia.
- Pulmonary edema.
- A drop in blood pressure to a state incompatible with life.
Affected Populations
Anthrax is most common in developing countries. It can be found throughout the world, although the regions of the world with the highest prevalence of the disease are South and Central America, Southern and Eastern Europe, Asia, Africa, the Caribbean and the Middle East.
The largest recorded agricultural outbreak occurred in Zimbabwe, with more than 10,000 cases reported between 1979 and 1985.
In 1979, 79 cases of inhalation anthrax were reported in the Sverdlovsk region (now Yekaterinburg). 64 of these cases were ultimately fatal.
Outbreaks of the disease are recorded in Russia to this day