Leptospirosis is a severe infection in half of the cases and is found in all countries, except in the North and South Poles. People get sick especially often in tropical countries, from where tourists carry the pathogen around the world. The migration of infection is facilitated by the growing popularity of water sports. Leptospirosis affects more than a hundred species of wild and domestic animals - the main source of human disease.
Our expert in this field:
Nagibina Margarita Vasilievna
Infectious disease doctor, MD
Call the doctor
Description of the disease
Leptospirosis (Vasilev-Weil disease) is a type of bacterial infection spread by animals. It is caused by a strain of bacteria called Leptospira.
Leptospirosis is a zoonotic disease, meaning it is spread to humans from animals.
You can become infected with leptospirosis by touching soil or water contaminated with the urine of wild animals infected with the Leptospira bacteria.
Animals known to carry Leptospira bacteria include:
- cows;
- pigs;
- dogs;
- rodents, especially rats.
Once an animal is infected, the bacteria remains in their urine for the rest of their life. Most animals show no symptoms, but up to 1 in 10 infected dogs die from the disease.
Person-to-person transmission through sex is possible but very rare.
Historical reference
In 1914-1915, Japanese researchers Inada and others isolated the causative agent of the disease, Leptospira, and classified it as a spirochete. In subsequent years, leptospirosis was identified in many countries and its causative agents—various species of Leptospira—were studied. So, for example, in 1916-1918. In Japan, a 7-day fever with the pathogen Leptospira hebdomadis was described.
In 1927, in the Soviet Union, V. A. Bashenin described benign anicteric leptospirosis under the name “water fever.” The causative agent of this fever, Leptospira grippotyphosa, was isolated from the blood of a patient in 1928 by S. I. Tarasov and G. V. Epstein. In the study of issues of epidemiology and prevention of leptospirosis, great achievements belong to V. I. Terskikh, K. N. Tokarevich and A. A. Varfolomeeva and other Soviet scientists.
Types of leptospirosis
There are two main types of leptospirosis infection (mild (acute) and severe):
- With mild leptospirosis, a person develops flu-like symptoms such as headache, chills and muscle pain.
- In severe leptospirosis, a person develops severe, sometimes life-threatening symptoms, including organ failure and internal bleeding. It is caused by bacteria infecting major organs such as the liver and kidneys.
Mild leptospirosis is the most common type of disease, accounting for 90% of cases. It is not clear why some people develop severe symptoms.
Risk factors for developing severe leptospirosis include:
- children under five years of age;
- adults over 65 years of age;
- already have a serious illness such as pneumonia.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0.5 | 13.8 | 14.5 | 14.5 | 14.5 | 14.5 | 14.5 | 0.5 | 14.5 | 14.5 | 14.5 | 14.5 | 14.5 | 14.5 |
How common is leptospirosis?
Leptospirosis is most common in tropical areas of the world. However, it is becoming increasingly common in urban areas with poor sanitation, such as impoverished areas of large cities in developing countries.
Most cases of leptospirosis are sporadic (one-off), although large outbreaks have been reported since the flood.
It is estimated that 10 million people worldwide become ill with leptospirosis every year. It is difficult to determine exactly how many people die from leptospirosis because many cases occur in parts of the developing world where causes of death are not routinely reported.
The number of cases of leptospirosis is expected to continue to increase in the coming years as a result of global warming and an expected increase in flooding. Some experts estimate that the mortality rate from leptospirosis may range from 5 to 25%. Mortality rates from leptospirosis tend to be higher in countries where access to quality health care is limited.
Statistics
According to WHO, this disease kills 30 to 35 percent of people infected with it. Until the beginning of the 21st century, leptospirosis was one of the most common zoonotic infections (diseases that humans contract from animals) in the Russian Federation.
The dynamics of morbidity throughout the twentieth century is characterized by its unevenness. During certain periods in Russia, the number of patients was 7 thousand per 100 thousand people. The highest rates were recorded in the Middle Volga region and the North Caucasus. The introduction of routine vaccination and other preventive measures helped reduce the incidence rate to 300 – 700 cases per 100 thousand population.
In the early period of the 21st century, a surge in leptospirosis infections was recorded, due to an increase in the number of dogs in cities and the emergence of a massive spread of infection among animals as a result of the development of economic activities in cities. Today, from 1,500 to 2,500 cases of disease are registered annually in the country. More than half of the sick people live in the North Caucasus region. Also, a high level of infection of people with Leptospira is observed in the Republic of Adygea, Mordovia, and the Tula region.
Symptoms
Symptoms of leptospirosis in humans usually develop suddenly 7 to 14 days after exposure to Leptospira bacteria.
However, signs may develop 3-30 days after exposure.
Mild leptospirosis
Symptoms of mild leptospirosis in humans include:
- high temperature (fever), which is usually between 38 and 40°C (100.4 and 104°F)
- chills;
- sudden headaches;
- nausea;
- vomiting;
- loss of appetite;
- diarrhea;
- cough;
- a sore throat;
- non-itchy skin pain;
- muscle pain, especially affecting the muscles of the calves and lower back;
- conjunctivitis (irritation and redness of the eyes).
Symptoms of mild leptospirosis usually resolve within 5-7 days. However, a small number of people will experience a further phase of more severe symptoms known as severe leptospirosis.
Symptoms of the disease
When Leptospira enters the body, the parasite begins an incubation period. And during this time no symptoms occur. That is, outwardly, if he was not sick with anything before, the virus does not manifest itself in any way in the infected person.
And during this time, the causative agent of leptospirosis begins to actively multiply. The embryos penetrate the lymphatic system and settle on the internal organs. Particularly their favorite places are the kidneys, liver, lungs and spleen. And when the number of leptospira reaches the required volume, they enter the bloodstream. And then the symptoms begin to appear.
Typically, the incubation period of the parasite lasts from 2 to 30 days. The time it takes for leptospira to multiply in organs depends on the number of them ingested and the endurance of the body. The moment the parasites enter the circulatory system, the infected person experiences the following symptoms:
- the temperature begins to rise from 39 to 40°C;
- the patient feels severe chills;
- the muscles begin to ache unbearably;
- headaches do not stop;
- general weakness is felt in the body;
- gagging appears;
- there is a decrease in appetite;
- want to drink constantly;
- heart rate increases.
Within 12 days the temperature does not subside and continues to remain at around 39 - 40°C. Then it drops sharply for no reason. But, after a few days there is a possibility of a recurrence of fever. There are times when the body temperature seems to decrease, but continues to remain at around 37°C. This effect will last for a long time. This condition is called low-grade fever.
The next stage of the disease is redness of the skin, face, upper chest, and neck. A “red eye effect” occurs (injection of scleral vessels). Lymph nodes begin to increase in size. A rash may appear on the skin.
Adults are carried through the bloodstream and settle for a second time on the internal organs. And by external signs it is possible to determine on which organs the leptospira have settled. The muscles begin to ache simultaneously with the rise in temperature and last about 10 days. This can be noticed by how much the calf and lumbar muscles begin to ache. In the muscles of the neck and abdomen they are not so pronounced.
Popular Prevention of tick-borne encephalitis and treatment in children
No matter what position the body is in, pain is felt only when the patient moves or is touched. When the disease reaches its peak, the muscles begin to break down and this can cause kidney failure. Such symptoms give false indications when diagnosing the problem.
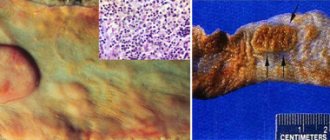
Liver damage
The liver may not suffer too much, but depending on the extent of the damage, the problem causes liver failure. If parasites have settled in this organ, then the most striking symptom is jaundice. And somewhere on the 2nd – 3rd or 4th – 6th day after Leptospira enters the body, the patient’s sclera begins to turn yellow. Then the yellowish tint spreads to the entire body. The illness lasts from one to several weeks.
The concentration of bilirubin in the blood increases significantly, and the urine turns dark. The stool becomes slightly discolored and the liver increases in size. And during diagnosis, the patient feels severe pain in this area. And along with the liver, an enlarged spleen and slight itching of the skin are possible. But the severity of the disease can be judged by the symptoms of jaundice. That is, the stronger the jaundice, the more severely the liver is affected.
Kidney damage
The kidneys are most often affected. As in the case of the liver, the more parasites settle on the organ, the more severe the disease progresses (up to renal failure and the development of uremic syndrome with a fatal outcome). These symptoms appear 7–10 days after infection. The amount of urine excreted is significantly reduced.
When you empty your bladder, you may see protein in your urine. No edema or high blood pressure is observed. The kidneys begin to work in reduced mode. Toxins are not disinfected and nitrogenous products appear in the blood. In the most severe cases, urine does not appear at all and anuria develops.
The central nervous system is not strongly felt in the initial stages. This could be a common headache or sleep disturbance. Delusions and hallucinations may occur due to high fever. When parasites recolonize organs, the following diseases may occur:
- meningitis;
- encephalitis.
Both symptoms are dangerous and can lead to the death of the patient.
Blood flow is the main “transport” in the blood supply system. It is through the blood that parasites multiply again in the internal organs. And, traveling through the circulatory system, they spray toxins, poisoning the inner lining of the blood vessels. External manifestations appear in the form of small hemorrhages: eyes, under the skin, blood from the nose, etc.
The most severe form of leptospirosis
Symptoms appear on days 3–4 and after that more serious hemorrhages may occur. But the most severe form of the disease is considered “disseminated intravascular coagulation syndrome.” This disease is characterized by the fact that the entire body bleeds at the same time. With leptospirosis, the cardiovascular system begins to behave unnaturally. The heart rate increases. Over time, their frequency returns to normal. But blood pressure may decrease. In some severe cases, myocarditis develops.
A patient who has been infected with Leptospira develops a strong immunity against this disease. But these indicators relate only to the group of parasites that infected him. But it may have side effects for a long time in the form of:
- muscle weakness;
- visual impairment;
- disruption of the central nervous system.
Causes and risk factors
Leptospirosis is caused by a strain of bacteria called Leptospira, which is found in some animals, including:
- mice;
- rats;
- pigs;
- cattle;
- horses;
- dogs;
- sheep;
- bats;
- raccoons
The bacteria live in the animal's kidneys and can end up in their urine. Bacteria introduced into soil or water can survive for weeks or even months.
You can become infected with Leptospira bacteria by drinking contaminated water, or if contaminated water or soil gets into your eyes, mouth, nose, or cuts on the skin. Less commonly, the infection can be transmitted to people who come into close physical contact with the blood of an infected animal.
Cases of leptospirosis in humans are rare, but occasional outbreaks can occur, especially during events that involve close contact with infected water sources, such as swimming in freshwater. A person can also become infected after a natural disaster such as a flood.
Person-to-person transmission is rare, but is thought to occur during sexual intercourse or when an infected mother passes the infection to her baby while breastfeeding.
Characteristics of the pathogen
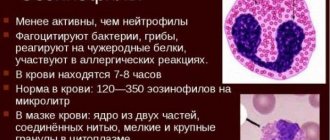
Leptospira are small spiral-curved bacteria of the spirochete class, belonging to the Gracilicutes department of the Spirochaetaks family of the Leptospira genus. Within Leptospira Interrogans, 23 serological groups have been identified, which include more than 200 serovars.
The pathogens have a characteristic appearance, which is why they received the name Leptospira (from the Latin Leptos - small, spira - curl). There are many types of bacteria. Some of them (Biflexa species) are safe for animals and humans, live in fresh and slightly brackish water, others (Interrogans species) are potential causative agents of a disease called leptospirosis. Both species are hydrobionts - they live in conditions of high humidity.
Morphology of pathogens
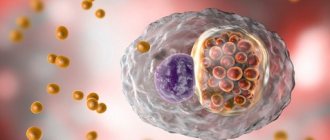
Leptospira are flexible microorganisms of an elongated corkscrew shape with numerous curls, carrying out complex translational-rotational energetic movement. Strict aerobes. Easily grown on artificial media.
- They have a length from 6 to 15 microns (sometimes there are species up to 30 - 40 microns), thickness - up to 0.25 microns.
- The number of curls ranges from 15 to 20 (primary curls). They fit tightly together (like a spring), which is why they look like a “string of pearls” under dark-field microscopy. One or both ends are thickened and curved, giving the microorganisms an S- or C-shape. There are strains of Leptospira that do not have hooks.
- Bacteria have 2 paired axial filaments coming from basal bodies located at the ends towards each other. There are no axial threads in the middle part. The axial threads provide energetic complex movement.
- The cytoplasm is homogeneous, tender, without inclusions. The shell is thin, structureless.
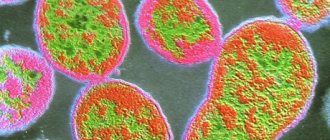
Microscopy
Aniline dyes are used to stain microorganisms. When stained according to Romanovsky-Giemsa (they stain poorly), the pathogens acquire a pale pink color (Gram-negative). To detect microorganisms, the Burri method and Morozov silvering are used (pathogens are painted black or brown); they are easily detected by dark-field microscopy, and more difficult by phase-contrast microscopy.
Rice. 3. In the photo of leptospira: A - dark-field microscopy, B - electron microphotography.
Antigenic characteristics
Leptospires have a common somatic antigen, which is of a protein nature with various variations in individual species, giving them species specificity. Antigens in humans and animals cause the formation of lysines, agglutinins, complement-fixing antibodies and precipitins. Within Leptospira Interrogans, 23 serological groups have been identified, which include more than 200 serovars. In our country, 13 serological groups of 27 serotypes are registered. The most common serogroups are Grippotyphosa, Pomona, Tarasovi, Hebdomadis, Iderohaemorrhagiae and Canicola.
Cultivation
Leptospira grows well in liquid and semi-liquid media. When growing on solid nutrient media, colonies are formed on days 8–10, round in shape, 1–3 mm in diameter. The optimal temperature for growth is 28 - 300C. Saprophytes grow at a temperature of 130C (distinctive feature).
Pathogenicity factors
The pathogenicity factors of Leptospira Interrogans are:
- Adhesins.
- Enzymes (fibrinolysin, lipase, plasmacoagulase).
- Extracellular substance (has cytotoxic and hemolytic properties).
- Endotoxin (have pyrogenic, lethal and skin-necrotic properties). Released when microorganisms are destroyed.
Rice. 4. - axial (axillary) thread, 2 - body of the microorganism.
Sustainability
Leptospires exist in water and humid conditions for many months (they are hydrobionts), which ensures the preservation of the species in natural conditions.
In fresh water bodies (rivers, lakes) microorganisms remain viable for up to 200 days, in wastewater - about 10 days, live in slurry for 1 day, in wet soil - up to 3 months, in dry soil - 2 - 3 hours, in swampy soils on soils - up to 200 days, on food products - several days. Retains activity when frozen.
Bacteria are not very stable in the external environment. They quickly die in salt lakes, estuaries and sea waters. Sensitive to sunlight, UV rays and heat. They quickly die when dried out, exposed to alkalis, acids and disinfectants. They die instantly in acidic environments. Dissolves in bile acids.
Rice. 5. Leptospira Interrogans on a polycarbonate filter (electron micrograph).
Diagnostics
Mild leptospirosis is difficult to diagnose when it is in the acute (early) stage because the symptoms are similar to many other more common infections, such as the flu.
Additionally, many of the tests commonly used to investigate flu symptoms are not very effective at diagnosing leptospirosis.
Therefore, a diagnosis of the disease is usually only considered if the patient experiences symptoms of severe leptospirosis.
Successful diagnosis usually requires a detailed personal history of the patient. You should tell your doctor if you:
- have recently traveled to parts of the world where leptospirosis is widespread;
- have recently been exposed to a fresh water source such as a river, lake, sewer or pond;
- have an occupation that involves exposure to animal urine or animal blood, such as farming, animal care (veterinary care) or working in a slaughterhouse.
A diagnosis of leptospirosis can be confirmed by performing a series of blood and urine tests to detect the presence of Leptospira bacteria in the blood or urine.
Preventive measures
In order not to find out what it is, leptospirosis after infection, it makes sense to get acquainted with this disease in an “absentia” form.
With timely and correct treatment, the disease goes away quickly
To prevent the development of this severe infectious disease, basic principles of prevention should be followed:
- Monitor health indicators of farm animals.
- Conduct vaccinations for people in contact with animals and during epidemic outbreaks.
- Regularly monitor the condition of the water.
- Minimize the spread of rodents.
As a rule, the prognosis of the disease is comforting. Mortality occurs only in cases where diagnostic and therapeutic measures were not taken in a timely manner. According to statistics, fatal cases of all leptospirosis do not exceed two percent. The percentage increases to twenty if there is a massive epidemic.
Treatment
Acute leptospirosis
Most cases of acute leptospirosis can be successfully treated with a five to seven day course of antibiotics. A tetracycline antibiotic called doxycycline is the preferred choice.
Side effects of doxycycline include:
- headache;
- runny nose;
- stomach upset;
- diarrhea.
These side effects should go away after completing the course of antibiotics. An alternative antibiotic such as erythromycin .
Side effects of erythromycin include:
- nausea;
- abdominal pain;
- vomiting;
- diarrhea.
It is very important to complete the prescribed course of antibiotics, even if you feel better. This is because stopping treatment before all bacteria has been killed may cause a more serious infection to return.
pain relievers such as paracetamol or ibuprofen can be used to relieve symptoms such as headache, fever and muscle pain.
Seek medical advice if, despite treatment, symptoms do not improve after 7 days.
Severe leptospirosis
Almost all cases of severe leptospirosis will require hospitalization. The underlying infection will be treated with intravenous antibiotics (antibiotics that are given directly into the bloodstream).
Question answer
In this section I will answer questions on the topic that dog breeders ask most often.
Is it possible to vaccinate against leptospirosis?
Getting vaccinated against leptospirosis is not only possible, but also necessary. If you live in an area that is free from leptospirosis, do not flatter yourself. Tomorrow, prosperity may disappear, because there are many carriers of infection - rodents, stray dogs and cats.
Complex and single vaccines against leptospirosis have been developed for dogs.
A vaccination schedule with Nobivak vaccines has been developed. The figure shows that puppies are immunized against distemper, enteritis, hepatitis (DHP) and leptospirosis simultaneously at 8-9 weeks and consolidated at 84 days. The biological product DHPPi (Pi-parainfluenza) and RL (rabies plus leptospirosis) are used. Vaccinate adult dogs annually, once, according to the same schedule as twelve-week-old puppies. If recommended by your veterinarian, additionally immunize your pet against leptospirosis with the monovaccine.
I anticipate the question: “Can leptospirosis occur in a vaccinated dog and if so, what are the symptoms? My answer is: there are no vaccines that provide 100% protection.
Objective reasons:
- vaccination during the incubation period;
- individual characteristics of the dog;
- crowded conditions in the nursery;
- the dog became infected with a leptospira serotype, the antigens of which are not in the biological product.
Human factor:
- violations of storage and (or) transportation rules;
- non-compliance with quarantine measures - you decided to walk the dog before the bactericidal antibody titer had formed;
- vaccination without prior deworming;
- improper maintenance and feeding.
The symptoms of the disease in the vaccinated dog are erased.
Can it be cured without consequences?
A recovered dog gains lifelong immunity. However, no one can guarantee that the dog will not subsequently develop some disease. It is impossible to determine what it is: the consequences of leptospirosis, an independent pathology or a symptom of another disease.
Therefore, be prepared for the fact that your pet will develop health problems over time. When taking a medical history, notify your veterinarian that your dog has had leptospirosis.
What tests are taken to diagnose leptospirosis?
Analysis for leptospirosis consists of biochemical and serological tests of blood and urine. The veterinarian will take a blood sample and you will need to collect urine. It should be warm and fresh, picked less than two hours ago. If leptospirosis is suspected, the sample is sent to a state laboratory.
How can you help at home?
Place the dog in a warm place on soft bedding and call a veterinarian. Trying to cure your pet on your own will waste time.
Complications
Without treatment, the disease can cause a number of complications:
- acute liver failure such as hepatic coma;
- acute renal failure;
- bleeding;
- damage to the membranes of the eyes;
- myocarditis;
- paralysis, paresis;
- infectious-toxic shock.
Control measures
On a farm where leptospirosis is diagnosed, it is prohibited:
- Export of livestock for breeding sale or for other purposes.
- Import of animals not vaccinated against leptospirosis.
- Grazing of unvaccinated livestock in places where there were sick people.
- Sales of products from animals forcedly slaughtered.
- Cattle are allowed onto dry meadows a week after diseased animals have been removed.
In a farm unfavorable for leptospirosis, the premises and surrounding area are disinfected after each case of infection is detected. Subsequently, they are treated every ten days until the quarantine is lifted. Deratization is carried out regularly. Water for drinking is brought to the pasture. Milk is given to animals after boiling.
It is prohibited to feed carnivores unprocessed slaughter products of a forced slaughtered animal. Pets that are not vaccinated against leptospirosis are not allowed to exhibit.
Vaccine
Prevention
If you are traveling to parts of the world where leptospirosis is common, you should limit your exposure to water. If you cannot avoid contact with fresh water sources such as rivers, ponds or lakes, you should ensure that you wear appropriate protective clothing.
You should also only drink sealed bottled water or fresh boiled water. Always cover any cuts or abrasions with waterproof bandages and clean any wounds as soon as possible.
Try to minimize exposure to animal urine by avoiding areas where animals may urinate, such as bedding and litter trays. If you suspect you have been exposed to animal urine, clean the affected area of skin as soon as possible.
Never touch a dead animal with your bare hands.
Antibiotic prophylaxis
Antibiotic prophylaxis is when you take antibiotics as a precaution against infection. However, there is limited evidence of the effectiveness of antibiotic prophylaxis for leptospirosis, so it is usually used only in exceptional cases, such as:
- for emergency workers working in disaster areas where there is a known outbreak of leptospirosis cases;
- for soldiers serving in areas with high rates of leptospirosis;
- for animals infected with animals known to carry Leptospira bacteria.
Etiology
The causative agent is a bacterium from the genus Spirochaetaceae, which lives and reproduces in stagnant water, as well as in the thickness of bottom silty sediments. Afraid of drying and sunlight. Resistant to freezing. Able to penetrate through scratches, intact skin, mouth, eyes, mucous membranes.
The reservoir of infection is rodents, as well as recovered animals. They acquire lifelong immunity, but remain leptospiron carriers for 3 years after infection. The incubation period lasts from 2 to 12 days. The peak incidence occurs at the end of summer or beginning of autumn.
A dog gets the pathogen by drinking from a puddle or pond of water or coming into contact with the feces of rodents or relatives. Infection through contaminated food is possible. Hunting dogs are at particular risk. An unbalanced diet contributes to the development of symptoms of the disease.
Leptospira live in puddles
Puppies become infected in utero, suffer severe illness and, as a rule, die.