Causes of thyroid cancer development
Risk groups for thyroid cancer include:
- patients who have undergone radiation therapy in the neck and head area. Exposure to ionizing radiation can trigger the development of a malignant tumor several years later. Radiation therapy stimulates active division, growth and mutation of body cells, which can subsequently cause the formation of papillary and follicular thyroid tumors;
- residents of areas exposed to radioactive radiation. Thus, after the Chernobyl accident, the number of people with malignant lesions of the thyroid gland increased 15 times. Radioactive rains that occur after nuclear weapons testing are also fraught with danger;
- persons who have had benign nodular neoplasms in the thyroid gland for a long time (nodular goiters, recurrent nodular goiters, chronic forms of nodular thyroiditis);
- patients diagnosed with thyroid adenoma;
- people suffering from chronic inflammatory processes or cancer of the genital organs, endocrine system, breast;
- family members with a hereditary predisposition. Of no small importance for the anamnesis is information about cancer diseases recorded in the past in close relatives. Family diseases such as polyposis, Cowden's syndrome, medullary thyroid carcinoma, Gardner's syndrome and others can become the basis for the formation of a malignant tumor of the thyroid gland. Numerous studies have confirmed the presence of a special gene that is responsible for the development of a malignant tumor;
- women suffering from hormonal imbalance during menopause, pregnancy and lactation are at risk of cancer;
- workers in hazardous industries (hot workshops, working with heavy metals, ionizing radiation);
- people with bad habits. Thus, nicotine contains carcinogenic products, and alcohol abuse leads to a weakening of the body’s protective function;
- persons subject to frequent stress and depression. Frequent psychological stress leads to weakened immunity, which provokes many diseases, including thyroid cancer.
It should be noted that an accelerating factor for the development of the disease can be either a single disease or a combination of several syndromes.
Final chord
So, here we come to the last lines of our article. It might seem that we are completely against ultrasound of the thyroid gland, but this is not so. There is a risk group of patients who need to have an ultrasound of the thyroid gland (for example, a family member has thyroid cancer). It is also impossible to ignore the fact that ultrasound has greatly advanced doctors in the early diagnosis of aggressive, fast-acting forms of thyroid cancer. However, most endocrinologists, especially abroad, are against doing an ultrasound of the thyroid gland when there are no symptoms of the disease! Essential reading, in our opinion, is the work of Professor V.V. Fadeev. “Just in case...” [28].
In this article, a highly qualified doctor draws the reader’s attention to the fact that doctors often evaluate the results of laboratory and instrumental tests only on the basis of generally accepted norms. In case of non-compliance with this “norm”, the patient is considered sick. It is very important to understand that a person is an individual, and the norm for each person can vary depending on the characteristics of the body. Therefore, we must treat not the tests, not the disease, but the patient . The doctor needs to evaluate not only the numbers on the test sheet, but also the patient’s condition, as well as the quality of life that awaits the person after treatment. This is called clinical thinking, which, unfortunately, is often absent from doctors in an age when we want to blindly trust numbers, and a machine begins to think for a person.
You can familiarize yourself with these and other thoughts at the link we left [26].
So, our dear readers! Based on everything we've covered above, we'd like you to draw three main conclusions:
- Do not do an ultrasound of the thyroid gland “just in case”, without any symptoms! Not on the advice of a friend, not because they said so on TV, not even if the doctor told you so (only if he clearly explains why you need to do an ultrasound).
- If you have a nodule, there is a 90% chance that it is benign.
- If you fall into the remaining 10%, remember that most thyroid cancer responds well to treatment and has a favorable prognosis.
Have a nice day everyone, and take care of your thyroid glands and nerves. 
Classification of thyroid cancer
Systematization of thyroid cancer involves differentiation by type (source of development of thyroid cancer), stage (degree of development), measures of prevalence and the presence of metastases.
Based on the histological appearance of the neoplasm, cancer is divided into:
- Papillary - 70-80%;
- Follicular - 10-20%;
- Medullary - 5-8%;
- Anaplastic (undifferentiated) - 2.5-4%.
Lymphoma, sarcoma, fibrosarcoma, and metastatic cancer are much less common; epidermoid cancer. These types of malignant tumors account for up to 2% of all forms of thyroid cancer.
The International Histological Association has developed the TNM classification (tumor - tumor, nodus - node, metastasis - movement). The systematization of tumors is based on three components:
- T—prevalence of primary tumor formations;
- N - absence or presence of metastases, as well as their intrazonality in regional lymph nodes;
- M—prevalence of metastases in organs distant from the main tumor.
The numerical index next to the component indicates the level of prevalence of the malignant neoplasm:
- T—primary tumor;
- TX - insufficient information to classify the primary tumor;
- T0—no primary tumor;
- T1 - the tumor is located within the thyroid gland and is no more than 2 cm in size;
- T2 - the neoplasm does not extend beyond the thyroid gland, tumor size is 2-4 cm;
- T3 - tumor neoplasm is limited to gland tissue, size - more than 4 cm;
- T4a - nodular formation, regardless of size, has spread beyond the boundaries of the thyroid gland and has grown into nearby tissues;
- T4b - tumor grows into the carotid artery, paravertebral connective tissue or mediastinal vessels;
- N - adjacent lymph nodes;
- Nx - there is not enough information to classify regional lymph nodes;
- N0 - no metastases in adjacent lymph nodes;
- N1 - there are lesions by metastases of nearby lymph nodes;
- N1a - metastatic foci are found in pretracheal, paratracheal and prethyroid lymph nodes;
- N1b - metastases are widespread in the submandibular, jugular, supraclavicular and mediastinal lymphatic areas. The focal lesion may be contralateral, unilateral, or bilateral;
- M - metastases;
- M0 - metastases are not detected in distant organs;
- M1 - distant metastases are present;
- Mx - damage to distant organs by metastases cannot be determined.
In addition, thyroid cancer is grouped by stages of development:
- Stage I - a local tumor that does not deform the thyroid gland, no metastases were detected;
- Stage II-a - a single tumor neoplasm or multiple nodes that deform the gland without invading the thyroid capsule; metastases are not found in adjacent lymph nodes;
- Stage II-b - local tumor, metastases are found in the lymph node on the side of the tumor;
- Stage III-a - a single tumor or multiple nodes that deform and grow into the capsule of the gland; compression of the esophagus, trachea, paresis of the recurrent nerve may be observed, metastases are not detected;
- Stage III-b - local tumor, metastases are present in regional lymph nodes;
- Stage IV-a - tumor has grown into nearby tissues and organs, regional metastatic process has not been confirmed;
- Stage IV-b - a tumor of any localization with metastasis to distant or adjacent organs.
Thyroid cancer is defined as primary or secondary. In the first case, the tumor is located directly in the gland, in the second, the tumor is initially localized in a neighboring organ with invasion into the gland.
Histogenetic classification of thyroid cancer
| SOURCE OF DEVELOPMENT | HISTOLOGICAL STRUCTURE OF THE TUMOR | |
| benign | malignant | |
| A cells | Papillary adenoma Follicular adenoma Trabecular adenoma | Papillary carcinoma Follicular carcinoma Undifferentiated cancer |
| B cells | Papillary adenoma Follicular adenoma Trabecular adenoma | Papillary carcinoma Follicular carcinoma Undifferentiated cancer |
| C cells | Solid adenoma | Solid cancer with stromal amyloidosis (medullary cancer) |
Lymphomas
Lymphomas are also fast-growing tumors. It is quite difficult to differentiate a neoplasm due to the fact that lymphoma can form against the background of autoimmune thyroiditis, which complicates diagnosis. However, lymphoma can also develop as an independent disease. A rapidly growing tumor involves the lymph nodes in the pathological process, and a process of compression of the mediastinal organs develops. If diagnosed early, lymphoma is highly treatable with radiation therapy.
The thyroid gland can be affected by metastases of malignant neoplasms localized in various organs. The process of metastasis of the gland is extremely rare. The source of focal lesions by metastases can be cancer of the stomach, intestines, lungs, pancreas and mammary glands, and lymphoma.
Consequences after surgery
The main complication after surgery for thyroid cancer (if the entire gland or a significant part of it was removed) is hypothyroidism. This condition causes severe symptoms because thyroid hormones have important functions. However, hypothyroidism can be successfully corrected with hormonal drugs. You will have to take them for life.
Other possible complications after surgery:
- Hoarseness or loss of voice
. This symptom may be temporary or permanent. It often occurs due to irritation of the larynx by the endotracheal tube. A more serious cause is accidental damage to the laryngeal nerve during surgery. - Damage to the parathyroid glands
. They are small glands that are located on the posterior surface of the thyroid gland, in pairs above and below. The parathyroid glands produce hormones that regulate calcium levels in the blood. When they are damaged, the level of calcium in the blood drops, which is manifested by muscle spasms, tingling and numbness in the arms and legs. - A large hematoma
can form in the neck area with intense bleeding. As after any surgical intervention, infection and suppuration are possible. To prevent such complications, antibacterial drugs are used.
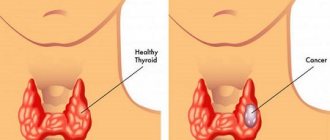
Symptoms of thyroid cancer
At the initial stage of tumor formation, the clinical picture does not differ in pronounced symptoms. It must be taken into account that in most cases, thyroid cancer and its symptoms develop against the background of a benign goiter (struma), which has existed for a long time. One of the first alarming symptoms is a rapidly enlarging goiter, the surface of which becomes lumpy and the structure more dense.
Tumor nodes can arise in a healthy gland, affecting only one lobe. As the tumors grow, they invade the entire thyroid region. Spreading to the back of the throat, the tumor causes compression of the fusion organs and is manifested by the following symptoms:
- lymph nodes become inflamed;
- swelling appears in the neck;
- change in voice timbre (hoarseness);
- difficulty swallowing;
- pain in the throat and neck area.
The thyroid gland is located close to the skin. In this regard, the newly formed nodes are easily palpated. You can even detect them yourself. Single nodes, as a rule, are benign in nature. However, as they develop, malignancy occurs. Timely diagnosis of thyroid cancer and its treatment, carried out adequately and on time, helps stop the pathological process with a successful outcome.
Cancer withdrawn into itself
Our traditional understanding of thyroid cancer, namely its development, has fundamentally changed thanks to three studies in 2014 (Thyroid cancer trilogy) [3–5]. It would seem that all malignant tumors undergo progression as they develop, and therefore require early diagnosis and surgical treatment. For the first time in human history, the existence of “self-limiting cancers” was discovered, which are malignant, but do not progress to lethal forms due to the limited ability to divide the cells that make up the tumor. Of course, there are also so-called lethal thyroid cancers. The difference between them lies in the origin of the cancer cells, which determines the development of the disease and its outcome. In the second case, the cells seem to be hidden for a long time, for years and even decades, and then, for still unclear reasons, they suddenly begin to divide and lead to an unfavorable outcome. However, at the moment it is believed that it is the “self-limiting” types of thyroid cancer that make up the majority.
Diagnosis of thyroid cancer
The set of diagnostic methods for determining thyroid cancer includes:
- objective examination;
- functional study;
- modern visualization methods;
- cytological, molecular genetic, immunocytochemical research.
An objective examination involves palpation of the thyroid gland. Tumors larger than 0.8 cm and located in the anterolateral and anterior parts of the gland are easily palpable. Upon palpation, inflammation of the lymph nodes of the jugular zone is detected in a number of patients.
Functional studies are based on detecting changes in the process of thyroid homeostasis.
Modern methods of visualizing thyroid tumors include:
- Ultrasound is a primary diagnostic method. Allows you to detect a node with a size of 1 mm, determine its size, contours, and examine the blood flow;
- radioisotope scintigraphy: the method is based on a comparative analysis of the absorption of radionuclides by the healthy and tumor parts of the thyroid gland;
- computed tomography - usually prescribed at an early stage of the disease. The method evaluates the presence of primary and metastatic tumor nodes, their location in the retrosternal region along the neurovascular bundles and retrotracheal localization;
- magnetic resonance imaging. MRI is commonly used to detect clinically undetectable metastases in the mediastinal and cervical lymph nodes. If the tumor process spreads beyond the boundaries of the gland, then MRI allows one to evaluate the retrotracheal or retrosternal location of the tumor;
- Positron emission tomography is a unique modern method for diagnosing thyroid cancer. PET together with computed tomography is prescribed to detect the presence of metastases and relapses in operated patients in cases where there is no accumulation of the radioisotope;
- classic x-ray: informative in case of spread of metastases to the lungs and lymph nodes of the mediastinal organs.
The basic method in diagnosing thyroid cancer is a cytological examination - a fine-needle biopsy followed by analysis of the biopsy sample.
Laboratory blood tests in patients with thyroid cancer usually show a decrease in hemoglobin and an increased level of ESR. The medullary form of cancer is characterized by an increase in the level of calcitonin in the blood.
Treatment
For thyroid cancer, surgical interventions are used, treatment with radioactive iodine, hormone therapy, chemotherapy, radiation, and targeted therapy are used. Treatment tactics are chosen based on the type and stage of cancer and the patient’s condition.
Find out the exact cost of treatment
Surgical treatment of thyroid cancer
Surgery is the main, radical method of treating thyroid cancer. If a fine-needle biopsy reveals tumor cells in the specimen, the first option is surgery, except in some cases of anaplastic cancer.
If, in differentiated forms of cancer (papillary or follicular), the tumor is small and does not spread beyond the thyroid gland, a lobectomy (hemithyroidectomy)
: the affected lobe is removed along with the isthmus. This helps maintain the production of thyroid hormones. Sometimes such an operation is performed for diagnostic purposes if, after a fine-needle biopsy, an accurate diagnosis cannot be established.
However, most often it is necessary to resort to removal of the entire gland - thyroidectomy,
or most of it -
subtotal resection
.
After this, you will have to take a synthetic analogue of thyroid hormones - levothyroxine -
.
If there is a suspicion that cancer cells have spread to the cervical lymph nodes, the latter are also removed. Surgeries to remove thyroid cancer are performed extrafascially, and it is important to carefully examine the entire thyroid gland and all areas where there may be regional metastases. In case of regional metastases on the affected side of the neck, the tissue is excised within the fascial sheaths. Particular attention should be paid to the fiber in the paratracheal zone and the anterosuperior mediastinum. After surgery, radioactive iodine therapy is prescribed to destroy remaining tumor cells and prevent recurrence.
Radioiodine therapy
Almost all the iodine that enters the human body goes to the needs of the thyroid gland. If radioactive iodine is administered to a patient, it will penetrate the gland tissue and destroy cancer cells without affecting other organs. For radioiodine therapy, the radioactive isotope of iodine I-131 is used, the same as for radioisotope research, only the dose of radioactivity will be much higher.
Papillary and follicular cancers are sensitive to radioactive iodine therapy; medullary and anaplastic tumors are insensitive. Typically this type of treatment is prescribed in the following cases:
- For inoperable tumors.
- After surgery, when the lymph nodes were affected, to prevent relapse.
- >If there are distant metastases.
In order for radioiodine therapy to bring maximum effect, the patient’s body must have a sufficiently high level of thyroid-stimulating hormone (TSH). You can increase it in two ways:
- Administer TSH drug.
- After removal of the thyroid gland, stop taking levothyroxine for several weeks. The level of the hormone in the blood will decrease, and the pituitary gland will begin to actively produce TSH to stimulate the no longer existing thyroid gland. During this time, the patient will have to endure some symptoms caused by the lack of thyroid hormones: increased fatigue, constipation, depression, poor concentration, muscle pain.
Before starting treatment, you need to reduce the amount of iodine in the body. The doctor will give some recommendations regarding diet: for 1–2 weeks you will have to give up iodized salt, soy, seafood, eggs, and dairy products.
Hormone therapy
After removal of the thyroid gland, the level of thyroid hormones in the human body drops sharply. This leads to some serious disorders, severe symptoms. The pituitary gland is activated and begins to produce TSH to stimulate growth and activate the thyroid gland, but it only stimulates the growth of cancer cells. Thyroid hormone medications help solve both problems. After thyroidectomy they will have to be taken for life.
Radiation therapy
In addition to therapy with radioactive iodine, thyroid cancer can be treated with radiation from external sources, that is, using radiation therapy in the classical form. It is prescribed for medullary and anaplastic cancers that do not respond to iodine. Typically, procedures are carried out 5 days a week for several weeks.
Chemotherapy
Chemotherapy works very little against thyroid tumors, but most often it is not necessary. Your doctor may consider using chemotherapy in two cases:
- For anaplastic cancer in combination with radiation therapy.
- For advanced cancer that does not respond to other treatments.
Targeted therapy for thyroid cancer
Targeted drugs are most widely used for medullary tumors that do not respond well to radioactive iodine therapy. Vandetanib is prescribed
or
cabozantinib
. Both drugs come in tablets and need to be taken once a day. They help stop the growth of cancer, but it is unknown how much they can prolong the life of patients.
For differentiated cancer that does not respond to other treatments, sorafenib
and
lenvatinib
. These drugs block the growth of blood vessels that feed the tumor and some proteins that promote the proliferation of cancer cells.
Book a consultation 24 hours a day
+7+7+78
Prognosis for thyroid cancer
The scenario for the development of the disease depends on the type of cancer, stage, treatment methods and age of the patient. In general, once diagnosed with thyroid cancer, the prognosis is favorable. With timely diagnosed tumors, up to 80% of patients can be completely cured. However, with sarcomas, lymphomas and anaplastic forms of thyroid cancer, a high percentage of unfavorable outcomes is observed.
We can say that mature people cope with the disease more successfully than patients under 20 and over 60 years of age.
Observation and forecast
Observation period
- 1st year after treatment – once every 3 months
- 2nd – 3rd year after treatment – once every 4 months
- 4th – 5th year after treatment – once every 6 months
- 6th and subsequent years after treatment – once a year
Forecast
| 5-year survival rate: | 10-year survival rate: | |
| Papillary cancer | 95,3% | 94,2% |
| Follicular cancer | 90,1% | 85,7% |
| Medullary cancer | 87,8% | 80% |
Prevention of thyroid cancer
Preventive measures for the development of thyroid cancer involve timely treatment of any morphological or functional abnormality of the thyroid gland. Regular preventive examinations for people at risk (workers in hazardous industries, residents of areas with high radiation, patients who have received radiation therapy, etc.) are of no small importance.
In order to prevent iodine deficiency, it is recommended to consume seafood, iodized salt, and also avoid unnecessary, frequent fluoroscopic exposure.
What do doctors think about this problem?
The problem of overtreatment of thyroid cancer exists not only among patients, but also among the medical community.
Of course, the choice of whether to remove the thyroid gland or not lies more with the patient than with the attending physician. And the patient may well choose surgical treatment tactics. And the doctor must determine how much thyroid tissue needs to be removed in a particular case.
To reduce overdiagnosis, the American Thyroid Association recommends against screening and biopsy of small thyroid masses in the absence of other clinical symptoms [6].
Clinical manifestations of the disease
The clinical picture is vague, symptoms vary from person to person. The thyroid gland is painless on palpation. To accurately establish a diagnosis, a highly differentiated selection of diagnostic methods is necessary, since lumps in the thyroid gland can be a sign of a benign tumor and do not lead to metastases.
If at the time of detection of a lump in the tissues of the thyroid gland a person is not yet 20 years old, in 95% of cases it is oncology: benign tumors do not appear in adolescents.
Symptoms of the disease
The initial stages of the disease are asymptomatic. But with careful attention to health, you can detect the first signs: small balls and nodular clots directly under the skin, palpating the neck area in front under the chin. The nodules are elastic, painless, and their mobility is limited. They roll under the skin without growing.
With the development of oncology, the nodules increase in size and lose elasticity, and the lymph nodes become enlarged and painful. If there are no signs of colds, this is sufficient reason to visit an oncologist and endocrinologist.
An increase in tumor size leads to a feeling of squeezing of the throat. This is accompanied by a change in voice, sore throat, difficulty swallowing, and shortness of breath. Frequent convulsions, increased body temperature, increased sweating, loss of appetite, weakness. The symptoms are similar to an acute viral disease, but taking antiviral drugs does not give positive dynamics.
When a thyroid tumor is visualized, but the lump is still mobile, serious symptoms of a malignant pathological process in the body appear:
- Enlarged lymph nodes in the areas adjacent to the thyroid gland.
- Swelling of the neck, shortness of breath and asthma attacks.
- Cough, sore throat, hoarseness or hoarseness of voice.
- Pain in the neck area that radiates to the ears.
As the tumor grows, the number of cancer cells also increases - the thyroid gland begins to produce its hormones in smaller quantities. Symptoms of hyperthyroidism appear. A sign of disease progression is a feeling of constriction in the larynx, a lump in the throat, and swelling of the neck veins. As a result of swelling, the neck loses mobility. Symptoms of body intoxication are noted. A progressive tumor compresses the trachea and esophagus.
Progressive cancer leads to sudden weight loss, insomnia, and chronic fatigue. A decrease in the level of hormone produced leads to apathy and loss of interest in life.
Associated symptoms include hair loss and tingling sensation in the arms and legs. The voice acquires a low pitch.
Forecast
The effectiveness of treatment and the quality of future life depend on the type and stage of the disease. For 2010, survival statistics were presented by the following figures.
| Five-year patient survival | Stage 1 | Stage 2 | Stage 3 | Stage 4 |
| Papillary cancer | almost 100 percent survival rate | almost 100 percent survival rate | 93% | 51% |
| Follicular cancer | about 100% | about 100% | 71% | 50% |
| Medullary cancer | about 100% | 98% | 81% | 28% |
The five-year survival rate for anaplastic (undifferentiated) thyroid carcinomas, most of which have reached stage 4 at the time of diagnosis, is about 7%.
Author:
Nikita Aleksandrovich Korobov, anesthesiologist
Oncology detection
If cancer is suspected in the tissues of the endocrine gland, it is necessary to determine whether the process is malignant. Methods used:
- Blood analysis using immunoenzymes to determine the content of tumor markers.
- Needle biopsy. The procedure allows you to identify tumor nodes and recognize their nature. Using the method, the actual size of the cancer lesion is determined. This is a reliable diagnosis. If there is any doubt about the results, an open biopsy is used, which involves surgery: a small part is cut off from the tumor and a rapid examination is performed.
It is worth making a reservation: even if a marker is detected, the presence of oncology cannot be stated unambiguously - there are known cases of increased levels of these compounds in the body of completely healthy people. There are also other cases: when there is a cancerous formation in the thyroid gland, but the tumor marker is not detected.
- Ultrasound. A safe procedure for establishing a type of cancer diagnosis. It is the main method for preventive examinations of patients at risk. Allows you to diagnose the disease in the early stages, determine the number of nodes, their size and location.
- Histological analysis. This procedure is carried out immediately before surgery. It is necessary to determine the extent of surgical intervention, clarify the localization of oncology, and prevent undesirable consequences.
- Magnetic resonance imaging is a procedure that accurately shows the stage of cancer development.
- Positron emission tomography is used to clarify the form of oncology and determine its stage.
PET-CT scanner
Provided that the disease is in an advanced stage, highly specialized medical methods are used to diagnose its features:
- Radioisotope scanning. The method is valued for its ability to determine the spread of metastases due to iodine-containing elements accumulating in them.
- Laryngoscopy. The method is used when the vocal cords are affected by metastases to determine the degree of paralysis of the vocal apparatus and brain.
- Bronchoscopy. The method is used to assess the condition of the trachea.
Additional information about a cancerous tumor can be obtained using x-rays. The following procedures are performed using an X-ray machine:
- Pneumography is a procedure that allows you to determine the exact size of an oncological formation.
- Angiography is a procedure that assesses the degree of involvement of blood vessels in the pathological process.
- X-ray of the trachea is a procedure to diagnose the condition of the esophagus.
Indications for diagnostic examinations are individual. Their set is determined by the doctor.
Determination of hormone levels as a basis for diagnosis
Assessing the degree of damage to the thyroid gland, an assessment of hormonal levels is carried out. The levels of the following hormones in the body are measured:
- TSH is thyroid-stimulating hormone. Stimulates the growth of thyroid cells, produced by the pituitary gland. Based on the results of an analysis of its content, one can not only identify the disease, but also understand whether the treatment was effective. If its concentration does not exceed 0.1 mIU/l, then the treatment was effective. If the hormone concentration is higher, this indicates a risk of relapse.
- T3 – triiodothyronine. This is a biologically active hormone that indicates the quality of the gland.
- T4 – thyroxine. The concentration of the hormone serves as an indicator of the functioning of the internal secretion organ.
- PTH is parathyroid hormone. Produced by glands located near the thyroid gland. A high concentration of this hormone in medullary thyroid cancer indicates the spread of metastases throughout the body.
Cancer cell metastases
Stages of thyroid cancer
When the suspicion of oncology is confirmed by the results of various diagnostic procedures, for the correct choice of treatment methods for types of cancer, an accurate determination of the stage of the disease is necessary. Features of symptoms and the patient’s ability to objectively assess his feelings allow us to describe the disease in stages:
- Stage 1 of the disease. A tumor measuring 2 cm is located inside the gland, occupying only one lobe and without changing the contours of the endocrine gland. The patient can independently detect it by palpation. There are no metastases. There are no other signs of a pathological process at this stage.
- Stage 2 carcinoma. The tumor is located in the capsule, but grows and reaches 4 cm in diameter, as a result of which the contours of the gland are deformed. The patient feels slight discomfort in the larynx. The neoplasm is not only palpable, but also becomes noticeable externally. There is multiple appearance of small cancerous nodes that do not grow into the capsule. There may be metastases on the part of the endocrine gland where the cancer originally occurred. It is recommended to begin treatment immediately to ensure it is as effective as possible. In 95% of cases, after starting treatment at this stage, the prognosis is favorable.
- Stage 3 thyroid carcinoma. The tumor grows into the capsule. It develops quickly and compresses nearby organs: the trachea and larynx. Regional lymph nodes increase in size. The tumor spreads by metastases to the lymph nodes on both sides of the neck. Symptoms increase: difficulty swallowing, shortness of breath, and attacks of suffocation are noted. A growing tumor causes compression of the esophagus - dysphagia develops. The mobility of the vocal folds decreases due to damage to the recurrent nerve - the patient’s voice changes. Sometimes the changes are minor, sometimes significant. But with the help of laryngoscopy, it is possible to detect changes in the vocal folds even with minor changes in the voice.
- Stage 4 thyroid carcinoma. The tumor grows into the tissue of neighboring organs. The thyroid gland increases in size and becomes immobilized. The patient's condition worsens. As a result of the pathological process, metastases begin to spread not only to neighboring tissues and organs, but throughout the entire body. This stage is characterized by decreased appetite, weight loss, and increased body temperature. The accompanying symptoms of stage 4 thyroid cancer are determined by which organ is affected by metastases. The lymph nodes of the neck most often become the area of spread of metastases. As a result of the inflammatory process, they become dense and increase in size. As a result of fusion with the skin, their mobility decreases.
However, metastasis in the lymph nodes does not interfere with curing the disease.
When the trachea is damaged, the main symptom is a cough with large amounts of sputum and blood in it. There is a feeling of chest compression, difficulty breathing, and chronic fatigue.
If oncology metastasizes to the brain, the symptom will be causeless headaches, for which conventional painkillers do not help. Visual acuity and coordination of movements decrease. Epileptic seizures are possible.
If the tumor metastasizes to the bone tissue, the bones become brittle. The most common bone tissues with metastasis are the bones of the skull, spine, pelvis, and ribs. On X-rays, bone lesions from cancer metastases appear as dark voids or growths.
Metastases to the liver cause hepatitis. Digestion is disrupted, the patient feels heaviness in the right hypochondrium. In severe forms, bloody stools and vomit in the form of coffee grounds are noted.
Metastases in the adrenal glands are practically not felt by the patient, but they can lead to acute adrenal insufficiency, the symptoms of which are low blood pressure and hemophilia. Reduces the production of sex hormones.
Metastases
The timing and intensity of metastasis in thyroid cancer depends on the type of disease.
So, in the papillary form, metastasis begins late and is inactive. Medullary tumors grow faster and metastasize more actively to regional lymph nodes.
The most aggressive variant of this disease in terms of metastasis is anaplastic. With this form, metastases begin to appear very quickly in distant organs such as the liver, lungs and bones.
Do you need a consultation with an oncologist and endocrinologist? Contact us in any convenient way!