Pancreatitis, like cirrhosis, is considered to be a disease of alcoholics. 70% of patients with acute or chronic inflammation of the pancreas are indeed heavy drinkers. But they are not the only ones who have pancreatitis. For example, it is very often found in patients with gallstone disease. This is due to the peculiarities of the work of two neighboring organs - the gallbladder and pancreas (read more here). Over the past 30 years, the prevalence of the disease has more than doubled, and now there is a persistent trend towards its rejuvenation. Let's figure out what happens to the body during pancreatitis and whether it can be cured.
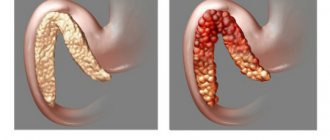
Exacerbation of chronic pancreatitis
Chronic pancreatitis is characterized by long-term development of the inflammatory process in the pancreas. The cells of the organ gradually die off (the tissues lack the ability to recover). Periods of remission are followed by exacerbations. In the first case, there may be no symptoms of the disease; in the second, a characteristic attack occurs, accompanied by severe pain and abnormalities in the digestive system.
Risk of exacerbation:
- violation of the secretory function of the pancreas;
- local death of tissues of the digestive organ;
- internal bleeding;
- spread of the inflammatory process to neighboring organs;
- purulent formations on the affected areas;
- peritonitis of the abdominal cavity.
Clinical examination
Diagnosing chronic pancreatitis is not easy because imaging studies and blood tests for the disease are not very specific. Blood tests are used to evaluate pancreatic enzyme levels, blood sugar levels, and liver and kidney function.
The stool may also be tested for enzymes and fat. Imaging studies of the pancreas are performed using computed tomography, radiography, magnetic resonance cholangiopancreatography, and transabdominal ultrasound (ultrasound).
Causes of the disease
Numerous factors can provoke an exacerbation of chronic pancreatitis. These include concomitant diseases, nutritional errors and external negative influences. In most cases, the provoking factor is a violation of the recommended regimen (uncontrolled use of medications, premature termination of therapy, lack of diet control).
Infections and progressive pathologies of other digestive organs can aggravate the patient's condition. Inflammatory processes instantly affect the functioning of the weakened pancreas.
Reasons for exacerbation:
- abuse of bad habits (drinking alcohol will almost instantly provoke pain and exacerbation of the inflammatory process);
- violation of nutrition and diet (prolonged fasting, overeating, non-compliance with food temperature, consumption of prohibited foods);
- consequences of taking certain medications (drug overdose, taking medications that have a negative effect on the pancreas, uncontrolled drug therapy);
- complications of infectious processes in the body (diseases do not necessarily have to be associated with the digestive system);
- progressive pathologies of the biliary system (cholecystitis, cholangitis, cholelithiasis);
- complications of diseases of the digestive tract (gastritis, peptic ulcer);
- negative consequences of stressful situations and psycho-emotional stress (the nervous system is interconnected with the functioning of the digestive organs, stress can promptly provoke an attack of pancreatitis).
Prevention is easier than cure
How to cure pancreatitis forever? To avoid such questions, you should take care of your health. It is better to prevent a disease than to treat it. It is worth sticking to the main points:
- Varied food. A rich diet will help protect against such illness and provide the body with all the necessary vitamins and minerals.
- Avoid eating fatty, fried and spicy foods. Of course, it’s difficult to refuse something fried. And you shouldn’t forever deprive yourself of the opportunity to eat spicy food. You just shouldn’t overuse it, and then the pancreas will say “Thank you.”
- No fast food. It has already been proven all over the world that eating fast food threatens obesity, the formation of cholesterol plaques in blood vessels, heart problems, etc.
- We try to avoid overeating. It is better to eat little and often than to eat heavily and rarely.
- We try not to be nervous and avoid stressful situations. Any exciting incident affects the entire human body. The internal organs take an emotional blow, which can cause the pancreas to become inflamed.
- We limit alcohol consumption.
People who are undergoing medical therapy and using antibiotics or hormonal drugs must constantly monitor their health. Taking such potent drugs can leave a mark on any of the internal organs.
Signs of exacerbation of pancreatitis
An attack of pancreatitis always begins with the onset of acute pain localized in the left hypochondrium. The pain syndrome intensifies in the absence of drug therapy. The pain may become wandering in nature and spread to the back, lower back, and shoulder blades. Painful symptoms are gradually joined by other signs of exacerbation of the inflammatory process.
Signs of development of exacerbation of pathology:
- characteristic pain after eating prohibited foods (fatty, fried, salty foods, alcohol, etc.);
- pain decreases if the patient assumes the fetal position or tilts the torso forward;
- pain occurs after taking enzyme medications (such medications increase the inflammatory process and enzyme activity of the pancreas).
Is it possible to get rid of pancreatitis once and for all?
Unfortunately, chronic pancreatitis is a pathology that cannot be cured completely and forever. After the first manifestation of the disease, you will have to give up your usual way of life.
To prevent the development of pain syndrome, you will have to think about what you eat throughout your life. The disease forces you to give up drinking alcoholic beverages, fast food, smoked delicacies and many other foods.
Fast food, coffee, cola, alcohol will have to be forgotten forever
You need to understand that any inflammatory process does not pass without a trace for the body. And, having manifested itself once, inflammation will manifest itself again - in an aggravated form. This can happen even after a course of properly selected therapy.
For this reason, it is difficult to talk about a complete cure for pancreatitis. The insidiousness of the disease and the difficulty of diagnosing it at an early stage force patients to change their usual lifestyle once and for all.
Symptoms and treatments
A distinctive feature of exacerbation of chronic pancreatitis is pain with unclear localization. An attack can be determined by the presence of additional symptoms. Inflammation of the pancreas is accompanied by a number of abnormalities in the general condition of the body, the process of bowel movement and food digestion.
If an exacerbation occurs against the background of a violation of the diet, then the consequence will be heartburn (with other provoking factors, this symptom may be absent).
Other symptoms:
taste of bile in the mouth;- uncontrollable vomiting;
- regular nausea;
- lack of appetite;
- yellowness of the sclera;
- dry mouth;
- diarrhea;
- particles of undigested food in the stool;
- decreased blood pressure;
- increased body temperature;
- chills and general weakness of the body.
Medical indications
Symptoms of exacerbation of pancreatitis include a number of abnormalities in the functioning of the internal systems of the body. The main factors indicating the progression of the inflammatory process are dull pain of different localization and diarrhea (particles of undigested food are present in the stool). The clinical picture is complemented by additional symptoms characteristic of pancreatitis.
Other medical indications:
- progressive weight loss;
- constant lack of appetite;
- a feeling of bitterness in the mouth;
- coating on the tongue;
- severe dyspepsia;
- regular vomiting of bile.
Diagnostic methods
A gastroenterologist diagnoses exacerbation of pancreatitis. At the first stage of the examination, the doctor collects an anamnesis. The patient is required to undergo general and biochemical tests (blood, urine, feces). A coprogram must be carried out (particles of undigested food must be present in the stool).
Instrumental diagnostic methods depend on the individual characteristics of the patient’s body and the severity of pain symptoms.
Other diagnostic methods:
- gastroscopy;
- radiography;
- Ultrasound;
- CT or MRI;
- LUNDT test;
- pancreatin level test;
- analysis for calcium and lipids;
- determination of blood glucose levels.
Prescribing home therapy
Home therapy for exacerbation of pancreatitis includes following a number of recommendations. For the first days after an attack, food intake should be avoided, the patient is provided with rest, and any physical activity is unacceptable. Pain relief in most cases occurs in a hospital setting. After discharge, the patient is given an individual course of therapy.
Home treatment includes:
- dieting (Diet 5p);
- course intake of prescribed medications;
- eliminating bad habits;
- addition to basic therapy with folk remedies.
Therapy in a hospital setting
Inpatient treatment involves special procedures to restore the functioning of the digestive system, prescribing medications, providing dietary nutrition and stopping an attack.
Hospitalization is a mandatory measure if the patient has complications or concomitant diseases.
Methods of treatment in a hospital setting:
- replenishment of water balance and nutrients in the body (intravenous administration of special solutions);
- prescription of drugs to ensure functional rest of the pancreas (blockers of various receptors, enzyme agents, antacids, etc.);
- prevention of complications using antibiotics (cephalosporins, penicillins);
- physiotherapeutic procedures (electrophoresis, sinusoidal modulated current).
How does pancreatitis manifest?
Inflammation of the organ is accompanied by symptoms that echo signs of serious poisoning. In pancreatitis, enzymes remain in the pancreatic ducts or in the organ itself and destroy it from the inside. In addition, they are absorbed into the blood, which leads to the development of intoxication of the body.
So, how does pancreatitis manifest? The following signs can be identified:
- Severe pain always accompanies inflammation of the gland. They torment the patient on a constant basis, their character is cutting or dull. The pain can be so severe that it can provoke a painful shock. Their location is the right hypochondrium or left hypochondrium, or an area located slightly below the middle edge of the sternum. The exact location of pain depends on which part of the organ is affected by inflammation. If the entire gland is inflamed, then the pain is girdling in nature.
- Increase in body temperature, drop or increase in blood pressure. The more intense the inflammation, the worse the patient will feel. Body temperature rises to high values, and blood pressure surges are possible.
- Change in skin color on the face. Firstly, the patient’s facial features become sharper. Secondly, the skin turns pale and then completely becomes earthy gray.
- The occurrence of vomiting. After the vomit comes out, the patient does not experience a feeling of relief. The masses themselves contain undigested food, and subsequently bile masses. In this regard, fasting is an important point in the treatment of inflammation, which lays the foundation for further successful recovery.
- Nausea and hiccups. In addition, belching and dry mouth may occur.
- Formation of constipation or development of diarrhea. Most often, the acute phase is accompanied by the appearance of foamy, foul-smelling stools containing food particles. Constipation is often the first sign of inflammation; in parallel, the patient experiences hardening of the abdominal muscles and bloating.
- The appearance of shortness of breath. This symptom is formed due to the loss of electrolytes during vomiting. A person develops sticky sweat and a large amount of yellow coating forms on the tongue.
- Bloating. Stopping the work of the intestines and stomach leads to bloating, which is diagnosed by the doctor during palpation.
- The appearance of bluish spots. They occur mainly in the lower back and around the navel. In this case, the skin appears marbled, and in the groin area it may turn blue-green. The reason for this condition is the penetration of blood from the inflamed organ under the skin.
- Yellowing of the skin and sclera of the eyes. If sclerosing pancreatitis occurs, the patient develops obstructive jaundice. It is formed against the background of compression of the bile duct by an inflamed organ.
If a patient exhibits signs of acute pancreatitis, his condition will quickly deteriorate. This is why it is so important to seek medical help immediately.
The same signs that appear in both acute and chronic (during exacerbations) forms of pancreatitis are acute, severe pain in the abdominal area. Localization depends on which part of the pancreas is affected by the inflammatory process.
The main components of the pancreas are: head, body and tail. If the process began in the head of the gland, then acute pain occurs in the right hypochondrium; if the body is affected, then pain is noted in the epigastric region, and pain in the left hypochondrium indicates the development of inflammation in the tail. If the process covers the entire gland, then the pain syndrome is of a girdling nature and can radiate to the back, behind the sternum, or to the scapula.
Pain syndrome in acute inflammation of the pancreas is considered one of the most severe. Acute, sharp pain that occurs in the abdomen or hypochondrium tends to spread to the back, to the area of the shoulder blades and behind the sternum.
In the acute form, as a rule, stool disturbances from diarrhea to constipation are observed. Most often, patients note mushy stools with impurities of undigested food and an unpleasant odor.
How long does it last
The pancreas is not able to quickly recover during the inflammatory process. This nuance explains the long period of exacerbation of pancreatitis. Intense pain symptoms can last up to two weeks (the average is from five to seven days). The situation can be aggravated by the lack of adequate therapy and poor diet. Restoration of the functional state of the digestive organs in this case will be slow or completely absent (progression of complications). The sooner treatment begins for exacerbation of pancreatitis, the shorter the duration of the attack.
First aid
If pancreatitis worsens, the patient must call an ambulance. Before the brigade arrives, a number of actions should be taken to alleviate his condition. It is important to provide three factors - cold, hunger and peace. The patient should be in a horizontal position. You can apply a cold compress to the source of pain (left hypochondrium). Eating any type of food is strictly prohibited.
Following these recommendations will help reduce the intensity of pain and slow down the progression of the inflammatory process.
How to relieve an aggravation
Patients diagnosed with chronic pancreatitis, in most cases, can independently determine the onset of exacerbation of the pathology. If alarming symptoms occur, you should begin to relieve them as soon as possible. First of all, the diet is adjusted. If the attack is intense, then the body is provided with fasting for a maximum of two days. If the exacerbation is mild, the menu is adjusted taking into account dietary rules (excluding all harmful foods).
Kvass on celandine according to Bolotov
Kvass, created according to the recipe of the scientist B.V. Bolotov, is a medicinal product prepared from whey, celandine and sugar. It has anti-inflammatory and cleansing properties. The celandine contained in the composition contains a lot of useful substances: essential oils, flavonoids, vitamins, organic acids, saponins, bitterness, about 20 alkaloids - toxic compounds that, under the influence of serum enzymes, undergo a fermentation process and are transformed into useful substances.
Kvass has a bactericidal effect, it destroys the pathogenic environment and promotes the renewal of tissues of the gastrointestinal tract, blocks inflammation, and eliminates pain. It is used with great success to treat prolonged chronic pancreatitis. In addition to its beneficial effects on the digestive system, its positive effect is invaluable in cases of nervous disorders, heart ailments, dysbacteriosis, skin diseases, tuberculosis, and myopia. The ability to renew cells and suppress the development of pathogens allows Bolotov’s kvass to be used for the treatment of oncology, increasing immunity, and healing wounds and ulcers.
Kvass recipe
A properly prepared drink has a pleasant taste and a bitter-sour smell, reminiscent of grapefruit and apple.
Ingredients for kvass:
- Whey or purified water - three liters.
- Natural sour cream no more than 15% fat - one teaspoon.
- Granulated sugar - one glass.
- Dry celandine herb – 25 grams (half a glass) or a glass of fresh herb.
Pour whey (water) into a three-liter jar, add sugar and sour cream. Place the celandine herb in a gauze bag folded in three or four layers (the gauze must be sterile), where a load is placed, for example, made of stone, glass or stainless steel; any cutlery can do. The bag with the weight and grass is tightly tied and dropped to the bottom of the jar. The neck of the jar should be covered with gauze, secured and put in a dark, warm place. Kvass takes 14 days to prepare, during which mold should be removed from its surface daily and stirred.
On the fifth day, when sediment appears at the bottom of the dish (it is thrown away), the top layer of kvass is poured into another three-liter jar, a bag of grass is transferred there and water is added to the brim. After the tenth day, the drink begins to foam; this is a normal reaction of properly prepared kvass. On the fifteenth day, a liter of the finished infusion is poured from the jar, it is put in a cool place for consumption, and water or whey is added to the remaining kvass to bring it to the previous volume.
In this way, the drink can be diluted four times. Next, fresh kvass is prepared according to the same procedure, having previously washed the container where the fresh product will be placed.
Method of treatment
Treatment of pancreatitis begins with a minimum dosage - a tablespoon three times a day 30 minutes before meals. If no negative effects in the form of bradycardia, nausea, or allergic reactions are observed within seven days, you can increase the dosage to one hundred milliliters three times a day and continue to drink the drink for another three weeks. To consolidate the results of treatment, it is recommended to extend the use of kvass for another month, taking half a glass once a day. This method of treatment helps to get rid of acute pain and nausea.
What to do if pancreatitis worsens
Exacerbation of pancreatitis implies the implementation of a certain algorithm of actions. The tendency to recovery and the effectiveness of further therapy depend on compliance with the recommendations. Ignoring the symptoms of an attack in some cases can cause the death of the patient (for example, if pancreatitis develops over a long time and provokes purulent formations, local death of digestive tissue and other complications).
Algorithm of actions for exacerbation of the inflammatory process:
- stopping an attack in accordance with the rules (first aid, calling a team of specialists);
- fluid replenishment (water, alkaline mineral water);
- resting the pancreas by fasting (maximum three days);
- compliance with diet and taking prescribed medications.
Triple tincture to stimulate insulin production
You can improve the functioning of the pancreas and insulin production with a remedy consisting of three tinctures:
- Grind 100 grams of onions until mushy. Pour in 600 milliliters of vodka. Place the product in a dark place for five days. Before use, the infusion must be strained.
- Pour 100 grams of crushed walnut leaves with 600 milliliters of vodka. Leave in a dark place for seven days, then strain.
- Crushed mantle grass in the amount of 60 grams is poured with 600 milliliters of vodka, infused for a week, and filtered.
Next, you need to prepare a medicine based on the three listed tinctures: 150 milliliters of onion tincture, 60 milliliters of nut leaf tincture, 40 milliliters of mantle tincture. The finished medicine is taken one tablespoon before bedtime and 20 minutes before breakfast.
On the subject: Treatment of pancreatitis with oatmeal jelly
Treatment
Exacerbation of pancreatitis requires complex treatment. The main method is a combination of drug therapy and diet. The patient will have to take certain medications and adjust the diet for a long time. Violation of the recommendations will shorten the period of remission and increase the severity of the next attack.
It is permissible to supplement therapy with some folk remedies, but only after agreeing with the attending physician.
Medicines
If pancreatitis is detected, the patient is prescribed certain drug therapy. Additionally, the doctor gives recommendations on the choice of drugs that will help stop the exacerbation of the pathology. Incorrectly selected medications will not only not eliminate the symptoms of the inflammatory process, but can also provoke serious complications.
Examples of medications:
non-narcotic analgesics (Paracetamol, Analgin);- agents to suppress secretion (Octreotide, Somatostatin);
- proton pump inhibitors (Omeprazole);
- prokinetics (Motilium);
- antispasmodics (No-Shpa, Drotaverine);
- preparations with enzymes (Creon);
- antienzyme agents (Gordox);
- anticholinergics (Methacin, Atropine).
Diet
For chronic pancreatitis, diet is an essential part of therapy. Correcting the diet helps prolong the period of remission and speed up the process of restoring the functional state of the digestive tract. In case of exacerbation of pathology, the diet has healing properties.
Thanks to a certain diet, you can relieve pain, eliminate additional symptoms of an attack and increase the tendency to recovery.
Basic principles:
- at the time of an exacerbation attack and in the first days after its relief, the patient is recommended to undergo therapeutic fasting (only alkaline mineral water and rose hip decoction are allowed);
- after fasting, nutrition is resumed gradually (for 5-7 days, only slimy porridges and soups should be present in the diet);
- expansion of the diet is permissible from the tenth day after the onset of an attack (only if there is a tendency to recovery);
- All types of products and dishes that can harm the digestive system are excluded from the menu (fatty, salty, spicy, fried foods, vegetables with coarse fiber, sour fruits and berries, seasonings, legumes, mushrooms, rich broths, sweet pastries, etc.);
- the menu is compiled on the basis of a list of permitted products (lean meats and fish, vegetarian soups, cereals, dairy and fermented milk products, non-acidic berries and fruits, some types of vegetables - potatoes, zucchini, carrots, squash);
- The diet must comply with the principles of the 5p Diet (fractional meals, gradual expansion of the menu, exclusion of overeating and starvation).
Traditional methods
Traditional medicine for exacerbation of pancreatic inflammation can only be used at the stage of restoring the diet. A good addition to the main therapy is rosehip decoction. The drink is recommended for a therapeutic diet and has a number of beneficial properties for the digestive system. It is recommended to consult your doctor in advance for other folk remedies.
Ingredients for preparing medicinal decoctions:
- chamomile;
- immortelle;
- barberry bark;
- calendula;
- yarrow;
- St. John's wort;
- sage.
The principle of preparing decoctions is not complicated. A teaspoon of the dry mixture is poured into a glass of boiling water and infused for thirty minutes. You can combine several ingredients in decoctions. You can use such drugs not only in the treatment of pathology, but also to prevent exacerbations. In addition to decoctions, other folk remedies are also used in the treatment of pancreatitis.
Examples of folk remedies:
- potato juice (the juice should be consumed fresh, the daily norm is 50 ml);
- buckwheat with kefir (grains are filled with fermented milk product, infused overnight and consumed in the morning for breakfast);
- oatmeal jelly (oatmeal should be soaked in water for thirty minutes, the cereal should be filled with water and cooked for an hour, you should get a mass of thick consistency).
What to eat when the exacerbation passes?
An exacerbation of chronic inflammation of the gland is dangerous because it leaves a scar after a painful period. With the frequent appearance of such scars, the connective tissue of the organ that performs digestive functions is preserved less and less. Therefore, over time, the quality of digestion seriously deteriorates.
To slow down this process and reduce the likelihood of relapse, it is also necessary to follow a dietary regimen. According to it, all dishes can only be boiled, baked, cooked in a double boiler and a slow cooker. The optimal intake for this period of time would be five or six meals daily.
The list of permitted foods for chronic diseases includes:
- dried white bread, uneatable crackers;
- pasta;
- vegetable purees and pureed soups;
- dairy products;
- egg whites (up to one yolk per day is allowed);
- vegetable oil (in limited quantities);
- cereals (preferably pureed, crushed);
- non-acidic fruits;
- meat (containing large amounts of iron), chicken and fish without fat;
- freshly squeezed juices, compotes.
To determine the nutritional value of foods, you can use a table from a cookbook. You should eat small portions of one hundred to two hundred grams. The last meal should take place no later than two to three hours before bedtime, and too long intervals should not be allowed. The optimal time between meals is three to four hours.
Prevention
Prevention of exacerbation of pancreatitis includes several important points. Firstly, following a diet will ensure restoration of the digestive system and long-term remission. Secondly, taking prescribed medications will improve the functional state of the pancreas. Thirdly, eliminating factors related to the causes of exacerbation of pathology will reduce the risk of recurrent attacks to the maximum extent.
Other preventive measures:
- regular intake of vitamin complexes;
- rejection of bad habits;
- elimination of excessive emotional and physical stress;
- compliance with the rules of a healthy lifestyle.
Video on the topic: Effective treatment of the pancreas without drugs or with drugs.
Medications
In case of acute form or relapse of chronic form, drug treatment cannot be avoided. It can be carried out both at home and in a clinic. Therapy includes the use of drugs from several groups:
- antispasmodics – relieve pain, usually used no more than a week after an exacerbation;
- mathematical agents - the most effective are Pentoxyl, Methyluracil;
- enzyme preparations - doctors often prescribe imported ones, such as Mezim; an available domestic analogue, which is no less effective, is Pancreatin;
- vitamin complexes.
Antibiotics are almost always prescribed; they are selected by the attending physician on an individual basis. Typically, broad-spectrum drugs are prescribed: Ceftriaxone, Amoxiclav, Abactal.
Thus, you can cope with any form of pancreatitis at home if an attack of pain is diagnosed in time. To prescribe medications, you must consult a doctor; therapy can be supplemented with the use of traditional recipes.
Forecast
Prognosis for exacerbation of the inflammatory process depends on the timeliness of therapy and compliance with the doctor’s recommendations. If the patient ignores the symptoms of an attack, the consequences can lead to death (peritonitis, sepsis) or a significant decrease in quality of life. In chronic pancreatitis, remission can reach several years, but only with adequate therapy and compliance with preventive measures.
Complications of the inflammatory process:
- renal failure;
- pancreas cancer;
- encephalopathy;
- internal bleeding;
- abscesses;
- death.
Recommendations for treating pancreatitis at home
Chronic pancreatitis has less severe symptoms than the acute form of the disease. Long-term remissions may cause patients to discontinue therapy. The consequence of violating the schedule for taking medications and diet will be an exacerbation of the inflammatory process. If pancreatitis is detected, then home treatment and prevention of the disease must be carried out regularly.
Recommendations for home treatment:
- You should take vitamin complexes and medications to protect the pancreas regardless of attacks (exacerbations are easier to prevent than to deal with their manifestations);
- You cannot independently select medications for symptomatic treatment (taking some medications can provoke a sudden attack of the disease);
- even minimal but regular deviations in the functioning of the digestive tract should be a reason to consult a doctor;
- experiments with nutrition during pancreatitis are unacceptable (spicy, salty or fatty foods can cause not only an attack, but also complications in the form of gastrointestinal bleeding).
Results
- exacerbation of pancreatitis can develop in a latent form or in the form of a sudden attack;
- in case of exacerbation of the pathology, the patient must be provided with qualified medical care;
- during an attack, food consumption is excluded (therapeutic fasting for two or three days);
- in the presence of complications, pain may persist for two weeks;
- After the attack has stopped, nutrition is resumed gradually;
- The basis for creating a menu is the principles of the 5p Diet.
List of prohibited products
Any heavy food (especially store-bought) should be excluded from the patient’s diet. In addition, semi-finished products and fast food are prohibited. Among the main restrictions are also:
- rich meat and fish broths;
- pickled products;
- smoked meats and pickles;
- legumes;
- mushrooms;
- onions, radishes and garlic (especially fresh);
- high fat dairy products;
- fatty meat and fish products;
- alcohol in any form;
- sweets, confectionery;
- sausage products;
- fresh baked goods and bread;
- sauces (especially tomato and mayonnaise);
- carbonated drinks, strong tea and coffee;
- very sour or sweet fruits.
Even dietary foods can be banned if processed incorrectly. Adding too much salt and seasoning is also prohibited.
Preparations for restoring intestinal microflora
An imbalance in the ratio of normal and pathogenic bacteria in the intestines is observed in almost all patients with chronic pancreatitis. This is explained by a lack of enzyme secretion and increased fermentation processes, which creates a favorable environment for the proliferation of pathogenic microflora.
To eliminate this phenomenon, the following are sometimes prescribed:
- Intestinal antibiotics: Enterofuril (Stop-diar) , Rifaximin (Alfanormix). Or Ciprofloxacin, course for up to 7 days.
- Then - probiotics and prebiotics containing normal beneficial bacteria. These include: Baktistatin, Enterol, Linex, Bifiform, Floristin, Normobact, etc. They are taken during or after meals in courses of up to 3 weeks.