Many people constantly confuse acute respiratory infections and acute respiratory viral infections.
These are different diagnoses: ARVI is a viral infection, and acute respiratory infection is a disease that can be caused not only by viruses, but also by other pathological microorganisms, including bacteria, fungi, etc.
Let us further consider possible pathologies, acute respiratory infections, its symptoms and treatment in adults, ways to maintain the immune system and good human health.
What is ORZ?
ARI is a collective concept that characterizes all possible diseases of the respiratory tract - viral, viral-microbial and purely microbial, as well as those caused by intracellular parasites.
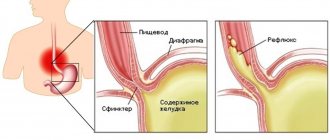
A distinctive feature of all acute respiratory infections are symptoms that indicate damage to the epithelium of the upper respiratory tract. It is here that the accumulation of pathogens, their primary deposition and reproduction occurs. In the future, the activity of viruses leads to the development of inflammatory processes and all kinds of complications associated with disruptions in the functioning of vital systems of the body.
Every year in our country, up to 40 million people suffer from acute respiratory diseases. For rhinovirus infection, the so-called. The “gates of entry” are the mucous membranes of the nose and conjunctiva. According to statistics, an adult suffers more or less severe acute respiratory disease on average 2-3 times a year.
This group of diseases manifests itself seasonally - more often pathologies occur when the seasons change (in the autumn-winter period). It is important to take timely measures to prevent acute respiratory infections so as not to become infected in the midst of an epidemic.
ARI has a synonym - ARI, or acute respiratory infection. In common parlance, acute respiratory infections are usually referred to by the more familiar word “cold.” Also, in connection with colds and flu, you can often hear the abbreviation ARVI.
Features of the development of acute respiratory infections
Often, it is quite problematic to separate acute respiratory infections and acute respiratory viral infections without complex methods of clinical laboratory diagnosis, only by external signs, among which the most pronounced can be considered:
- Manifestations of a runny nose (rhinitis);
- External discharge of serous (liquid) secretion;
- Swelling and redness of the nasal mucosa;
- Maceration of the surface of the nasal cavity (swelling of the epithelium as a result of its contact with liquid secretions) and the subsequent appearance of microwound surfaces and cracks in the cavity and at the base of the skin of the nose;
- Cough.
The cause of a runny nose is:
- Reduced resistance of the body under the influence of allergens (dust, smoke, gas and aerosols);
- Weakening of local resistance, as a result of hypothermia of the extremities or the whole body (cold).
Against the background of a cold, the pathogenic activity of opportunistic microflora of the nasal cavity (for example, staphylococci and streptococci), as well as a specific viral infection, is activated.
The actual causes of a runny nose trigger a reflex of the nasal mucosa to irritation. It has been proven that, for example, the cold factor acting on the back area is a trigger for the development of catarrhal runny nose. Hypothermia of the lower back causes a sharp constriction of the blood vessels of the kidneys, which affects daily filtration and urine output.
Damage to the nasal mucosa and cough are the most typical signs of inflammation. The symptoms of rhinitis can be divided into three distinct stages:
1. The dry stage of irritation, which begins at the earliest stage of the development of the disease and is accompanied by the following symptoms:
- dryness and redness of the mucous membrane;
- there is a burning sensation in the nose;
- feeling of nasal congestion;
- developing edema caused by swelling of the mucous membrane of the nasal passages;
- narrowing of the nasal passages.
This period is not characterized by a rise in temperature to noticeable values, so it may not be noticed. The sense of smell deteriorates and the acuity of taste decreases (respiratory hyposmia). This condition may continue at the beginning of the disease, less often for two days.
2. The stage of serous discharge, which is characteristic of the first day of the disease, when abundant transudate (liquid effusion) is observed. Subsequently, the transudate thickens due to an increase in the content of the protein fraction produced by glandular epithelial cells. The secretions increase the content of sodium chloride molecules and ammonium ions, which cause irritation (itching) of the mucous membrane and skin. Redness and swelling spread to the skin at the base of the nose and to the upper lip. By the end of this stage, as a rule, the feeling of dryness and burning disappears, but lacrimation occurs and it becomes impossible to breathe through the nose. A characteristic closed nasal tone appears in the voice.
3. Mucopurulent stage of discharge, which appears on the 4th day of illness. This period is characterized by the appearance of viscous and then thick discharge, which at the beginning of this stage is yellow and then green. The color of the discharge depends on what cells and in what quantity are included in the composition of this discharge. These are mainly leukocytes, lymphocytes and rejected epithelial cells. The appearance of green mucus indicates that the acute stage is ending.
It should be remembered that signs of swelling of the nasal cavity appear not only under the influence of infection, but also as a reflex reaction to hypothermia or an allergen.
During the reflex reaction the following is observed:
- Increased blood flow;
- The vessels dilate and become permeable to the liquid part of the blood;
- Exudation of serum, followed by the formation of transudate (liquid secretion) and exudate (thick secretion);
- Decreased resistance of the nasal mucosa.
These reasons violate local immunity and lead to the proliferation of viruses or bacteria that are part of the microflora, as well as foreign microorganisms entering the respiratory tract as part of the inhaled air.
The occurrence of cough is an indicator of the development of inflammation and the entry of mucous effusion into the underlying respiratory sections. The physiological cause of cough is a reflex reaction, the stimulus for which is irritation of receptors located in the mucous membrane of the larynx, trachea and large-caliber bronchi. The main irritant that causes coughing is thickened mucus flowing towards the lung tissue. Externally, cough is manifested by infrequent coughing, repeated jerking movements of the chest associated with contraction of the intercostal muscles and diaphragm. At the beginning of the disease, the cough is usually dry (without sputum), but after a couple of days, with increased mucus secretion and the formation of mucopurulent exudate, it becomes wet.
Causes
Viruses that cause acute respiratory infections infect the mucous membrane of the respiratory tract. An inflammatory process develops in the underlying tissue. Toxic products of viruses act on various parts of the nervous system. The severity of the disease is related to the virulence of the virus and the state of the patient’s immune system. A viral infection causes a decrease in immunity, which contributes to the addition of a secondary bacterial infection and the appearance of complications.
Depending on the involvement of various parts of the respiratory tract in the process, the following are distinguished:
- ARI of the lower sections with localization of the process below the level of the vocal cords - laryngitis, bronchitis, tracheitis;
- Acute respiratory infections of the upper sections - rhinitis, sinusitis, pharyngitis and tonsillitis.
The main causes of the development of diseases from this group are more than 200 different viruses:
- rhinovirus;
- flu;
- adenovirus;
- parainfluenza;
- RS virus;
- picornavirus;
- coronavirus;
- Bocaruvirus and others.
Let's look at the main factors that lead to weakened immunity in adults:
- hypothermia of the body;
- lack of vitamins and microelements necessary for its normal functioning, especially vitamin C (ascorbic acid);
- stress, mental overstrain;
- unfavorable environmental conditions in places where people frequently stay - gas pollution, dust, fungi on the walls, etc.;
- the presence of untreated chronic diseases in the body.
Classification of acute respiratory infections
Depending on the type of pathogen, the following types of acute respiratory infections are distinguished:
- adenoviral infection - manifested by symptoms of conjunctivitis (photophobia, sensation of a foreign body in the eyes, pain, lacrimation, redness);
- rhinovirus infection is most often a common cold, which is easy and goes away quite quickly without causing significant harm to the body;
- Corona virus infection also occurs like a cold and does not require special treatment;
- parainfluenza - the main symptom is a dry barking cough.
Incubation period
Infection of acute respiratory infections in adults occurs by airborne spread of the pathogen from a sick person or carrier to a healthy person. The main site for the replication of the acute respiratory viral infection is the epithelial cells of the respiratory tract, as a result of which thousands of virions appear, which spread over a long distance, accompanied by necrotization and desquamation of the surface layers of the mucous membranes of the respiratory tract.
The incubation period, i.e. the time between contact with a patient and the onset of the disease lasts from 12-48 hours for influenza to 1-14 days for other acute respiratory infections. The pathogen penetrates through the upper respiratory tract, fixes on the mucous membranes and multiplies, damaging the mucous membranes. In this case, the primary signs of acute respiratory infections appear - swelling and inflammation in the nose and throat.
A person becomes a carrier of the disease when the pathogen enters his body. Adults are carriers of the disease even during the hidden incubation period, without knowing it. The threat extends not only during these periods of illness; infection occurs throughout the illness until the presence of rhinitis, cough or fever decreases.
How is the treatment carried out?
Acute respiratory viral diseases are treatable. The best results are achieved with an integrated approach and early exposure to the pathogen. In typical cases, the pathology begins with a feeling of discomfort, sore nose and throat, sneezing, and runny nose. Gradually, the intensity of symptoms increases, manifestations of intoxication occur, body temperature rises, and a nonproductive cough appears.
The basis for diagnosing acute respiratory infections is the clinical picture. To establish the type of inflammatory process and the nature of the pathogen, laboratory tests are used. If the pathology is of microbial origin, tests will confirm leukocytosis. With a viral infection, lymphocytosis appears. If there is severe wheezing in the lungs, a chest x-ray is indicated. It eliminates pneumonia.
Diagnosis and treatment of the disease is provided by a therapist, family doctor, pediatrician (if an acute respiratory infection occurs in a child). If complications develop from the ENT organs, consultation with an otolaryngologist is indicated. If conjunctivitis occurs, the help of an ophthalmologist is necessary. The duration of treatment is from 7 to 14 days. You should not resort to self-medication or use alternative medicine; such actions can lead to serious complications.
Treatment of acute respiratory infections consists of eliminating symptoms and increasing the body's immunity. The use of such means is shown:
- antipyretic drugs;
- anti-inflammatory drugs;
- sprays for sanitizing the nasal cavity and facilitating breathing;
- antitussives or expectorants;
- vitamins.
The dosage of medications and the regimen of use are determined by the doctor. Clinical recommendations for acute respiratory infections include bed rest, proper rest, and drinking plenty of fluids.
Symptoms of acute respiratory infections in adults
Typically, the first symptoms of acute respiratory infections appear 2-3 days after infection, but deviations from these figures are also possible. Thus, in weakened people, elderly people and children, the first signs of the disease may appear a few hours after contact with the patient.
An acute respiratory disease begins with discomfort and unpleasant sensations in the nasopharynx and throat. Sneezing, runny nose, malaise, weakness, dizziness and headaches also appear.
In the first stages of the disease, the temperature usually remains within normal limits or rises slightly. Nasal discharge appears 2-3 days after the onset of the disease and is watery in nature.
Signs of acute respiratory infections in adults appear as follows:
- General weakness.
- Painful sensations in the head.
- Chills.
- Aches in muscles and joints.
- Raising body temperature to 37.5 degrees.
- Decreased appetite.
- Runny nose.
- Sore throat, pain and cough.
Symptoms that indicate a severe course of the disease or the development of possible complications of acute respiratory infections:
- the disease does not go away within two weeks;
- temperature rise above 40 degrees. Taking antipyretic drugs does not have the desired effect;
- chest pain;
- cough that produces brown, green, or red sputum;
- severe headaches;
- confusion;
- pain in the chest during breathing;
- the appearance of spider veins on the skin.
In most cases, the above symptoms are accompanied by conjunctivitis, headaches, muscle and joint pain, inflammation of the lymph nodes, hoarseness or “shooting” pain in the ears.
Fever with acute respiratory infections in most cases begins with chills or chills. Body temperature already reaches its maximum level on the first day (38-40 °C). The duration of fever varies depending on the etiology of the disease and severity.
These symptoms occur not only with acute respiratory infections, but also with acute respiratory viral infections and influenza. It is quite difficult to diagnose the disease yourself, since colds have similar symptoms.
One type of acute respiratory disease is influenza. The manifestations of the disease with this virus are strikingly different from other acute respiratory infections. Influenza is characterized by a sudden onset of the disease with the following symptoms:
- high temperature (up to 39-40 degrees), persisting for 3-4 days;
- pain and pain in the eyes;
- intoxication of the body (eye reaction to light, sweating, weakness, dizziness);
- mild nasal congestion, sneezing.
Important: Acute bronchitis and bronchiolitis can also be considered as manifestations of acute respiratory infections, but only if these pathologies are accompanied by damage to the upper respiratory tract.
As soon as the first signs of acute respiratory infections appear in adults (runny nose, pain or just discomfort in the throat), you need to respond to them immediately. Coping with the disease at the very beginning is easier than treating numerous complications from an infection that has penetrated “deeply.”
As a rule, acute respiratory disease lasts for 6-8 days and goes away without consequences if it is treated correctly.
Brief characteristics of pathogens of acute respiratory infections
The development of acute respiratory infection occurs due to bacteria and viruses belonging to various families and genera, as well as mycoplasmas and chlamydia. Possible combinations in the form:
- Virus-virus infection,
- Virus-bacterial infection,
- Virus-mycoplasma infection.
The clinical picture of such forms of acute respiratory infections may have similar manifestations with varying severity of the disease and spread of infection.
The greatest contribution to the overall incidence of acute respiratory infections is made by a viral infection, which is caused by:
- Influenza viruses;
- Adenoviral infection;
- Parainfluenza virus;
- Rhinoviruses;
- Coronaviruses;
- Respiratory syncytial viruses.
Damage to local immunity and the development of inflammation of the respiratory organs can provoke further development of bacterial:
- Streptococcal infection;
- Staphylococcal infection;
- Pneumococcal infection (causes “typical pneumonia”);
- Respiratory mycoplasmosis and chlamydia.
The influenza virus, depending on the season and the prevalence of a particular type, can make a 20-50% contribution to the overall incidence of respiratory diseases. It belongs to the family of orthomyxoviruses, the genome of which consists of RNA molecules, and is distinguished by the presence of neuraminidase and hemagglutinin molecules on its surface, which provide the antigenic variability of this virus. The most variable type A differs from the stable types B and C in that it very quickly changes structural properties and forms new subtypes. Viral particles have rather weak stability in warm climates, but are resistant to low temperatures (from -25 to -75 ºС). Warming and dry climate, as well as the effect of small concentrations of chlorine or ultraviolet radiation, suppress the spread of the virus in the environment.
Adenovirus infection is caused by DNA containing viruses of the same family, differing in genomic composition. Adenoviral infection can compete with the influenza virus in terms of incidence, especially in the group of children from 0.5 to 5 years old. The virus does not have high variability in terms of antigenic structure, but has 32 types, the 8th of which causes damage to the cornea and conjunctiva of the eye (keratoconjunctivitis). The entry gate for adenovirus can be the mucous membrane of the respiratory tract and intestinal enterocytes. Adenoviruses can persist in the environment for a long time; to disinfect the room, regular ventilation and mandatory treatment with a bleach solution or ultraviolet irradiation are required.
The parainfluenza virus belongs to the same family of myxoviruses as the influenza virus. At the same time, the infection it causes has a different course from influenza and has its own characteristic features. Parainfluenza contributes about 20% to acute respiratory infections in adults and about 30% to childhood morbidity. It belongs to the family of paramyxoviruses, the genome of which contains an RNA molecule, and differs from other viruses in the relative stability of the antigenic component. 4 types of this virus have been studied, which cause damage to the respiratory tract, mainly the larynx. A mild form of parainfluenza develops as a result of infection with a type 1 and 2 virus, which causes a sore throat, hoarseness and cough. The severe form develops when infected with a virus of types 3 and 4, accompanied by spasm of the larynx (laryngospasm) and severe intoxication. The parainfluenza virus is unstable and is quickly destroyed (up to 4 hours) in a well-ventilated area.
In the structure of viral respiratory infections, rhinoviruses account for 20-25% of morbidity cases. They belong to the picornovirus family, whose genome consists of an RNA molecule. The strains are able to actively reproduce in the ciliated epithelium of the nasal cavity. They are extremely unstable in the air and lose their ability to cause infection when left in a warm room for 20-30 minutes. The source of infection is virus carriers; rhinovirus spreads by airborne droplets. The gateway to infection is the ciliated epithelium of the nasal cavity.
Respiratory syncytial infection is caused by an RNA paramyxovirus, the distinctive feature of which is the ability to cause the development of giant multinucleated cells (syncytia) along the entire length of the respiratory tract - from the nasopharynx to the lower parts of the bronchial tree. The virus poses the greatest danger to infants in the first months of life, since it can cause severe damage to the bronchi of various sizes. A severe form of infection causes up to 0.5% mortality in the group of children under one year of age. By the age of three years, children develop stable immunity, so the incidence of respiratory syncytial infection rarely exceeds 15%. The virus is extremely unstable in the external environment.
Coronavirus infection accounts for 5-10% of cases of ARVI. Infection in adults is accompanied by damage to the upper respiratory tract; in children it penetrates deep into the bronchopulmonary tissue. Coronavirus is part of the family of pleomorphic viruses that contain an RNA molecule in their genome. Viruses are not resistant when in indoor air.
Complications
If an acute respiratory disease is not given a proper “response”, it can lead to the development of various more serious diseases:
- Sinusitis (the runny nose is accompanied by sinusitis, frontal sinusitis, ethmoiditis and sphenoiditis);
- Otitis;
- Meningitis;
- Tracheitis;
- Bronchitis;
- Pneumonia (pneumonia);
- Empyema of the pleura;
- Neuritis;
- Radiculoneuritis;
- Myocarditis;
- Viral encephalitis;
- Liver damage.
To prevent an acute respiratory disease from developing into consequences for the body, be sure to contact your doctor to prescribe treatment.
Acute respiratory infections - symptoms and possible complications
Since infections affect the upper respiratory tract, a number of acute respiratory infections symptoms can be identified that are characteristic of all types:
- sore throat;
- cough;
- hoarseness of voice;
- runny nose;
- feeling overwhelmed;
- muscle pain;
- temperature increase.
Some acute respiratory infections lead to enlarged lymph nodes, blockage of the bronchi, chest pain, the development of pharyngitis and pneumonia. If, upon diagnosis of acute respiratory infections, treatment was insufficient or not carried out at all, then patients risk facing serious complications. Most often infections lead to:
- clouding of consciousness;
- hemorrhages in internal organs;
- nosebleeds;
- damage to peripheral nerves;
- suffocation due to narrowing of the larynx;
- exacerbations of bronchial asthma;
- severe pain when swallowing food.
ARIs are especially dangerous during pregnancy, as they can threaten the health of the baby, cause irreversible changes in the fetus or premature birth.
Diagnostics
If you have or suspect the development of an acute respiratory infection, you should immediately seek advice from specialists such as a therapist or an infectious disease specialist. Additionally, the attending physician may prescribe the following diagnostic techniques:
- consultation with an ENT doctor;
- general blood analysis;
- immunological studies (particularly relevant when the disease is diagnosed in an infant or in children 2–6 years old);
- chest x-ray;
- If there is a suspicion of atypical infections, sputum culture is performed.
If the following symptoms appear, you should see a doctor immediately:
- The temperature remains above 38.5 °C for more than 2 days.
- The cough is accompanied by the discharge of purulent yellow-green sputum.
- Chest pain appeared when coughing or inhaling, shortness of breath, headaches, pain in the forehead, in the ear.
- It is imperative that people with chronic bronchitis or heart disease consult a doctor if acute respiratory infections occur.
Diagnosis of acute respiratory infections
The diagnosis of acute respiratory infections and acute respiratory viral infections is made based on the patient’s complaints, as well as survey and examination data. Typically, a characteristic clinical picture (catarrhal symptoms, fever) is sufficient reason to make an accurate diagnosis.
In some cases, laboratory diagnostic methods are prescribed to confirm the diagnosis:
- PCR, RIF - determine viral antigens in the nasal mucosa;
- serological methods (ELISA, RTGA, RSK) - are carried out to clarify the diagnosis in retrospect.
If complications of acute respiratory infections develop, consultation with a specialist (otorhinolaryngologist, pulmonologist) is necessary.
How to treat acute respiratory infections?
For the treatment of adult patients suffering from any etiopathogenetic form of acute respiratory infections, therapeutic, organizational, and hygienic measures are used, the effect of which is aimed at isolating the carrier of pathogens, reducing the activity of pathogen reproduction processes in the body, stimulating the individual protective capabilities of the patient, as well as relieving the main symptoms of the disease.
First, a few mandatory rules:
- Bed rest, at least for the first two days of the disease, in a ventilated room.
- If your body temperature does not rise above 38 degrees, you should not bring it down.
- Do not take antibiotics unless prescribed by your doctor. They are powerless against viruses. Their main strength is antibacterial.
- When body temperature rises above 37.5 degrees, thermal procedures are prohibited! May harm the heart and blood vessels
- Don't get carried away with vasoconstrictors. By drying out the nasal mucosa, it opens the way for viruses.
- Do not take expectorants and cough suppressants together. They stop each other's action.
How to treat acute respiratory infections with drugs?
The proposed medications for the treatment of acute respiratory infections in adults are used only symptomatically. You do not need to take them several times a day or drink them in certain cycles. The attending physician will definitely select the necessary antipyretic drug, taking into account all contraindications and determine when and how to take the medicine. Unfortunately, many products are toxic and require a competent approach.
If the causative agent of the disease is a virus, antiviral drugs are prescribed:
- Kagocel.
- Interferon.
- Grippferon.
- Amiksin.
- Rimantadine.
- Arbidol.
When the temperature rises above 38 degrees, non-steroidal anti-inflammatory drugs cannot be avoided; this temperature must be reduced. It is worth noting that the simultaneous use of various types of anti-inflammatory drugs can cause increased side effects, so you need to take either drugs containing ibuprofen or paracetamol.
To reduce the temperature during acute respiratory infections, the following is prescribed:
- butadione;
- acetylsalicylic acid;
- upsarin upsa;
- paracetamol;
- ketorolac;
- perfalgan;
- cefekon N (suppositories);
- askofen;
- faspik;
- Nurafen;
- efferalgan with vitamin C.
A sore throat is treated with sprays and lozenges:
- Inhalipt.
- Ambassador
- Faringosept.
- Cameton.
- Strepsils.
- Hexoral.
In case of active inflammatory processes in the bronchi, lungs and larynx with the formation of sputum, adults are prescribed broncho-secretolytic medications:
- Bronholitin;
- Ambroxol;
- ACC;
- Bromhexine;
- Ambrobene.
Antibiotics are prescribed to treat infections: bacterial, microplasma and chlamydial. In serious condition and the possibility of developing complications, the patient must be hospitalized. In these cases, antibiotics and hormonal drugs are prescribed.
A complex of vitamins is prescribed (multivitamins, Revit, Hexavit, Undevit 2 tablets each, Decamevit 1 tablet 2-3 times a day), ascorbic acid up to 600-900 mg/day and vitamin P up to 150-300 mg/day.
Regardless of whether the throat hurts or not, it is necessary to wash the nasopharynx mucosa from germs. Even a small runny nose running down the back wall is an irritant to the pharynx. Rinsing with regular sea salt has a good effect. For half a glass of warm water, take 1/3 teaspoon of salt. Gargle 3 times a day.
Call a doctor so that he can determine how to properly treat a patient with acute respiratory infections and what medications to prescribe. Isolate him from others so that he cannot infect anyone else.
Causes of acute respiratory infections
The cause of the development of acute respiratory infections are pathogenic microorganisms that penetrate a healthy human body and begin active activity there.
ARI, the symptoms and treatment of which in adults should be under close supervision not only of the patient, but also of the general practitioner, is accompanied by a wet cough, which is often combined with purulent sputum. Every person encounters the acute respiratory infection virus several times every day. However, this is not enough to get sick.
In order for the disease to move into the development stage and then into an acute form, you also need:
- severe fatigue of the body;
- weakened immune system;
- stressful conditions;
- hypothermia of the lower extremities;
- inflammation in connective tissues.
Nutrition to support the body
For proper treatment of acute respiratory infections, it is first necessary to reduce the load on the body. Eliminate fatty, fried, spicy, high-calorie foods from your diet. Drink more healthy liquid, dissolve honey under your tongue until it is completely dissolved.
The diet of a sick person should be gentle - you should not starve, nor should you overload the body with food. The diet should be complete in composition and include foods that are easily digestible. Culinary processing of food should also not create unnecessary stress on the digestive system.
To increase the body's resistance to infection and restore vitamin content, consume the following foods:
- rich in vitamin C (citrus fruits, kiwi, rose hip decoction, etc.),
- B vitamins (eggs, vegetables, poultry), retinol (green and yellow vegetables, egg yolk, cottage cheese, butter).
If there is no appetite, the patient should not be forced to eat. At this time, all the body’s forces are aimed at fighting the infection, so the diet should be as light as possible - broths, cereals, fresh vegetables and fruits, dairy products. As soon as the patient recovers, the appetite will appear and it will be possible to return to the previous diet.
Drink plenty of fluids
A patient with an acute respiratory disease needs to drink as much fluid as possible, since the disease is almost always accompanied by general intoxication of the body.
However, not just any drink can be consumed; in this situation, it is best to drink:
- fruit drink made from cranberries;
- weak warm tea with milk or lemon;
- mineral water (preferably still);
- juices that are better to prepare yourself, rather than packaged ones.
Treatment
Treatment of acute respiratory infections should only be carried out under the supervision of a doctor, since even a mild cold can cause serious complications (especially if it develops in an infant or small child). It is permissible to treat mild forms of respiratory infections at home. If a severe form develops, hospitalization in a hospital is indicated.
Treatment of acute respiratory infections includes:
- taking antiviral drugs. Doctors usually prescribe zanamivir, remantadine, oseltamivir for adults and children;
- strict bed rest, especially during fever;
- drink plenty of water. You can use decoctions of medicinal herbs, rose hips, drink tea, etc.;
- taking interferons;
- strict bed rest, especially during fever;
- drink plenty of water. You can use decoctions of medicinal herbs, rose hips, drink tea, etc.;
- At high temperatures, take antipyretic drugs. Adults are prescribed tablets or injections, but children are better off taking medications in syrup;
- anti-inflammatory drugs;
- antihistamines;
- herbal infusions for gargling. This method of treatment is more suitable for adult patients, since not all children can gargle;
- drugs that help relieve pain and discomfort in the throat - sprays, lozenges;
- drops with a vasoconstrictor effect for instillation into the nose. They can even be used to treat infants, but only very carefully. You can rinse the nasal passages with saline solutions (more applicable for adult patients);
- vitamin therapy;
- antitussive drugs.
Treatment of acute respiratory infections at home can only be carried out with the permission of the attending physician. It is important to strictly adhere to the treatment plan so that the effect is achieved as quickly as possible. Treatment at home with folk remedies can only be carried out as a general strengthening therapy, the effect of which will be aimed at increasing the reactivity of the body. You can take decoctions of medicinal herbs, gargle with infusions. They can be easily prepared at home.
There is no need to treat respiratory infections with antimicrobial and antibacterial drugs. They can be prescribed only in case of secondary microbial complications.
Treatment of acute respiratory infections in adults with folk remedies
In most cases, treatment of acute respiratory infections in adults is carried out at home, and folk remedies are widely used here.
- Linden flowers are prepared as an infusion: 2 tablespoons of crushed linden flowers in 2 cups of boiling water, infuse for 30 minutes, filter, take 1/3 cup after meals 4 times a day.
- Gargling with warm decoctions of herbs such as sage, chamomile and calendula is very helpful for inflammation of the tonsils.
- For hoarseness, eggnog is effective - grind 2 egg yolks with sugar until white and add butter, take in between meals.
- Rosehip is a record holder for vitamin C content - what is needed for this acute respiratory infection. Pour one hundred grams of dried rose hips into a half-liter thermos and pour boiling water over it. After six hours, strain, mix with half a liter of pomegranate juice and drink a glass several times a day.
- Radish will effectively help with cough. The top of a radish with a “tail” is cut off and the core is selected. This “cup” is half filled with honey and placed in a glass of water so that the “tail” is immersed in water. Drink a teaspoon of juice 4-5 times a day. Radish is used for no more than 2 days.
- Chamomile is an essential ingredient in many traditional medicine recipes. Pour one spoonful of flowers into a glass of boiling water and place in a water bath for half an hour. Add boiling water to a volume of one liter. Cool slightly and breathe over the steam for a quarter of an hour.
- The most popular inhalation for adults with acute respiratory infections is inhalation of vapors from potatoes boiled with garlic and dill. You need to breathe over the potato steam, covering your head with a towel so that the steam does not escape. In this case, you need to make sure that the steam is not too hot and will not burn the mucous membranes of the throat and nose.
- Expectorant. Mix raspberries and oregano in a 2:1 ratio and brew with a glass of boiling water. Drink the infusion hot 3 times a day and half a glass.
- Pour hot water into a basin and place your hands in there up to your elbows. Keep for 20-30 minutes. When finished, wipe your hands dry, put on a warm sweater and mittens (preferably down ones). In this form you need to go to bed, at least for one hour.
- Grate a clove of garlic and mix with vegetable oil, approximately 50 ml. Then wait a few hours for the oil to infuse and drop it into your nose.
Treatment of acute respiratory infections during pregnancy
Perhaps every doctor will agree that it is better for the expectant mother not to take any medications at all, however, letting acute respiratory infections take their course is also not the best option. A woman should definitely consult with her doctor, who will select the safest medications. When treating acute respiratory infections in pregnant women, you can take: multivitamins, paracetamol-based drugs, bioparox, aqua maris, pinosol, cough syrups, various folk remedies, for example, a decoction of chamomile, sage or eucalyptus. Almost all antibiotics, aspirin, dietary supplements, galazolin, naphthyzin, ambraxol, and calendula tinctures are strictly contraindicated.
Prevention
Prevention of acute respiratory infections includes isolation, regime-restrictive and sanitary-hygienic measures. Certain prospects have recently been associated with antiviral drugs for emergency prevention, as well as stimulants of immunity and general resistance.
Prevention of acute respiratory infections in adults consists of the following measures:
- quitting smoking and drinking alcoholic beverages;
- flu vaccination;
- taking multivitamin complexes;
- prophylaxis with immunomodulatory and antiviral drugs;
- taking foods that contain the amount of vitamins and nutrients necessary for the body;
- complete rest;
- wearing a mask during an epidemic;
- avoiding contact with sick people.
If an acute respiratory infection (acute respiratory disease) has nevertheless visited the body, do not rush to run to work or college. It is better to cope with the illness within a week than to reap the sad fruits of complications, and then bed rest is guaranteed for a longer period.
Prevention of acute respiratory infections and acute respiratory viral infections
To prevent acute respiratory infections of bacterial or viral etiology, experts advise adhering to the following recommendations:
- Limit contacts during seasonal epidemics (going to crowded places - theatre, cinema, public transport during rush hours, large supermarkets, especially with small children, i.e. to any places where excessive crowds of people are possible);
- Carry out regular cleaning of the premises using disinfectants (chloramine, chlorcin, dezavid, dezoxon, etc.);
- Ventilate the room and maintain optimal air humidity in the range of 40-60%;
- Include in your diet foods rich in ascorbic acid and vitamin P (bioflavonoids);
- Regularly rinse the nasal cavity and throat with an infusion of chamomile or calendula flowers.
World statistics show that vaccination can reduce the incidence of ARVI by 3-4 times. However, you should approach the issue of vaccination carefully and understand in what cases it is necessary to be vaccinated against a particular virus.
Currently, prevention of ARVI is mainly aimed at influenza vaccination. It has been shown that the practice of influenza vaccination is justified for the so-called risk groups:
- Children with chronic lung diseases, including asthmatics and patients with chronic bronchitis;
- Children with heart disease and hemodynamic disorders (arterial hypertension, etc.);
- Children, after immunosuppressive therapy (chemotherapy);
- People suffering from diabetes;
- Elderly people who may come into contact with infected children.
In addition, it is recommended to vaccinate against seasonal flu in September-November in preschools, schools, and for staff of clinics and hospitals.
Live (rarely) and inactivated vaccines are used for vaccination. They are prepared from strains of the influenza virus, which are grown in chicken embryo fluid. The reaction to the vaccine is local and general immunity, which includes direct suppression of the virus by T lymphocytes and the production of specific antibodies by B lymphocytes. The virus is inactivated (neutralized) using formaldehyde.
Influenza vaccines are divided into three groups:
- Inactivated whole virion vaccines are used, due to low tolerability, only in the high school group and for adults;
- Subviral vaccines (splits) - these vaccines are highly purified and are recommended for all age groups, starting from 6 months;
- Subunit polyvalent influenza vaccines - such vaccines are prepared from derivatives of the viral shell; this group of drugs is the most expensive because it requires high purification and concentration of the virus-containing material.
Among the drugs used in vaccination are:
- Grippol, produced by the Russian Institute of Immunology, belongs to the group of subunit polyvalent vaccines;
- Vaxigrip, produced in France by Pasteur Merrier Connaught, belongs to the group of subviral vaccines, the vaccine contains formaldehyde, merthiolate and traces of neomycin;
- Fluarix, produced by the Belgian company Smith Klein Beecham, belongs to the group of subviral vaccines, containing formaldehyde, merthiolate and sucrose;
- Influvac, produced by the Dutch company Solvay Pharma, is a subunit vaccine containing purified virus envelope products.
When using a particular vaccine, local or general reactions may occur, accompanied by:
- Malaise;
- Slight redness at the vaccine injection site;
- Increased body temperature;
- Muscle pain and headache.
Children should be given special attention on the day of vaccination. Vaccination requires a preliminary examination of the child by the attending physician. It should be remembered that if there is a suspicion or signs of any infection are already appearing, vaccination should be postponed until the body has completely recovered.
Signs and symptoms of ARVI
The symptoms of acute respiratory diseases are very similar to each other, but the signs of ARVI are pronounced, and the disease is more complex.
The first signs of ARVI are general weakness, headache, and malaise . A sick person often sneezes, the back of the throat and tonsils turn red, and clear mucus begins to be produced in the nose. After a couple of days, with ARVI (which is not the case with acute respiratory infections), the body temperature may rise to 38 degrees. As a rule, it lasts up to three days. If there are no signs of complications, then the acute respiratory viral infection lasts up to ten days, after which the patient recovers well. In the case when ARVI is provoked by the influenza virus, the disease becomes more severe. It may take several weeks for the body to regain its strength.