What is mitral stenosis?
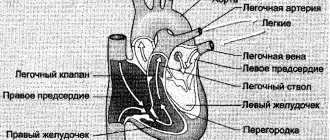
Mitral stenosis (MS) is a cardiac pathology caused by an abnormal structural defect (narrowing of the left atrioventricular orifice) that prevents the passage of blood from the left atrium to the ventricle, caused by degenerative processes of the mitral valve (MV).
The narrowing of the left AV (atrioventricular) opening occurs due to gluing, and then fusion of the tangent edges of the MV valves; the fusion sites are called commissures. Next to this, the valves flatten, the notochordal threads shorten and thicken. The consequence of this is prolapse of the MV valves into the ventricular cavity.
The hemodynamic effect causes damage to the valve on the leaflets with parietal thrombus formation. Further organization of blood clots provokes even greater fusion of the MV valves and progression of the disease. With MS, the structures underlying the valve are involved in the process: the chords shorten, thicken, and fuse together. Sometimes calcification of the commissures occurs, which makes the valves practically immobile.
Diagnostics
If these symptoms appear in the body, you should immediately contact a cardiologist to undergo diagnostics and confirm or refute the presence of pathology in the body. The fact is that the manifestation of these symptoms does not mean that the patient has mitral stenosis. Therefore, diagnosing yourself on your own is unacceptable in any case.
Diagnosis of the disease consists of personal examination, auscultation, laboratory and instrumental research methods.
Initially, the medical history is ascertained, when exactly the symptoms began to appear and whether there were any pre-existing factors for this - excessive physical activity, stress, previous surgeries, and so on. The doctor must perform auscultation (listening to the heart). The auscultation method allows a preliminary diagnosis to be made before a more in-depth diagnosis is carried out.
The standard diagnostic program for mitral stenosis includes the following:
- physical examination – personal and family history, auscultation;
- general blood analysis;
- general urine analysis.
Based on the results of this examination, the following procedures may be prescribed:
- blood chemistry;
- coagulogram (blood clotting test).
In addition, instrumental tests are required:
- ECG;
- ECHO (echocardiography);
- X-ray examination of the chest organs;
- transesophageal echocardiography - since the feeding tube passes very close to the heart, this research method allows you to see the outline of the heart and the size of the mitral orifice.
An ECG examination is mandatory if such a pathological process is suspected. Auscultation can only indicate approximately the extent of the lesion. By the way, an ECG study is mandatory if there is a suspicion of disturbances in the functioning of the cardiovascular system.
Auscultation of the heart
In addition to these research methods and consultation with a cardiologist, consultation with a rheumatologist and cardiac surgeon may be necessary. The doctor can give such prescriptions only if the narrowing of the hole has reached a moderate or severe form.
Reasons for the development of the defect and its classification
Etiology of MS:
- Rheumatism (in 80% of cases);
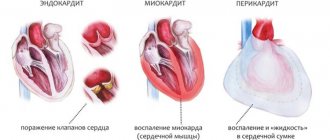
- Infectious, septic endocarditis;
SLE, rheumatoid arthritis, storage diseases, amyloidosis;- Asymmetrical LV hypertrophy in HCM;
- Congenital heart disease (Lutembashe syndrome, patent ductus Botall, myocardial fibroelastosis, coarctation of the aorta, subaortic stenosis);
- Myxoma;
- Thrombus in the left atrium;
- Carcinomatosis;
- Tertiary syphilis;
- Effect of medications (preparations based on wormwood);
- Restenosis after commissurotomy, MV replacement.
Types of mitral stenosis
According to the anatomical characteristics of the narrowing:
- Narrowing like a jacket buttonhole - the valve looks like a jumper with marginal fusion of fibrous valves, a slight shortening of the notochordal threads is visualized;
- Funnel-shaped narrowing like a “fish mouth” - the valve flaps are soldered low to the papillary muscles;
- Combined stenosis.
Degrees of mitral valve narrowing
In a healthy person, the area of the left AV ostium is 4-6 cm2. Clinically, stenosis manifests itself when the area decreases to 2 cm2.
When narrowing to 1 cm2, there is a sharp decrease in tolerance to physical activity. Based on the magnitude of the narrowing of the MV, stenosis is divided into:
- Minimal stenosis;
- Sharp – total area less than 0.5 cm2;
- Pronounced – area from 0.5 to 1 cm2;
- Moderate – narrowing from 1 to 1.5 cm2;
- Minor - the hole area is more than 2 cm2.
Forecast
Stenosis of the left atrioventricular orifice is a severe acquired heart defect. It takes a long time to form; from infective endocarditis (forming factor) to pronounced symptoms of the disease can take an average of 15–20 years. The pathology during this period is completely asymptomatic and is diagnosed accidentally.
With pronounced narrowing of the valve (from 2.2 to 1.7 sq. cm), the life expectancy of 50% of patients is only 5 years (usually death occurs between the ages of 45 and 55 years). Surgical treatment improves the prognosis; the mortality rate in the postoperative period is only 15% over 10 years.
Repeated stenosis is recorded in 30% of patients within 10 years after surgery, which requires additional surgical intervention.
Main symptoms and clinical signs of pathology
The semiotics of clinical manifestations of the disease depends on the stage of stenosis:
- I – compensatory – the patient has no complaints. Signs of MS are found during auscultation, echocardiography, and on ECG only signs of LA overload;
- II – stagnation in the small circle – with paroxysms of shortness of breath, limited ability to work;
- III – right ventricular failure – stable pulmonary hypertension with the formation of a “second barrier”, CHF;
- IV – dystrophic – symptoms of blood flow disorders in both circles, drug support can temporarily improve the condition, rhythm disturbances;
- V-terminal – critical circulatory disorders are comparable to stage III CHF.
Subjective symptoms of mitral valve stenosis:
- decreased tolerance to physical activity;
- chronic fatigue, paroxysmal shortness of breath (later and at rest);
- cough with hemoptysis;
- recurrent pulmonary infections (bronchitis, pneumonia);
- heartbeat;
- distension in the right hypochondrium;
- hoarseness (the hypertrophied left left laryngeal recurrent nerve is compressed by Ortner), discomfort in the pericardial region.
Objective data:
Facies mitralis - blue-red blush on the face in the form of a butterfly;- “Heart hump”, the presence of epigastric pulsation (RV hypertrophy);
- Peripheral edema, acrocyanosis, hepatomegaly, hydrothorax, ascites;
- Tachycardia, atrial fibrillation, pulsus deferens (pulse difference in the radial arteries);
- Diastolic vibration of the chest (“cat purring”);
- Percussion – widening of the boundaries of cardiac dullness upward and to the right;
- Auscultatory picture: “quail rhythm”, strong, clanging 1st tone in the 4th intercostal space on the left,
- the clicking sound of the MK opening at the end of the 2nd tone;
- protodastolic murmur with presystolic amplification;
- accent of the second tone in the second intercostal space on the right and a subsiding Graham-Still noise.
According to the ECG results, there are:
- Symptoms of hypertrophy and overload of the left atrium: Double apical P in I, avL, V4,5,6;
- A significant jump in the amplitude and duration of the P wave in the second phase in V1;
- Extension of the period of internal deviation P longer than 0.06 s.
- 2.1 Deviation of the EOS to the right, dislocation of the S-T interval and inversion of the T wave in avF, III;
Echocardiography shows:
- Unilateral movement of both MV valves anteriorly;
- Slowing down the premature closure of the anterior MV leaflet during diastole;
- Decreased amplitude of movement of the anterior valve leaflet;
- Expanded diameter of the cavities of the left chambers of the heart.
To clarify the stage of the disease, Ro-graphy of the OGK, ultrasound of the OB, and an exercise tolerance test are performed.
Features of hemodynamic disturbances in mitral stenosis
The area of the orifice after which significant hemodynamic disturbances occur is 1-1.5 cm2. Normal intracavitary pressure in the left atrium ranges from 5 to 6 mmHg, and the diastolic pressure gradient between the LA and LV is 1-2 mmHg.
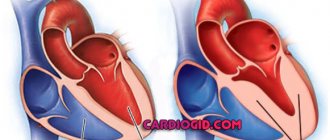
Stenosis of the left AV orifice impedes blood flow and changes intracardiac hemodynamic parameters. Narrowing of the MV orifice to 1 cm2 causes an increase in intracavitary pressure of the left atrium and in the pulmonary venules to 25-30 mmHg. and an increase in the diastolic gradient to 30-40 mmHg. High intracavitary pressure causes hypertrophy of the muscular layer of the left atrium to ensure the pushing of blood into the left ventricle. Through the narrowed orifice, blood flow slows down, the time of blood filling of the left ventricle is prolonged, therefore, the left atrium is emptied for a long time and not completely.
Reduced blood supply to the left ventricle causes ineffective systole, a decrease in ejection fraction and, as a consequence, cardiac output. Increased pressure is passively transmitted from the left atrium to the pulmonary vessels, causing pulmonary hypertension. When borderline pressure in the pulmonary vessels is reached (above 30 mm Hg), a protective precapillary spasm of small arterioles of the small circle develops (Kitaev baroreceptor reflex). The result of long-term spasm is sclerosis of the vascular wall, which further aggravates the phenomena of insufficiency in the pulmonary circulation.
Refractory pulmonary hypertension (more than 150-180 mmHg) leads to thickening of the walls of the right ventricle, and subsequently to its tonogenic dilatation with relative insufficiency of the tricuspid valve. The result of the above pathological processes is decompensation of blood circulation in the systemic circle.
General symptoms
At the initial stage, the disease may not show symptoms at all. As the disease progresses, the following symptoms may occur:
- increased fatigue;
- shortness of breath, even with minor exertion;
- cough with blood;
- arrhythmia or tachycardia;
- asthma attacks at night.
At later stages of the disease, signs of mitral stenosis may be more pronounced. Especially the doctor can detect interruptions in the functioning of the heart using auscultation. At a late stage, a person experiences shortness of breath even at rest. Asthma symptoms become more frequent, and not just at night.
A symptom such as shortness of breath is the first and most sure sign of an illness. But, at the same time, such a symptom, as well as hemodynamics, may indicate other diseases. Therefore, you should consult a cardiologist for an accurate diagnosis.
The patient's appearance gradually changes. Cyanosis of the lips and even fingertips is observed. An unhealthy blush may appear on your cheeks. These are also characteristic symptoms of the disease.
Mitral stenosis can be fatal if not treated promptly. According to statistics, this disease leads to death in 40% of cases.
Treatment of the disease
Unfortunately, there is no specific conservative therapy for this disease. Drug treatment is aimed at:
- Prevention of rheumatic carditis;
- Antibiotic prophylaxis before invasive procedures (prevention of infective endocarditis);
- Treatment of complications that arise.
Indications for conservative (drug) treatment and its main features
Indications for conservative management of patients with MS:
- I, II and V stages of stenosis (when invasive treatment is not advisable);
- Correction of pulmonary hypertension, rhythm disturbances, hemoptysis, CNC;
- Emergency care for pulmonary edema.
The treatment regimen for MS includes:
- Diuretics;
- Long-acting nitrates;
- β-blockers;
- Anticoagulants;
- Ca2+ channel blockers;
- Antiarrhythmic drugs.
When is surgery used and how is it performed?
Indications for surgical treatment:
- Symptoms of pulmonary hypertension;
- MK hole area is less than 1.5 cm2;
- Asymptomatic with a high risk of thromboembolism;
- Pregnancy planning.
Types of invasive treatment:
Percutaneous mitral commissurotomy is a rupture or dismemberment of fused commissures using a balloon inserted through a catheter through the interatrial septum. It has high efficiency, low risk of complications, quick recovery. Do not use in late stages and intracardiac complications.- Open valvotomy is open heart surgery using extracorporeal oxygenation. It is carried out in the presence of a thrombus in the left atrium, calcification of both commissures, combined heart defects, coronary artery disease with the necessary CABG.
- Anuloplasty (mitral valve replacement) is performed for patients with critical damage to the valve apparatus, NYHA class III/IV. Has a higher risk of complications, mortality comparable to commissurotomy. Compliance with all recommendations of postoperative rehabilitation significantly reduces the above risks.
Complications of the operation
Both in the early and late postoperative periods, there is also the possibility of developing complications:
- infective endocarditis (development of bacterial inflammation on valve leaflets, including biological artificial ones);
- the formation of blood clots as a result of the operation of a mechanical prosthesis with the development of thromboembolism - the separation of a blood clot and its release into the vessels of the lungs, brain, and abdominal cavity;
- degeneration (destruction) of an artificial biovalve with repeated development of hemodynamic disorders.
The doctor’s tactics boil down to regular examination of patients using echocardiography, monitoring the blood coagulation system, lifelong prescription of anticoagulants and antiplatelet agents (clopidogrel, warfarin, dipyridamole, chimes, aspirin, etc.), antibiotic therapy for infectious diseases, abdominal surgeries, and minimal therapeutic and diagnostic procedures in gynecology, urology, dentistry, etc.
What is the prognosis for patients with mitral stenosis of varying degrees of severity?
Without surgical treatment, the life expectancy of patients with MS is 40-45 years, about 15% of patients overcome the fifty-year mark.
Invasive treatment of mitral valve stenosis can significantly prolong and improve quality of life. The 10-year postoperative survival rate is 85%.
The most unfavorable prognosis is for patients with stages IV and V, when the compensatory capabilities of the myocardium are insufficient and permanent damage to internal organs develops. Drug correction of emerging complications helps to slightly prolong life.
Statistics
Mitral stenosis is a commonly diagnosed acquired defect of the mitral heart valve:
- the disease is detected in approximately 90% of all patients with acquired heart defects;
- 1 person out of 50-80 thousand suffers from this disease;
- in 40% of cases this is an isolated pathology, in the rest it is combined with other anatomical defects in the structure of the heart;
- the risk of clinical manifestations of the disease increases with age: the most “dangerous” age is 40-60 years;
- women are more predisposed to this disease than men: among patients with this defect, 75% of the fairer sex.
Features in children
The causes of mitral stenosis in children may be systemic autoimmune diseases:
- Rheumatism.
- Dermatomyositis.
- Systemic lupus erythematosus.
- Polymyositis.
In the vast majority of cases, the etiology of the defect in a child is untreated tonsillitis and the lack of bicillin prophylaxis after streptococcal infection.
The disease is characterized by the same hemodynamic changes as in adults, but the clinic has some features:
- Retarded physical development.
- “Mitral face” rarely develops.
- The disease is not complicated by atrial fibrillation.
- The “quail rhythm” is rarely heard; protodiastolic and prediastolic murmurs at the apex of the heart are more typical.
Special symptoms:
- Frequent fainting.
- Pronounced epigastric pulsation (up to the development of a “heart hump”).
Treatment methods:
- Conservative (preparation for surgery)
- Surgical (valve replacement).
The prognosis without treatment is unfavorable . The operation is performed in the first month after diagnosis and is successful in more than 90% of cases. The life expectancy of treated patients is 55-65 years.