Did you know that there are more than 100 types of defects in the structure of the heart and coronary vessels, which are commonly called congenital defects, or congenital defects? Global statistics state that the incidence of congenital heart disease in children is approximately 8 in every thousand. From 0.7 to 1.7% of babies are born with various structural defects of this organ. Heart disease in a newborn is a problem that requires a mandatory solution. Timely detection and adequate treatment of this anomaly can not only save the child’s life, but also give him the opportunity to fully develop.
A little anatomy and physiology
This information will be useful to those who want to understand why a certain defect is more dangerous and why it has the symptoms it does.
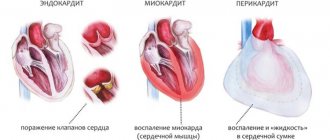
The heart is an organ that performs the function of a pump. It is made up of four chambers - two atria and two ventricles. They are all made of three layers. The internal endocardium forms partitions between the heart chambers:
- Between the atrium and ventricle they look like valves. They open under pressure from blood entering the atrium to allow it to pass into the ventricle. After the blood flows into the ventricle, the valve flaps must close and prevent blood from flowing back into the atrium. Between the left chambers of the heart there is a bicuspid mitral valve, between the right chambers there is a valve consisting of three petals, which is called “tricuspid”.
- The two ventricles are separated by the interventricular septum - a rather dense structure, 7.5-11 mm thick, in the middle of which there is muscle tissue.
- The two atria are separated by the interatrial septum. It is thinner than the interventricular one, but, like the latter, it should not have any holes.
The aorta emerges from the left ventricle - the largest vessel with a diameter of 25-30 mm. The aorta, branching into many branches of smaller diameter, extending from it gradually, as internal organs appear along its path, carries oxygenated blood to them. Its last branches are the iliac arteries. They nourish the pelvic organs and also give off branches going to the legs.
“Wasted” blood, poor in oxygen, but with an abundance of carbon dioxide, leaves all internal organs through venules that flow into veins. The latter gradually also merge together:
- from the lower extremities, pelvis, abdomen they collect into the inferior vena cava (vena cava);
- from the arms, head, neck and lungs with the bronchi - into the superior vena cava.
Both vena cavae, above and below, flow into the right atrium. The blood makes a full circle in 23-37 seconds.
This is a large circle of blood circulation. In its arteries the pressure is higher than in the same vessels of the small circle.
The pulmonary circulation serves to ensure that all arterial blood in the systemic circulation can be oxygenated - saturated with oxygen.
It originates from the right ventricle, which pushes blood into the pulmonary trunk, which soon branches into the right (goes to the right lung) and left (goes to the left lung) pulmonary artery. Branching into smaller and smaller branches, the arterial vessels reach the alveoli of the lungs. There they give off carbon dioxide, which a person exhales.
Oxygen does not enter the arterial, but the venous blood of the pulmonary circulation. Venules with venous blood merge to form veins, and the latter, 4 in number, flow into the left atrium. The blood describes such a path (circle) in 4-5 seconds.
Placental circulation
While the fetus is developing in the uterus, its lungs are not used, since there is no connection between the baby and the surrounding air. But oxygen still reaches the baby, and this happens with the help of the placental circulation. It looks like this:
- oxygenated maternal blood enters intraplacentally;
- from the placenta it goes along the umbilical vein, which is divided into 2 parts:
- one goes into the inferior vena cava and mixes with the blood of the lower half of the body, which is already left without oxygen;
- the second goes to the portal vein, nourishes an important organ - the liver, and then mixes with the blood of the inferior vena cava;
- thus, venous-arterial blood flows through the inferior vena cava;
- non-oxygenated blood flows through the superior vena cava;
- From two vena cava, blood, like in a person after birth, enters the right atrium. But, unlike the extrauterine circulation, the right and left atria communicate with each other through the oval window;
- in the fetus, the foramen ovale is wide: almost all the blood from the right atrium enters the left, and then into the left ventricle;
- from the left ventricle blood enters the aorta;
- a small part of the blood goes from the right atrium to the right ventricle;
- from the right ventricle blood enters the pulmonary trunk;
- Since the lungs are collapsed, the pressure in the arteries that make up the pulmonary trunk is higher, so the blood has to be discharged into the aorta, where the pressure is still lower. This happens through a special vessel - the ductus botallus, which must close after birth. It flows into the aorta after the arteries to the head and upper extremities depart from it (that is, the latter receive more oxygenated blood);
- 60% of the systemic blood flow goes through the 2 umbilical arteries (they go on both sides of the umbilical vein) to the placenta;
- 40% of the blood from the systemic circle goes to the organs of the lower body.
It is precisely due to the structural features of the placental circle that the formed congenital heart defect does not lead to a significant deterioration in the child’s condition in utero.
Normal changes in the cardiovascular system after birth
When a baby is born, the foramen ovale, the communication between the atria, should close within the first year. This happens because when the lungs expand with air, the blood flow in the lungs increases. As a result, the pressure in the left atrium increases, and this “thrust” leads to the closure of the oval window. It does not heal immediately: the more the child screams, cries, and works on sucking (for example, with neurological problems or developmental defects such as a cleft lip), the longer a strong connective tissue – a “damper” – does not form in this place.
Regarding the ductus botallus, the situation is more complicated. It should close within the first 24 hours after birth, but if increased pressure remains in the pulmonary artery, it remains open. This is facilitated by hypoxia suffered during childbirth, which leads to spasm of the pulmonary vessels.
In the first 5-7 days, the pressure in the pulmonary artery decreases during heart contraction and should return to normal within 2 weeks after birth. Then it continues to decrease, because the pulmonary vessels undergo changes: the thickened muscle layer in them decreases, small pulmonary arteries disappear, some of the vessels straighten (previously they were tortuous). In addition, the alveoli, the main areas in which oxygen is exchanged between the air entering the lungs and the blood, expand in the lungs.
Late manifestations of ASD
Atrial septal defect, if not operated on at an early age, causes serious complications and can pose a threat to the patient's life. The most common complication is pulmonary hypertension. High blood pressure leads to fluid stagnation in the lungs. In rare cases, it can cause Eisenmenger syndrome - organic changes in the lungs. Among other complications, the most common are:
- heart failure, especially of the right atrium and ventricle;
- heart rhythm disturbances;
- stroke.
If the defect is not operated on, life expectancy is reduced to 35–40 years.
Incidence of congenital heart defects
Congenital heart disease in newborns occurs in 0.8-1.2%. In 2013, it was registered in 34.3 million people worldwide. It accounts for 10 to 30% of all congenital malformations and ranks second after malformations of the nervous system.
Depending on the nature of the diagnosis, congenital heart defects can be detected in 4–75 cases per 1000 infants born alive. In 0.6-1.9% they are moderate to severe. Congenital heart defects are the main cause of death in children from developmental defects. In 2013, for example, there were 323 thousand deaths worldwide, and in 1990 - 366 thousand. And if a child with a congenital defect lives to be 15 years old, then it is not necessary that he has “outgrown” it, and the risk of severe complications is now reduced.
The most common heart defects are:
- ventricular septal defect (1/5 of all congenital defects);
- atrial septal defects (10-15% in the entire structure);
- open botal duct (10-15% in the entire structure);
- coarctation of the aorta;
- aortic stenosis;
- pulmonary stenosis;
- transposition of the great vessels.
There are defects that are more common in boys, others that are more typical for girls, but there are also those whose frequency is approximately the same in both sexes. Thus, in male infants, stenosis, coarctation of the aorta, transposition of the great vessels, common truncus arteriosus, tetralogy of Fallot, and pulmonary stenosis are more often found. In girls, patent ductus arteriosus, ventricular and atrial septal defects, and Fallot's triad are detected. Information about the gender of the developing fetus increases the likelihood of early diagnosis of characteristic defects.
The greatest concerns regarding the possible presence of such defects are in premature babies and those who were born weighing less than 3 kg. It is these newborns that require the prompt implementation of all diagnostic measures in order to identify possible developmental defects as early as possible.
Symptoms
Photo: gorlor.com
The symptoms of congenital heart disease are very diverse, and it can easily be confused with some other ailments of the body. It is not at all necessary that a congenital heart defect will manifest itself immediately after birth. There are often cases when ultrasound machines fail to detect this defect in the development of a young heart during pregnancy. A newborn child can please parents for some time, who will not even realize that the baby is unwell.
Symptoms of congenital heart disease in newborns.
The main symptom at such an early age is a heart murmur. At this stage of life, only timely visits to the pediatrician will help determine it. By carefully listening to the heart, an experienced doctor can easily diagnose signs of congenital heart disease. Mothers should also observe the color of their child’s skin. As a rule, due to insufficiently active blood circulation and oxygen saturation, the skin may become pale, and in some cases even bluish. Other symptoms of congenital heart disease include lethargy and rapid heartbeat. Nursing mothers should pay attention to their baby's appetite. If your newborn spits up frequently and does not breastfeed well, consult a specialist immediately. However, the most noticeable sign of congenital heart disease is crying. In the first days of life, children are often capricious, since their body is still adjusting to stable functioning, but if the baby begins to turn blue, this should already be a wake-up call.
Symptoms of congenital heart disease in children.
The main symptoms of congenital heart disease may not appear until the age of two. The most noticeable sign of heart disease in children is shortness of breath, and strong physical exertion is not necessary. It is enough for a child to simply recite a rhyme or talk for a while to feel the lack of air.
At the age of 8 to 12 years, a child may develop a sign of congenital heart disease such as frequent headaches. As a rule, they are accompanied by weakness and dizziness and even fainting, especially in exciting or emergency situations, so you should not expose the child to emotional stress and changes. It is also worth paying attention to the child’s complaints. Excessive heart and pulse rhythms are just a few accompanying signs of the disease. In addition to the general picture of malaise, periodic pain in the heart, abdomen and the entire lower body as a whole may also be added. As a result of these symptoms, there may even be a delay in mental and physical development (both of the whole organism and individual organs). Most often, the growth and development of the limbs of the body, both bone and soft muscle tissue, partially or completely freezes.
Symptoms of congenital heart disease in adolescents.
By the symptoms of congenital heart disease, you can determine the disease not only in a baby, but also in a teenager. As a rule, the main difference in the patient's appearance is the bluish discoloration of the skin around the mouth. In some cases, the blue discoloration may spread to the ears and nose. The fingers and toes are also blue. In addition, the outer phalanges thicken, and the nail plates become almost round. This symptom is usually called the “watch glass” or “drumstick” syndrome.
Unreasonable swelling of the feet and legs may also indicate problems with the heart.
However, external differences are not the only sign of congenital heart disease. It is worth paying attention to human behavior. As a rule, people with such a disease are rarely the “ringleaders”. Most often these are inactive, phlegmatic teenagers. They prefer quiet rest in the shade to active games.
Symptoms of congenital heart disease in an adult.
You can also recognize an adult with symptoms of congenital heart disease by such a sign as “heart hump”. This concept is usually called a change in the volume of the chest in a larger direction.
A person with congenital heart disease should constantly monitor his hemoglobin levels. As a rule, in such people it is higher than normal.
There is another symptom that is common to all ages and categories - susceptibility to viral lung diseases. Pulmonary diseases will haunt a person at all stages of his life until surgery occurs and the congenital heart defect is eliminated.
In other words: no matter who you are, an adult or a child, you should not overestimate your health. Listen to your body and pay attention to changes in it, because it may be a symptom of a particular disease.
Why the heart can develop a birth defect
Often the cause of heart defects in newborns cannot be detected. In some cases, these may be individual reasons or a combination of them (most often a combination of genetic factors and various external influences):
Genetic factors
It can be:
- chromosomal disorders (in 5% of cases): trisomy on chromosomes 21, 13 and 18;
- gene mutations (in 2% of cases): in the genes TBX5, NKX2-5, TBX1, MYH6, GATA
Most often, these mutations are sporadic, occurring randomly and cannot be predicted before pregnancy. You can think about the fact that a child can be born with a congenital heart defect when there are (were) people in the family suffering from congenital heart defects, Down syndrome, Turner syndrome, Marfan syndrome, DiGeorge syndrome, Holt-Oram syndrome, Kartagener syndrome, Noonan syndrome and others. You also need to suspect a heart defect if a similar syndrome is detected in the fetus.
Infectious diseases
suffered by a pregnant woman, especially if it happened early in pregnancy. The most dangerous for the developing fetal heart are: rubella, viruses of the ARVI group (especially influenza and adenoviral infection), herpetic group (especially chicken pox and herpes simplex), viral hepatitis, cytomegaly, syphilis, tuberculosis, listeriosis, toxoplasmosis, mycoplasmosis.
Environmental factors
polluted air, radiation, living in mountainous areas or in places of high atmospheric pressure.
Toxic effects on the fetus if pregnant:
- takes certain medications: antibacterial and sulfa drugs, anticonvulsants and antiepileptic drugs (for example, Trimethadione), lithium preparations, painkillers and hormonal medications;
- smokes;
- takes drugs (amphetamines have a particularly toxic effect on the fetal heart);
- works with paint and varnish products, nitrates;
- drinks alcohol, especially in the initial weeks of gestation.
Causes related to maternal metabolism:
when she suffers from endocrine diseases (especially diabetes), is undernourished or, on the contrary, is obese.
If a pregnant woman is sick with diseases such as:
systemic lupus erythematosus, phenylketonuria, rheumatism.
At risk
In addition, we can say that the following pregnant women are at risk for developing congenital heart defects in children:
- over 35 years old or under 15 years old;
- having a history of stillbirth;
- with a history of spontaneous miscarriages;
- with bad habits (alcohol consumption is especially dangerous: the risk of congenital heart disease reaches 40%);
- if the child is conceived from a blood relative;
- when toxicosis of the first trimester is expressed;
- if the pregnancy proceeds with the threat of termination;
- whose family has relatives with heart defects.
What it is?
Congenital developmental defects are defects in the development of the fetus during its intrauterine development. Non-fusion of the upper lip is considered a congenital defect, which is accompanied by an impaired cosmetic effect. This process can only be corrected surgically.
Another birth defect is non-fusion of the two halves of the hard palate. With this pathological process, the development of a cleft palate is observed. This is the most severe pathological change in the patient’s appearance.
Hemolytic disease is also a congenital pathology. Moreover, this is due to the Rh factor. The Rh factor can affect the circulatory system of the newborn, degeneration of red blood cells occurs, and the formation of blast structures in them.
Another congenital pathology is dropsy. Dropsy is the most severe pathology, and the child may die. Severe newborn jaundice is associated with yellowing of the skin, a condition that progresses over time.
go to top
At what age does heart disease develop?
The critical period when the above factors have a high chance of leading to the formation of heart defects is the first 3 months of pregnancy. At this time, cardiac structures are formed, and the influence of microbial, medicinal or industrial toxins on the fetal body can stop their development or lead to the formation of a heart “as at the previous stage of phylogenesis” (for example, as in reptiles, birds or amphibians). Cardiac structures are formed according to a clearly drawn up plan, and changes in it lead to the formation of one or another defect.
Around the 15th day of intrauterine development, the cells that give rise to the heart are located in the middle germinal layer (mesoderm) in the form of two horseshoe-shaped stripes. Some cells migrate here from a region of the outer germ layer (ectoderm) called the neural crest, a region that supplies different nerve cells to different parts of the body.
On day 19, 1 pair of vascular elements is formed - endocardial tubes. They merge with each other, the cells between them undergo programmed death, and the cells of the primary heart migrate to the tube and by day 21 form a ring of muscle cells around them. By day 22, the heart begins to contract and blood begins to circulate.
At the time of 22 days, the vascular system is a bilaterally symmetrical system with paired vessels on each side of the body and the heart, represented by a primitive tube located in the middle, in the middle layer of the body. Its sections, from which the atria are formed, are located further from the head (although it should be the other way around).
From days 23 to 28, the heart tube folds and twists. The future ventricles move to the left side of the center, taking their final location, and the atria move to the head end of the body. On the 28th day, the tissue of the heart tube expands, and within 2 weeks 4 heart cavities are formed here, separated by a primary membrane septum. If a damaging factor acts at this stage, blood will flow between the cavities of the heart.
Cells migrated from the neural crest give rise to the formation of the cardiac bulb, the main outflow tract from the heart. The bulb must be divided into 2 parts by the growing spiral septum, and then the ascending aorta and pulmonary trunk are formed. If the separation by the septum does not end, a defect is formed - a persistent ductus arteriosus. And if the vessels are located in the opposite direction, transposition of the great vessels results.
The two halves of the outflow tract must occupy certain positions at certain ventricles. When exposed to damaging factors at this stage, a “riding aorta” defect is formed (when the vessel originates from the interventricular septum).
Some of the cells of the septum primum die, forming an opening. At the same time, muscle cells grow here, forming a secondary septum, but the gap between the atria remains. This is the foramen ovale (window) - a shunt through which blood flows from the right to the left atrium. At the same stage, the ductus botallis is formed - a connecting channel between the aorta and the pulmonary artery.
Causes
ASD is a hereditary disease, the severity of which depends on genetic predisposition and the influence of adverse environmental factors on the fetus. The main reason for the formation of ASD is a violation of the development of the heart in the early stages of embryogenesis. This usually occurs in the first trimester of pregnancy. Normally, the fetal heart consists of several parts, which during their development are correctly compared and adequately connected to each other. If this process is disrupted, a defect remains in the interatrial septum.
Factors contributing to the development of pathology:
- Ecology - chemical, physical and biological mutagens,
- Heredity - point changes in a gene or changes in chromosomes,
- Viral diseases contracted during pregnancy,
- Diabetes mellitus in mother
- Use of medications by a pregnant woman
- Alcoholism and drug addiction of the mother,
- Irradiation,
- Industrial hazards,
- Toxicoses of pregnancy,
- The father's age is more than 45 years, the mother's age is more than 35 years.
In most cases, ASD is combined with Down's disease, renal anomalies, and cleft lip.
What are the dangers of congenital heart defects?
Congenital cardiac defects lead to the development of major symptoms and complications through one of two mechanisms:
- The flow of blood through the vessels is disrupted. In case of anomalies with valve insufficiency or septal defects, the parts of the heart are overloaded with an increased volume of blood. If the defects involve narrowing (stenosis) of the openings or blood vessels, then the heart is overloaded with resistance. First, from any overload, the cardiac muscle layer increases, and the strength of its contractions increases. Afterwards, the compensation mechanisms “break down”, and the muscles of the enlarged heart become thinner. This disrupts systemic circulation and leads to cardiac failure.
- There is a disturbance in the systemic blood flow: either there is a lot of blood in the small circle, or there is little blood in one of the circles. Because of this, the supply of oxygen to organs deteriorates.
With “blue” defects, less oxygen is delivered due to a disruption in the speed of blood movement through the vessels. When the defect is “white,” hypoxia is associated with difficulties in the release of oxygen by hemoglobin molecules.
These pathogenetic mechanisms are the basis for the classification of congenital heart defects into phases, which, in turn, is used to determine treatment tactics. Thus, there are 3 phases of the disease:
Phase 1 – compensation and adaptation. The body compensates for the resulting disturbances by increasing the saturation of the myocardium.
Phase 2 is relatively compensatory. The heart muscle no longer functions as intensively. The structure and regulation of the heart is disrupted. The child’s physical development and motor activity improve.
Phase 3 – terminal. It occurs when the compensatory capabilities of the heart are exhausted, which is why dystrophic changes develop in the myocardium and internal organs. This stage ends with death. Infectious diseases, lung diseases and other pathologies can hasten its onset.
Consequences: what will happen if left untreated?
A congenital heart defect is not a situation that can be left to chance. Without treatment, congenital heart disease leads to the development of complications:
- heart failure is a condition in which an organ is unable to do its job;
- rhythm disturbance;
- infective endocarditis - bacterial damage to the heart valves;
- bronchopulmonary diseases (bronchitis, pneumonia).
All these conditions significantly disrupt the normal course of life, prevent full development and can cause disability.
Classification of congenital cardiac defects
There are more than 100 forms of congenital heart abnormalities. Based on the nature of changes in blood circulation and, accordingly, the main symptoms, there are 2 main types of defects - “blue” (in which the baby’s skin has a bluish tint) and “white” (the baby’s skin is pale). They also have their own division.
"White" anomalies:
with them, arterial and venous blood do not mix. But this does not exclude the possibility of blood discharge from an area of higher pressure (from the left ventricle, that is, the systemic circle) to an area of lower pressure (to the right ventricle, the “source” of the pulmonary circulation):
- defects in which the volume of blood in the small circle increases. This is a functioning ductus arteriosus, atrial and interventricular septal defect, atrioventricular communication;
- anomalies associated with a decrease in the amount of blood in the pulmonary circulation: for example, isolated stenosis of the pulmonary trunk;
- defects that caused reduction (depletion) of blood in the systemic circle: isolated aortic stenosis, coarctation of the aorta;
- without any special discharge of blood from right to left. This occurs when the heart is structured normally, but is not located in its place, but on the right (dextrocardia), in the middle of the chest (mesocardia), in the abdominal cavity (abdominal dystopia of the heart), in the neck (cervical dystopia). A similar type of defect is characteristic of the bicuspid aortic valve (it should be tricuspid)
“Blue” defects, when mixing of arterial and venous blood occurs:
- when enrichment of the pulmonary circulation occurs (Eisenmenger syndrome, transposition of the great vessels);
- with depletion of the small circle: tetralogy of Fallot, Ebstein's defect.
Exodus
Death most often occurs with hydrops of the newborn. Biliary atresia can also be fatal. This is due to its severe course.
Atresia can lead to severe cachexia. Cachexia in most cases cannot be corrected. Since exhaustion of the body causes dysfunction of organs and systems.
Recovery occurs with comprehensive treatment. However, only with a mild course of the disease. Severe disease leads to disability and death.
go to top
How do congenital heart defects manifest?
Symptoms of heart disease depend on the type of pathology.
Signs of “blue” defects
Defects such as patent truncus arteriosus, tetralogy of Fallot, congenital fusion (stenosis) of the tricuspid valve, anomaly of the connection of the pulmonary veins are manifested by the following symptoms:
- the lips and nasolabial triangle may be bluish at rest (if the defect is significant), but this color can only appear during screaming, sucking or physical exertion;
- cyanotic fingers, which over time take on the appearance of “drum sticks”: completely thin, but thickened in the area of the nail phalanges;
- rough murmur over the heart;
- frequent infectious diseases, pneumonia;
- weakness;
- increased breathing;
- delayed physical and mental development;
- children are short;
- puberty occurs late.
In addition to changes in skin color, fatigue, weakness, shortness of breath, and changes in heart rate, congenital heart disease should be suspected if the child has one of these anomalies (abbreviation VACTERL):
- V – spinal anomalies (vertebral);
- A – anal atresia;
- C – cardiovascular (cardiovascular) abnormalities;
- T – transesophageal fistula (abnormal connections between the esophagus and other organs);
- E – esophageal (esophageal) atresia;
- R – renal (renal) anomaly;
- L – developmental defects of the limbs.
Signs of “white” defects
Such anomalies that occur with enrichment of the pulmonary circulation, for example, a ventricular septal defect, can be suspected immediately after the birth of a child. This:
- heart murmurs and increased heart rate, which are usually immediately heard by the neonatologist examining the baby immediately after birth;
- bluish tint of the skin, especially pronounced in the extremities;
- breathing that is more frequent than normal;
- poor appetite;
- light weight;
- lack of appetite or weak desire to breastfeed;
- inactivity;
- The baby sucks the breast/pacifier, but quickly gets tired and lets go.
If the septal defect is small, and all of these signs are mild, then poor weight gain should alert parents. Minor defects may even heal by the age of 10, but treatment should be carried out to reduce pressure in the pulmonary circulation system.
Anomalies of the interatrial septum are also characterized by disturbances in heart rhythm and the appearance of a protrusion of the chest wall in the area of the heart (“heart hump”).
An anomaly such as coarctation of the aorta is characterized by a feeling of heaviness and pulsation in the head, flushes of “heat” to the head, dizziness, and shortness of breath. Pulsating arteries are visible in the neck. Legs feel numbness, weakness in the legs; they are cold, and during physical activity there are cramps in the calf muscles.
If with a “white” defect there is no mixing of arterial and venous blood, this is manifested by the following signs:
- pain in the heart area;
- increased heart rate;
- dizziness, possibly with fainting;
- increased blood pressure;
- dyspnea;
- throbbing pain in the head.
Lifespan
Due to the development of severe symptomatic complexes, life expectancy is reduced. Therefore, complex treatment designed to reduce acute symptoms is required. Life expectancy also depends on the reasons that led to the development of these conditions.
If the reason is the presence of infectious lesions in the mother, then life expectancy may decrease. Infections usually lead to severe lesions. The hemolytic etiology of these conditions is also dangerous.
Life expectancy is higher if careful prevention is carried out in both mother and child. The disease can be prevented by planning pregnancy. Which in this case excludes the development of these conditions.
Complications of congenital heart defects
The consequences of heart disease depend on the form of the defect and its severity. The main complications are:
- bacterial endocarditis;
- cardiac failure;
- frequent inflammation of the bronchi and lungs;
- attacks with shortness of breath and bluish skin;
- angina pectoris;
- myocardial infarction;
- thrombosis of peripheral veins;
- thromboembolism of cerebral vessels;
- rheumatic endocarditis;
- vascular aneurysms or their early atherosclerosis (typical of coarctation of the aorta).
Diagnostics
Some heart defects are detected during pregnancy using fetal echocardioscopy. This test is performed between 18 and 24 weeks of pregnancy using a transabdominal or transvaginal probe.
Often, congenital heart disease can be suspected after birth - by its characteristic appearance, rapid fatigue, and refusal to breastfeed. Sometimes the doctor’s attention is immediately drawn to disturbances in heart rhythm, heart murmurs, and expansion of the boundaries of this organ.
If no pathology is detected during examination, the defect can be suspected by a routine electrocardiogram or chest x-ray performed for suspected pneumonia. Heart defects are confirmed by echocardioscopy with Dopplerography (ultrasound of the heart with determination of blood flow in the cavities and through large vessels), but the final diagnosis is made in the cardiac center according to the following data:
- expert class echocardioscopy;
- inserting catheters into the cardiac cavities to measure pressure in them;
- angiocardiography.
Critical periods of embryonic and fetal development
So, in the development of the embryo and fetus, three main periods can be distinguished:
1) the first period, preembryonic, which continues after fertilization during the first week of pregnancy. The critical moments of this period are fertilization and implantation. The action of unfavorable factors during this period causes an embryotoxic effect or the absence of any influence, the “all or nothing” law;
2) the second period is embryonic, lasting from 3 to 8 weeks after fertilization (within 5-10 weeks of gestational age) (period of organogenesis). This is the most sensitive and dangerous period (critical) for exposure to aggressive environmental factors. The action of unfavorable factors during this period causes a teratogenic effect;
3) the third, fetal (fetal) period lasts from the 9th week of pregnancy until the birth of the child. During the fetal period, aggressive factors usually do not cause significant malformations, but can cause mental impairment and abnormal behavioral reactions in the postnatal period.
Therapy of defects
Treatment of congenital heart defects is divided into medical and surgical. The first type is used for minor defects, as well as at the stages of preparation for and after intervention. It is aimed at stabilizing pressure in the pulmonary artery system or systemic circulation, improving myocardial trophism and oxygen absorption by internal organs. For this purpose they prescribe:
- diuretics;
- potassium salts;
- digitalis preparations;
- antiarrhythmic drugs;
- beta blockers;
- indomethacin - according to the regimen. This is the only radical drug treatment that can completely solve the problem in the case of an open ductus arteriosus.
Some cardiac anomalies can resolve on their own, without surgical treatment, but this usually does not apply to “blue” defects.
Surgery for heart defects takes into account the type and phase of the defect:
- If the cardiac defect is within phase I, emergency surgery is performed before one year of life. For example, when the small circle is depleted, this is artificial stenosis of the pulmonary artery; when the small circle is overfilled, it is the application of an artificial ductus arteriosus.
- In phase II, a planned operation is carried out, which is carried out after careful preparation, at various times (usually before puberty).
- In case of decompensation, when the defect is detected already in the third phase, only this type of intervention can be carried out that will slightly improve the child’s quality of life.
If the cardiac anomaly was discovered before birth, then some types of operations can already be performed in utero. In cases where this is not possible and the defect is a life-threatening anomaly, the woman is given birth in a specialized hospital, after which the child undergoes the necessary intervention immediately after birth. For some serious defects, a heart transplant may be possible.
Treatment
Photo: medicinetrip.ru
This disease is the most common intrauterine anomaly in children. Therefore, parents faced with this problem are wondering whether congenital heart disease can be treated?
Some complex heart defects are diagnosed in newborns immediately in the maternity hospital. In this regard, instead of being discharged, the child is sent to the cardiology department. Treatment options and patient care will depend on the severity and complexity of the disease. The clinical picture with this diagnosis is always different.
Treatment of congenital heart defects in children
Treatment is aimed at improving the patient’s condition, correcting defects in the cardiac cavity, so that the child can lead a normal life in the future, i.e., achieving an optimal level of the patient’s quality of life.
Depending on the age of the patient, he will be observed by a pediatrician, a pediatric cardiologist, and in adults - by a regular cardiologist.
It is possible to completely cure some heart defects with surgery. The operations are performed by cardiac surgeons: both in the first days of children’s lives and during the first year of life. If a patent ductus arteriosus is diagnosed, provided there are no life-threatening symptoms, a wait-and-see approach is possible. There is a possibility that the defect will close on its own in the first two years of a child’s life.
During cardiac surgery, the chest wall is cut or a probe is inserted into the vessels.
Unfortunately, when diagnosing a three-chambered heart (characterized by the presence of one atrium and two ventricles, or two atria and one ventricle), surgical intervention is not possible. Such a vice is incompatible with life.
The treatment process includes not only surgical correction, but also therapeutic methods.
Therapeutic methods in the treatment of congenital heart defects are aimed at strengthening the heart muscle and ensuring normal blood supply. Therapeutic treatment methods:
- drug therapy (taking medications);
- physiotherapeutic procedures (therapeutic massage, light physical activity).
Surgical treatment of congenital heart defects is aimed at eliminating developed defects in the heart. Methods of surgical treatment:
- removal and replacement of damaged valves;
- connection of sections of the heart muscle;
- installation of a pacemaker;
- transplantation.
Therapeutic treatment
The basis of this treatment is to regularly take medications prescribed by the doctor. Most often, a cardiologist prescribes the following drugs:
- vasodilators;
- nootropic;
- cardiac;
- diuretics;
- hypotensive;
- vitamins.
The period of taking medications depends on the severity of the disease. The effect of medications helps lower blood pressure, normalize brain function, improve blood circulation in the heart arteries, and increase immunity.
Important!
The dosage of drugs and the duration of the course should be prescribed by a cardiologist. Otherwise, self-medication may provoke a deterioration in the patient’s condition, as well as the development of complications.
Forecast
Congenital heart disease - how long do you live with it? This is based on the form of the anomaly:
- With a functioning ductus botallus, septal anomalies or stenosis of the pulmonary artery, mortality in the first year of life without treatment is 8-11%.
- Tetralogy (a combination of 4 defects) of Fallot and pathologies of the myocardium structure cause a mortality rate of 24-36% in children under one year of age.
- Coarctation, aortic stenosis and aortic dextraposition lead to 36-52% mortality in the first year of life. Average life expectancy is 12 years.
- With left ventricular hypoplasia, pulmonary atresia, and common aortic trunk, 73-97% die in the first 12 months of life.
To prevent the formation of cardiac defects as much as possible, even before pregnancy, a woman should be vaccinated against rubella, add iodized salt and folic acid to her food. While pregnant, the mother should not smoke, take alcohol or take drugs. If there are frequent cases of heart defects in the family, a woman or man should consult a geneticist and, perhaps, not plan a pregnancy.
Author:
Krivega Maria Salavatovna resuscitator
Clinical case
A 3-month-old baby was admitted for consultation. From the anamnesis it is known: second pregnancy, delivery by cesarean section at 39-40 weeks. The pregnancy was accompanied by gestosis; in the first trimester, the woman suffered from acute respiratory viral infection (she was treated at home on her own).
A neonatologist at the maternity hospital suspected a congenital heart defect on the third day after the baby was born. The doctor listened to a rough systolic murmur along the left sternal border and referred the child for examination. On the fifth day, echocardiography was performed. A diagnosis was made: open atrioventricular canal, incomplete form. With this pathology, a defect occurs in the lower part of the interatrial septum, and the bicuspid (mitral) valve is split.
Maintenance therapy was prescribed: cardiac glycosides, diuretics. During treatment, the child's condition remained stable.
At the age of 3 months, a repeat examination was carried out. Based on the results, a decision was made to hospitalize and prepare for surgery. The scope of surgical intervention is radical correction of the defect under artificial circulation. A patch was made from the patient's own pericardium (the sac surrounding the heart), and the mitral valve was sutured. The postoperative period was uneventful. Upon further observation, the patient's condition remained stable.