© Author: Andrey Alekseevich Illarionov, therapist, bacteriologist, especially for SosudInfo.ru (about the authors)
Carditis is an infectious-allergic inflammation of the various membranes of the heart. Carditis occurs in almost all age groups, but most often in young children, mainly boys. The disease manifests itself with nonspecific symptoms and is dangerous due to the development of complications. Carditis is characterized by tachycardia, shortness of breath, and cyanosis. Sick children lag behind their peers in physical development.
In practical medicine, the term “carditis” means simultaneous damage to several membranes of the heart .
Classification and reasons
To understand what carditis is, it is worth studying their types and forms. They are classified according to different criteria. Primarily rheumatic and non-rheumatic.
Rheumatic carditis develops against the background of a systemic autoimmune disease – rheumatism. In this case, all the membranes of the heart are involved in the pathological process; the myocardium is first affected, which can result in endocarditis and pericarditis.
According to statistics, in 90-95% of adult patients (70-85% in children), the membranes of the heart are affected already during the first rheumatic attack.
In 20-25% of cases the disease leads to acquired heart disease. The majority - 59% of the sick - recover thanks to timely active treatment , there are no changes in the heart.
Non-rheumatic carditis is due to other reasons. It is also quite common in medical practice. Both adults (age and gender do not matter) and children are susceptible to non-rheumatic carditis. In the latter, non-rheumatic carditis occurs more often than in the “adults” category.
According to experts, 0.5% of all hospitalized patients are children with non-rheumatic carditis . Autopsies of deceased minors show 2.3–8% carditis. The percentage can rise to 10-15 if a viral infection is confirmed.
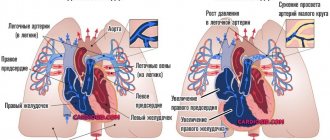
The photo shows the classification of carditis by localization of inflammation:
Non-rheumatic carditis has the following ethology:
- Viral . Generated by influenza viruses, polio, rubella, chickenpox, adenoviruses; enteroviruses – herpes, Coxsackie, ECHO.
- Bacterial . Cause: typhoid fever or diphtheria.
- Allergic . Reason: drugs, vaccine, serum.
- Fungal . Cause: coccidioidomycosis.
- Parasitic . Cause: toxoplasmosis, histoplasmosis, schistosomiasis.
- Unknown etymology.
Non-rheumatic inflammation of the membranes of the heart is also classified according to periods of occurrence, nature of the course, severity and outcome.
By period of occurrence:
- congenital;
- acquired.
Congenital carditis can be early or late , and is detected in newborns in the first days or months of life. Cause: intrauterine viral/bacterial infection suffered by the mother during pregnancy.
Acquired carditis occurs in children as a result of a viral, bacterial infection or rheumatic attack.
By duration:
- acute (inflammatory process lasts less than three months)
- subacute (inflammation lasts up to eighteen months)
- chronic (the disease lasts more than one and a half years)
Description of infectious pericarditis
The pericardium is anatomically a thin membrane that surrounds and protects the heart from external damage. Inflammation of this serous layer leads to pericarditis and if the underlying cause is any infection, then infectious pericarditis is diagnosed.
Infectious pericarditis varies depending on the cause of the disease. The most common forms of IP are:
- Parasitic
- Bacterial
- Viral
- Fungal
- Rickettsial
- Tuberculous
A similar classification according to E.E. Gogin, 1979 allows for more targeted treatment subsequently, which gives better results.
Additionally, according to the nature of the course, infectious pericarditis can be acute, chronic or recurrent.
- Acute pericarditis lasts no more than 6 weeks and, depending on the amount and nature of the pericardial effusion, can be dry (fibrinous) or exudative. In the latter case, pus, blood or fibrinous inclusions can be detected, then they speak of purulent, hemorrhagic or serous-fibrinous pericarditis, respectively.
- Subacute pericarditis lasts from 6 weeks to no more than 6 months. Its characteristics are the same as those of acute pericarditis.
- Chronic pericarditis. Its duration is from 6 months. It, like acute, can be exudative, but in addition there are also adhesive and constrictive pericarditis.
- Recurrent pericarditis. Develops again after previously treated inflammation of the pericardium.
There are also non-inflammatory forms of pericarditis, such as pneumopericardium, hydropericardium, chylopericardium and hemopericardium, but they are not so typical for infectious pericarditis.
Features of the development of infectious pericarditis:
- May develop due to protozoan infestation, such as malarial or amoebic pericarditis.
- Parasitic pericarditis is most often caused by echinococcus.
- Bacterial pericarditis can be specific or nonspecific. An example of the former is dysenteric, tulareic and syphilitic pericarditis, the latter - various bacterial pericarditis, mainly coccal.
- Non-bacterial infectious pericarditis are rickettsial and viral diseases, mainly developing against the background of influenza, infectious mononucleosis, etc.
- Fungal infectious pericarditis is most often associated with candidiasis and actinomycosis.
It is worth pointing out that approximately 30% of people with viral pericarditis or pericarditis of unknown cause have one or more episodes of exacerbation of the disease. [1 - Imazio, M; Gaita, F; LeWinter, M (13 October 2015). "Evaluation and Treatment of Pericarditis: A Systematic Review". JAMA. 314 (14): 1498–506] The pathogen can enter directly into the pericardial cavity, but if it is present in the body, infectious-allergic reactions can be triggered, and if a connection between allergization and the microbial pathogen is proven, then they also talk about infectious pericarditis. An example of such a condition is rheumatic pericarditis.
Symptoms and signs
The primary symptoms of inflammation of the cardiac membranes are difficult and require special attention from the attending physician. The nature of the disease rarely directly indicates heart problems. Especially in cases of acquired carditis after an infectious disease.
The patient complains of weakness, fatigue, lack of appetite, nausea, and decreased attention. Such general symptoms accompany many diseases.
The development of the process gives more definite signs of cardiac pathology : tachycardia, arrhythmia, dullness of heart sounds, shortness of breath, edema, cyanosis.
But they also often coincide with the characteristic features of other cardiovascular diseases such as mitral stenosis, arrhythmia of extracardiac origin, rheumatism, heart disease, and tumor processes in the myocardium.
In children, carditis is accompanied by cough and pain in the heart area . The child cannot talk about pain; he tries to avoid sudden movements and breathe shallowly.
by signs of conduction disturbances and automaticity that persist for a long time , along with other indicators indicating hypertrophy of the left heart and myocardial ischemia. X-ray reveals changes in shape, enlargement of the cardiac tissue of the left ventricle, slow pulsation (80-85% of patients).
Diagnostics
To correctly diagnose carditis, it is necessary to collect anamnesis and clarify complaints. The results of instrumental and laboratory studies will help confirm or refute the suspected diagnosis.
- In the blood of patients there is pronounced leukocytosis, increased ESR, and dysproteinemia.
- Microbiological examination of nasopharyngeal discharge makes it possible to isolate the causative agent of the disease. In the blood there are antibacterial, antiviral and anticardiac antibodies.
- These immunograms indicate characteristic changes in the immune status - an increase in immunoglobulins IgM and IgG, an increase in antibody titers.
- If rheumatoid carditis is suspected, patients are advised to donate blood for rheumatoid factor.
- Electrocardiography is an important instrumental method that detects myocardial damage during carditis and reveals arrhythmia, AV block, and hypertrophy of the left chambers of the heart.
- FCG - systolic murmur, the appearance of pathological 3 and 4 tones.
- X-ray of the chest organs - cardiomegaly, enlarged thymus gland in children, congestion in the lungs.
- Angiocardiography is the study of the cavities of the heart and coronary vessels by introducing a contrast agent. The resulting image shows the coronary arteries and chambers of the heart. This technique allows you to evaluate the shape and size of the left ventricle, the condition of the interventricular septum, and the presence of blood clots in the heart.
- Ultrasound of the heart - expansion of the chambers of the heart, accumulation of exudate in the pericardial cavity.
Which doctor should I contact?
Treatment of heart diseases is carried out by a cardiologist . It is he who will make an accurate diagnosis and prescribe qualified treatment. a cardio-rheumatologist, can continue treatment .
The primary diagnosis of heart problems is carried out by a therapist . At the slightest suspicion, he will refer the patient to a cardiologist. In case of a viral disease, an infectious disease specialist should identify signs of carditis and also redirect the patient to a consultation with a cardiologist.
Treatment tactics
The disease is treated comprehensively and step by step. Requires a long time . The doctor takes into account all the nuances: the severity of the process, how timely the patient sought help, what form the disease takes, what was its cause, as well as the age of the patient, his general physical condition.
In the acute form or sharp exacerbation of chronic carditis, hospitalization is required for 10-14 days and up to 1 month. In the first acute phase, etiotropic antibacterial drugs . The patient is on strict bed rest.
A special diet is required - foods enriched with potassium salts, vitamins (recommended: baked potatoes, dried apricots, raisins), limited salt intake. You should not eat foods that delay the removal of fluid from the body to prevent edema. If the disease is severe, oxygen therapy is prescribed.
When relieving acute inflammation of the heart membranes, outpatient treatment is permissible.
In the first two months of treatment, the patient takes anti-inflammatory non-steroidal drugs - indomethacin, voltaren in combination with vitamins, antihistamines and potassium. Diuretics are often prescribed.
In case of severe, protracted course of the disease, the doctor may prescribe prednisolone. In case of heart failure, cardiac glycosides are indicated. If signs of intravascular coagulation appear, drugs are prescribed that improve microcirculation and metabolic processes in the myocardium . Antiarrhythmic therapy is possible.
When the process goes through an acute period, the person is recommended to engage in physical therapy .
However, significant physical activity is strictly contraindicated . Children are exempt from physical education and subbotniks. Preventive vaccinations are possible no earlier than five years later and after consultation with a cardiologist.
Rehabilitation treatment in special cardiological sanatoriums is also . A cardiologist or cardiorheumatologist monitors the patient throughout the year: routine examinations are carried out and an ECG is prescribed every three months.
Forecast
The prognosis for inflammation of the lining of the heart depends on many factors: the patient’s health and age, the state of his immune system, timeliness and proper treatment, hereditary predisposition, compliance with doctor’s recommendations and preventive measures.
Only when, after a year or two, a person has completely disappeared all signs of an inflammatory disease of the membranes of the heart, is he considered completely cured. This outcome of the disease is observed more often in acute forms of carditis .
With a subacute course of the disease or its chronic version, carditis has a protracted course, which is fraught with various complications: arrhythmia, pulmonary hypertension, myocardial hypertrophy and cardiosclerosis.
Any of the complications worsens the prognosis for recovery and does not exclude death. This is the danger and insidiousness of this disease.
Prevention
Experts divide preventive measures to prevent carditis into primary and secondary.
Primary
Primary prevention involves measures to prevent the occurrence of a disease. In case of rheumatic carditis, prevention is aimed, first of all, at preventing the occurrence and development of rheumatism in the human body.
In practice, this is a complex of general strengthening actions , such as hardening, physical exercise, a balanced diet, taking vitamins, etc.
In cases of non-rheumatic carditis, the goal of prevention is to prevent infection by various types of infections . Particular attention is required during periods of epidemics. A set of measures: general strengthening and health-improving procedures, taking vitamins and drugs that increase immunity.
In pediatrics, primary prevention is measures to prevent pregnant women from getting infections , identifying and sanitizing foci of infection in the body of the expectant mother, and following vaccination rules. Particular attention is paid to risk groups: pregnant women with family history and cardiovascular diseases.
Prevention of carditis in children : hardening of the newborn, clinical observation of children at risk.
Secondary
Secondary prevention includes a number of measures to prevent relapses and the development of complications. Constant supervision of specialists, timely diagnosis, therapy, preventive treatment courses .
For rheumatic carditis, these are measures to prevent relapses of rheumatism. Usually they include the introduction of long-acting antibiotics (bicillin, penicillin, retarpen, pendepon).
The timing of anti-relapse treatment is determined individually. Patients with established heart failure must take preventive measures for life.
Carditis is a disease that can be successfully treated by modern medicine. However, the risk of complications still remains serious in all age groups of patients. In order not to develop a chronic cardiovascular disease, you should contact specialists in a timely manner, accurately describe all disturbing symptoms , require an in-depth examination, timely diagnosis and treatment.
Pathogenesis of the disease
Non-rheumatic carditis develops as a result of the direct cardiotoxic effect of the pathogen with the formation of destructive and inflammatory changes in the membranes of the heart muscle. As a result of the introduction of an infectious agent, the formation of cytotoxic T-lymphocytes, antibodies to cardiomyocytes, and CECs occurs, which cause allergic reactions. As a result, different structures of the heart undergo destructive changes, which causes:
- disruption of its microcirculation and vascular permeability;
- destruction of myofibrils;
- the occurrence of thromboembolism and tissue hypoxia.
The combined influence of immunopathological processes and an infectious agent mainly causes the development of acute carditis. As for the chronic process, autoimmune reactions play a key role in it.