What is nephrotic syndrome?
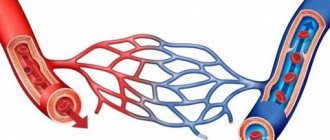
Nephrotic syndrome occurs when tiny blood vessels in the kidneys, called glomeruli, do not work properly. The glomeruli typically act as filters, removing water and waste from the blood and sending them to the bladder as urine, allowing blood cells and proteins to remain in the blood. If the glomeruli are damaged, protein can leak through the filter system into the urine.
Nephrotic syndrome includes the following symptoms:
- Albuminuria
: high levels of protein in the urine - Hypoalbuminemia
: low levels of a protein called albumin in the blood - Hyperlipidemia
: increased levels of fat and cholesterol in the blood
Nephrotic syndrome - symptoms
Symptoms of nephrotic syndrome include:
- swelling of the ankles, feet and legs
- fatigue
- loss of appetite
- weight gain
- foamy urine
The foaming that occurs due to the presence of protein in the urine is different from the bubbles that can be seen in normal urine. Foam appears in layers of small to medium-sized bubbles that do not dissipate. In contrast, normal urine may contain a single layer of larger bubbles that soon disappear.
Patients with nephrotic syndrome may notice swelling in the legs after standing for long periods of time or puffiness around the eyes after waking up. As the disease progresses, there is constant swelling of the lower extremities and other parts of the body.
Symptoms
Despite the varied etiology of the syndrome, its clinical manifestations are the same and typical.
- Proteinuria is the leading, but not the only, symptom of pathology. Most of the lost protein is albumin. Their amount in the blood decreases, fluid retention occurs in the body, which is clinically manifested by edema of varying localization and prevalence, accumulation of free transudate in the cavities. Daily diuresis is less than 1 liter.
- Patients have a typical appearance: they have a pale, pasty face and swollen eyelids, a coated tongue, and a distended abdomen. The first swelling appears around the eyes, on the forehead, and cheeks. The so-called “nephrotic face” is formed. Then they descend to the lower back, limbs and spread to the entire subcutaneous tissue, stretching the skin. Edema limits the mobility of patients, reduces their activity, complicates the process of urination, and causes constant watery eyes.
- Signs of asthenia include: weakness, lethargy, physical inactivity, dry mouth, thirst, discomfort and heaviness in the lower back, decreased performance.
- Acute nephrotic syndrome is manifested by increased body temperature and signs of intoxication.
- Degenerative-dystrophic changes in the skin - dryness, peeling, the appearance of cracks through which fluid can be released.
- Dyspeptic symptoms do not always occur. These include epigastric pain, lack of appetite, vomiting, flatulence, and diarrhea.
- Pain syndrome – headaches, myalgia and arthralgia, lower back pain.
- Severe chronic nephrotic syndrome is clinically manifested by paresthesias and convulsions.
- Hydrothorax and hydropericardium are manifested by shortness of breath and chest pain.
Forms of the syndrome:
- Persistent is a common form of the disease, characterized by a sluggish and slow course. Even persistent therapy does not provide stable remission. The outcome of the pathology is the development of renal failure.
Recurrent – a frequent change of spontaneous exacerbations and remissions, which are achieved with the help of drug therapy.- Episodic – develops at the beginning of the main disease and ends in stable remission.
- Progressive - rapid development of pathology, leading to the development of renal failure in 1-3 years.
There are also 2 types of syndrome depending on sensitivity to hormone therapy - hormone-resistant and hormone-sensitive.
Nephrotic syndrome - causes
Doctors classify the cause of nephrotic syndrome as primary or secondary.
Primary cause
The primary causes of nephrotic syndrome are conditions that affect only the kidneys. Examples of primary causes include:
- Focal segmental glomerulosclerosis (FSGS)
: In FSGS, scarring occurs in specific areas of the glomeruli. FSGS occurs more often in men than women and has a higher prevalence among African Americans. - Membranous nephropathy
: Immune complexes accumulate in the glomeruli, causing damage. - Minimal change disease (MCD)
: Damage to the glomeruli can only be seen with a very powerful microscope. MCD is the most common cause of nephrotic syndrome in children. In adults, allergies, infections, or certain medications can cause MCD. - Membranoproliferative glomerulonephritis (MPGN)
: The immune system attacks kidney cells, damaging the glomeruli. Sometimes another disease, such as hepatitis C, causes MPGN.
Secondary cause
Secondary causes are conditions that affect the entire body, leading to nephrotic syndrome. Here are some examples of secondary causes:
- diabetes
- lupus
- infections such as hepatitis B, C or HIV
- cancers such as Hodgkin's disease
Prevention
- Prevention of inflammatory kidney damage consists of timely and correct treatment of primary bacterial ( tonsillitis , tonsillitis , furunculosis , abscesses , cellulitis ) and viral diseases.
- To reduce the risk of congenital kidney pathologies in a pregnant woman, it is important to lead a healthy lifestyle during pregnancy (proper nutrition, moderate daily activity, avoidance of alcohol, smoking, drugs, medicinal exposures and harmful occupational exposures).
In the prevention of occupational toxic kidney damage in adults, preliminary and periodic medical examinations are important. It is also important to improve technological processes that eliminate/minimize the impact of chemical and physical factors on workers. Vitamin therapy and restoratives are recommended for those working in hazardous conditions. During pregnancy, from the first weeks, the issue of providing the woman with work that is not associated with hazards should be decided.
Nephrotic syndrome - diagnosis
In addition to a physical examination and history, a doctor will usually diagnose nephrotic syndrome using the following tests:
- Urinalysis
: This test looks for elevated levels of protein in the urine. - Blood test
: This test helps reveal the levels of albumin, cholesterol, and other blood components. - Kidney biopsy
: This is ordered to look for microscopic changes in the kidney. - Ultrasound: This type of imaging is used to see what the kidneys look like.
Establishing diagnosis
In diagnosis, the main thing is not to determine the clinical picture of nephrotic syndrome in a patient (to do this, it is enough to identify edema and prescribe a urine test), but to clarify its root cause. Sometimes a person has been sick for a long time (for example, with diabetes or hypothyroidism), and nephritis develops as a complication. In this case, diagnostics are also required to clarify the patient’s condition. Therefore, examination of the patient requires special attention of an experienced nephrologist.
Factors taken into account:
- History - in pediatrics it is important to know how the pregnancy and childbirth proceeded. The doctor will ask both the adult and the child about diseases of relatives, allergies, previous infections, clarify when the first symptom appeared, an acute or chronic process, and ask in detail about the course of the disease and the implementation of medical recommendations.
- Examination - mandatory measurement of blood pressure, pulse, determination of respiratory rate. In case of nephrotic syndrome, an objective examination involves auscultation of the heart and lungs, palpation of the abdomen, assessment of the condition of the skin, mucous membranes, and thyroid gland.
- Laboratory data - a general blood test will reveal possible signs of an inflammatory process in the body (accelerated ESR, leukocytosis), as well as anemia. A biochemical study will confirm hypercholesterolemia and hypoproteinemia. When assessing urine, not only the presence of protein is taken into account, but also other indicators - specific gravity, the number of blood cells, the presence of salts. If infectious diseases are suspected, the doctor will prescribe additional tests for HIV, hepatitis, sputum bacterioscopy, and ELISA.
- Instrumental methods – the main one is ultrasound. It will not evaluate the functioning of the kidney, but will identify anatomical changes and congenital anomalies. Dopplerography of the renal vessels will clarify the condition of the arteries and microcirculation disorders. Nephroscintigraphy will allow you to assess the degree of damage to the renal parenchyma.
- Morphological study - it is likely that it will be necessary to prepare microslides from tissues of various organs. In childhood, a kidney biopsy is required in cases of prednisolone-resistant form of the disease.
Based on the results obtained, the specialist, following the algorithm, must identify the underlying disease that caused nephrotic syndrome. Perhaps, to prevent an incorrect diagnosis, the doctor will consider it necessary to conduct an examination of the heart, liver, and lungs.
Nephrotic syndrome - treatment
Treatment for nephrotic syndrome will depend on the cause. However, therapy usually involves medications to treat the underlying cause as well as dietary changes.
Some drug treatments:
- Steroids
: Doctors may prescribe hormonal medications to treat MCD in children or adults. - Diuretics
: Help the body remove excess fluid and reduce swelling. - Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers
: help control blood pressure and reduce protein in the urine. - Immunosuppressive drugs
: Help with conditions such as FSGS, in which the immune system attacks the glomeruli. - Statins
: lower cholesterol levels. - Pneumococcal vaccine.
Dietary changes help treat nephrotic syndrome:
- sodium restriction
- eating less protein
- reducing intake of saturated fat and cholesterol
Therapeutic measures
The pathology is treated by urologists and nephrologists in an inpatient setting. All patients are prescribed a salt-free diet, fluid restriction, bed rest, etiotropic and symptomatic therapy.
Diet therapy is necessary to normalize metabolism, restore daily diuresis and prevent edema. Patients should consume approximately 2700 - 3000 kilocalories per day, eat five to six times a day in small portions, limit the amount of liquid and table salt in the diet to 2-4 grams. Food should be rich in proteins, carbohydrates, vitamins and potassium. Allowed are low-fat meats and fish, skim milk and cottage cheese, cereals and pasta, raw vegetables and fruits, jelly, compotes, teas. Pickles and marinades, smoked foods, spices, sweets, baked goods, fried and spicy foods are prohibited.
Etiological treatment:
- If the syndrome is a manifestation of an autoimmune pathology, glucocorticosteroids are prescribed - Prednisolone, Betamethasone. Glucocorticosteroids have anti-inflammatory, anti-edematous, anti-allergic and anti-shock effects. The immunosuppressive effect of steroids is to inhibit the process of antibody formation, the formation of the central nervous system, and improve renal blood flow and glomerular filtration.
- Hormone-resistant nephrotic syndrome of unknown etiology is treated with cytostatics - Cyclophosphamide, Methotrexate, Chlorobutin. They suppress cell division without having selective ability and affecting all organs and tissues.
- If the cause of the pathology is a bacterial infection, patients are prescribed antibiotics - Cefazolin, Ampicillin, Doxycycline.
Symptomatic therapy:
- Diuretics to reduce edema - Furosemide, Hypothiazide, Aldactone, Veroshpiron.
- Potassium preparations - “Panangin”, “Asparkam”.
- Desensitizing agents – “Suprastin”, “Tavegil”, “Cetrin”.
- Cardiac glycosides – “Strophanthin”, “Korglikon”, “Cordiamin”.
- Anticoagulants to prevent thromboembolic complications - Heparin, Fraxiparin.
- Infusion therapy - intravenous administration of albumin, plasma, rheopolyglucin to normalize blood volume, rehydration, and detoxification of the body.
- Antihypertensive drugs for high blood pressure - “Capoten”, “Lisinopril”, “Tenoric”.
In severe cases, hemosorption and plasmapheresis are performed. After the acute phenomena subside, restorative treatment is prescribed at the resorts of the North Caucasus or the Crimean coast.
Traditional medicine does not have a pronounced therapeutic effect. Experts may recommend taking diuretics and decoctions made from bearberry, juniper, parsley, and lingonberry at home.
Nephrotic syndrome is a deadly disease that often causes the development of brain, cardiac, and pulmonary dysfunction. Proper treatment of nephrotic syndrome and compliance with all clinical recommendations of specialists can normalize kidney function and achieve stable remission.
Complications
Complications of nephrotic syndrome often result from the loss of certain proteins in the urine. The body requires proteins to fight infections or control blood clotting.
Other complications of nephrotic syndrome may include:
- coronary artery diseases
- high blood pressure
- anemia, which occurs when there is a shortage of healthy red blood cells
- hypothyroidism, which occurs when the thyroid gland is unable to produce enough thyroid hormones
- temporary decrease in kidney function
Forecast
The prognosis of nephrotic syndrome can vary. It depends on what the underlying cause is as well as your overall health.
Some diseases that cause nephrotic syndrome go away on their own or with treatment. After treatment of the underlying disease, nephrotic syndrome should improve. However, other diseases can eventually lead to kidney failure, even with treatment. When this happens, dialysis and possibly a kidney transplant will be required.
If you have warning signs or think you may have nephrotic syndrome, make an appointment with your doctor to discuss your concerns.