Causes of periodontitis
There are several reasons for the development of pathology. One of the most common is the penetration of microorganisms into soft tissues. Diagnosis of periodontitis usually shows the presence of Prevotella intermedia, Porphyromonas gingivalis, Treponema denticola, Actinobacillus actinomycetemcomitans in the oral cavity.
Other causes of the disease are:
- malocclusion;
- crowded teeth;
- high tone of the masticatory muscles;
- injury to the mucous membrane;
- poor blood supply to the gums;
- lack of vitamins and minerals.
Contributing factors are considered to be dental plaque, food debris in the interdental spaces, damage to the gums by an incorrectly selected toothbrush, and smoking.
Prevention
When treating chronic periodontitis correctly, it is necessary to follow the recommendations given by the dentist. This will help the dental system maintain its function for many years. It is also necessary to remove plaque, cure caries, correct the bite and replace low-quality dentures. In addition, you should stop smoking and begin treating existing diseases.
A proper diet rich in omega-3 fatty acids will help avoid relapse of chronic periodontitis. The diet should also include solid foods (vegetables and fruits). When brushing your teeth, you should massage your gums and clean the interdental spaces and dental crowns.
Symptoms and signs
The disease has several stages. The initial stage - gingivitis - is manifested by bleeding gums. Small traces of blood when brushing your teeth or chewing solid food are rarely a cause for concern. The person thinks that he accidentally scratched the mucous membrane and does not see a doctor.
In the second stage of periodontitis, symptoms and treatment in adults are inextricably linked. A person cannot ignore warning signs. He has:
- bad breath;
- gum thickening;
- increasing spaces between teeth;
- severe bleeding.
At the third stage, tooth sensitivity to temperature changes, spicy and sweet foods occurs. The gums recede significantly, and the root necks are exposed. Along with blood, pus is released from the wounds, and the stench from the mouth becomes unbearable.
The gums swell, the teeth become loose and begin to fall out. Sometimes there is a sharp deterioration in general health: dizziness, increased body temperature, headache.
X-ray signs
X-ray studies help make an accurate diagnosis and determine the stages of periodontitis. The photographs clearly show inflammatory-dystrophic processes in the periodontium. After looking at the photo, the specialist clearly sees bone pockets, foci of destruction, and destroyed tissue.
The degree of destructive changes is determined by the clarity of the contour of the resorption zones and the presence of signs of osteoporosis. There are initial, moderate and severe stages of radiological manifestations of periodontitis.
Typically, destruction manifests itself in the cervical region, affecting the cortical lining of the interalveolar septa, and only then penetrates into deeper zones. Bone tissue destruction can occur in different parts of the alveolar processes.
Mild periodontitis is characterized by the following symptoms:
- the amount of plaque increases significantly and becomes visible to the naked eye;
- the color of the gums becomes brighter - this is due to the fact that a lot of blood flows to the gum margin and papillae, sometimes with a slight tint of blue;
- bleeding of gums increases during brushing teeth and when eating solid foods;
- X-rays show that the destruction of the jaw bone reaches the beginning of the tooth root;
- the first degree of tooth mobility is observed, with a quarter of the tooth roots becoming visible;
- The periodontal pocket fills with purulent formations and increases in size.
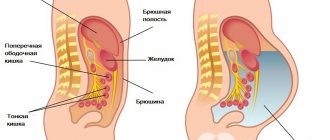
Why is periodontitis dangerous?
Inflammatory diseases of the oral cavity pose a danger that goes far beyond the scope of dentistry. When the immune system is weakened, toxic substances and bacteria easily penetrate the circulatory system and spread to organs and tissues. The body is poisoned, causing diseases of internal organs, acute respiratory viral infections, and endocrine disorders.
In the advanced stage of periodontitis, the cardiovascular system suffers. The vascular walls become thinner, and atherosclerosis develops, leading to heart attack and stroke.
Mouth infections are a serious problem during pregnancy. Due to hormones in women, the chemical composition of saliva changes and vascular permeability is impaired. The mucous membrane is often irritated and becomes vulnerable to bacteria. Bleeding, inflammation, and sores appear in the mouth. Progressive periodontitis during pregnancy can cause fetal poisoning and miscarriage.
The first sign of periodontitis is bleeding gums
Etiology of periodontitis
Periodontitis can be caused by various factors.
- Microbes.
The oral cavity of any person is inhabited by pathogenic microorganisms that do not cause harm if proper nutrition and hygiene are observed. But, if the patient constantly consumes carbohydrates and neglects to use dental floss, bacteria actively develop and gradually affect the enamel, dentin and reach the periodontal tissues. - Genetic predisposition.
If for many generations all family members have suffered from this disease, there is a high probability of adopting this predisposition. Heredity plays a big role in the development of gum periodontitis, even if a person carefully monitors hygiene and eats right. - Mechanical damage to the gums.
Tissue bruise due to negligence, an incorrect bite, in which increased pressure is applied to a specific area of the gum, or an oversized filling, due to which the tooth puts increased pressure on the gum and damages it. - Systemic diseases.
Dental diseases and periodontitis can cause pathologies not related to the oral cavity, such as vegetative-vascular dystonia, HIV, diabetes mellitus, hypertension and gastrointestinal diseases. - Autoimmune diseases.
Reduced immunity, disruption of the endocrine system, hormonal imbalances during pregnancy. - Poor quality dentist work.
Tissue damage during treatment, an unsuitable crown, incorrectly installed braces and other tissue injuries due to the fault of the doctor can provoke periodontitis.
Among the given factors are microbial causes of the development of periodontitis, and microbes are known to be transmitted from one person to another. So is periodontitis contagious? No, directly, for example, by airborne droplets or through saliva, it is impossible to become infected with the pathology, and every person has microbes that provoke the disease - even if periodontitis bacteria are transmitted from a sick person to a healthy person, the microbes will not develop without additional favorable circumstances: poor oral hygiene, gum injuries, predisposition or concomitant diseases.
Classification
Most often, periodontitis is a consequence of gingivitis - inflammation of the gums. If the process is started, it spreads deeper, affects the tooth sockets and destroys bone tissue.
According to the course of the disease, periodontitis is classified into:
- spicy;
- chronic;
- abscessing.
According to the degree of distribution, it can be focal, that is, localized in one area, and generalized, affecting all periodontal tissues.
Acute periodontitis
The acute form usually affects the periodontium of 1-2 teeth and begins suddenly with pronounced symptoms. A person suffers from:
- severe pain when chewing;
- bleeding gums;
- swelling at the site of the lesion.
If the disease is not treated in a timely manner, it becomes chronic.
This type of disease occurs due to immune disorders, thermal or chemical burns of the mucous membrane, mechanical injuries, incorrectly placed fillings, and poorly fitting dentures.
Chronic
A sluggish and prolonged inflammatory process in the oral cavity is called chronic periodontitis. It is accompanied by:
- bleeding;
- itching;
- accumulation of tartar;
- bad breath;
- mobility of teeth;
- purulent discharge;
- general intoxication.
Chronic disease has a cyclical course, characterized by periods of exacerbation and remission. The severity of symptoms depends on the severity of the pathology.
Localized
Focal or localized periodontitis is an inflammatory process affecting one or more teeth. Its peculiarity is that even if the disease progresses for a long time, it does not spread to other periodontal tissues. The disease can be acute or chronic.
With chronic periodontitis, teeth begin to loosen
The clinical picture is manifested by bleeding gums, swelling, pain during chewing, and hyperemia.
Generalized periodontitis
The generalized form is characterized by a destructive-inflammatory process that affects all periodontal tissues. The disease affects most teeth, is difficult to treat and leads to partial or complete adentia.
It is generalized periodontitis that usually causes intoxication and the development of cardiovascular and endocrine diseases.
Marginal
In case of infection of the periodontium, the dentist makes a diagnosis of marginal periodontitis. The disease occurs when bacteria penetrate deep into the soft tissue through tiny microcracks in the mucous membrane.
The dental sockets, ligaments, root system, and alveolar bone are affected. The disease is localized and affects a certain part of the periodontium. Most often occurs in a chronic form.
Aggressive form with rapid development of the inflammatory process and the formation of large periodontal pockets
Prosthetic
Prosthetic periodontitis develops due to prosthetics. Doctors identify the following reasons:
- traumatic impact of removable and fixed prostheses;
- side effects of dental procedures.
Therapeutic measures consist of eliminating the inflammatory process. To do this, they sanitize the oral cavity and try to free the prosthetic bed from the base as much as possible in order to reduce damage to the marginal periodontium.
What is an aggressive form of periodontitis?
It is distinguished by the rapid development of the inflammatory process and the formation of large periodontal pockets. There are several forms of aggressive periodontitis:
- prepubertal;
- juvenile;
- fast-flowing.
The main causes of development are considered to be immune and microbial factors. The clinical picture is characterized by the absence of acute pain with intense destruction of bone tissue.
In severe cases, the bottom of the pocket becomes more than 5 mm
Periodontitis of mild, moderate and severe severity, signs in the photo
Symptoms and treatment of periodontitis of varying severity can be seen in the photos below.
- The mild form is characterized by a decrease in the alveolar bone by a third of the height of the tooth root. The depth of the periodontal pocket reaches 3.5 mm. Affected units remain motionless.
- The average form is diagnosed when the pocket depth increases to 5 mm, the reduction in alveolar bone is half the height of the root, and tooth mobility is weak.
- In severe forms, the bottom of the pocket becomes more than 5 mm, and the alveolar bone decreases by more than half the height of the root, the teeth become loose and bleed.
In the severe stage, pus may accumulate in the gum pockets. If measures are not taken in time, this becomes the cause of an abscess.
Additional studies are prescribed:
- Schiller-Pisarev test (helps to see the inflammatory process in the gums at an early stage due to staining);
- benzidine test (helps determine the presence of pus in the periodontal pocket);
- a smear from a periodontal pocket (determines causative bacteria);
- radiography (to visualize the degree of bone tissue destruction);
- panoramic tomography (a full view of the affected jaw, mainly prescribed for suspected generalized periodontitis).
In cases where periodontitis is accompanied by general diseases, other tests may be prescribed to help determine the diagnosis and prescribe appropriate treatment.
Periodontitis in children, differences
In young patients, the main causes of periodontitis are insufficient hygiene, trauma to the mucous membrane, weak immunity, and pathogenic bacteria. As in adults, the disease occurs:
- local;
- generalized;
- sharp;
- chronic.
Symptoms of childhood periodontitis do not differ from signs of the disease in adults.
In addition to these forms, doctors distinguish two varieties that are characteristic only for children:
- prepubertal, developing during the growth of baby teeth;
- pubertal, diagnosed in adolescents.
Symptoms of childhood periodontitis do not differ from signs of the disease in adult patients. Children develop plaque on their teeth, exposed roots, bad breath, pain when chewing food, bleeding, and enlarged lymph nodes.
Periodontitis: symptoms of the disease at different stages
Generalized periodontitis of the initial stage can be stopped, and it is necessary to pay attention to symptoms such as:
- the appearance of soft plaque on the teeth;
- a clearer manifestation of gingivitis, which is characterized by gingival bleeding;
- the appearance of pain during oral hygiene procedures;
- the periodontal pocket becomes deeper;
- tooth mobility becomes noticeable;
- X-rays show the places where the process of bone destruction has begun.
Treatment of periodontitis
If there are signs of periodontitis, treatment should be entrusted to an experienced doctor. During diagnosis, the dentist:
- listens to complaints;
- clarifies the characteristics of the bite;
- checks the presence of tartar and the nature of dental plaque using special dyes;
- studies the density, color of gums and tooth mobility.
Then the patient is sent for an x-ray to identify all areas of inflammation and the depth of tissue damage. The doctor fills out a periodontogram - a card, indicating the condition of all dental units, and prescribes treatment.
Therapy depends on the severity and location of the disease. Mandatory activities are:
- removal of plaque and tartar;
- cleaning periodontal pockets;
- teeth polishing;
- mouth sanitation;
- filling carious cavities;
- elimination of prosthetic defects;
- correction of bite.
In advanced forms, surgery may be required. The operation restores damaged bone tissue and removes gum recession.
How is diagnostics carried out?
Before starting treatment, the specialist must conduct a thorough diagnosis, determine the degree and form of periodontitis. Moreover, the dentist relies not only on the result of a visual examination. You also need to take an x-ray / tomography of the patient’s jaw - the doctor will be able to assess the condition of the bone tissue (its loss), the presence of inflammation under the roots. To choose the “right” medicine, you should take a swab from the oral cavity - an analysis for anaerobic microflora, plus an analysis for antibiotic resistance, and a general blood test. After all, the dentist needs to understand what caused the pathology - “deposits” of tartar or some general disease of the body.
Some patients will have to be tested for vitamin levels, hormones, and sugar levels. If necessary, consultation and treatment will be required from another specialist - a cardiologist, endocrinologist, gastroenterologist, etc.
On a note! After treatment, tests will have to be taken again to assess the effectiveness of the prescribed drugs.
Periodontitis - treatment at home
Antibiotics are usually prescribed for treatment. The following drugs have proven themselves to be effective:
- Metranidazole;
- Syphlox;
- Tavirid.
When treating periodontitis, antibiotics are almost always prescribed.
The dosage and benefit of taking it are determined by the doctor, based on the patient’s condition. Complex therapy uses:
- mouth rinses;
- rinsing the gums with hydrogen peroxide, Miramistin, Chlorhexedine;
- applications to areas of inflammation.
At home, drug treatment can be combined with folk remedies.
Applications for gums
Gel applications help get rid of inflammation and bleeding gums. The following drugs are suitable for the procedure:
- Metrogil Denta;
- Parodium;
- Dentament.
A small portion of the gel is placed in periodontal pockets for 30 minutes twice a day. The average course is 7-10 days.
Gum massage
To improve blood flow in the affected area, regular massage is required, which you can do yourself.
- Wash your hands and treat with alcohol.
- Use your middle and index fingers to massage along the blood flow line for 10 minutes.
- Repeat sessions 2-3 times a day for a month.
Gum massage improves blood circulation
Procedures cannot be skipped. This is the only way to achieve noticeable results.
Description of the pathology - what kind of disease it is
Periodontium is the tissue surrounding the tooth root, which is responsible for holding it in the socket. In fact, this is a whole complex that includes fibers, vessels and channels involved in the process of feeding harder tissues. Periodontitis is a chronic inflammation of the gums, ligaments, and bones resulting from infection. In severe form and in the acute phase, the disease can be accompanied not only by bleeding gums, but also by purulent discharge. At the same time, the inflamed tissues move further away from the roots of the teeth, as a result of which the teeth begin to become loose and fall out if left untreated.
It is important to know! Previously, it was believed that periodontitis cannot be treated, but is simply “slowed down” in the existing phase. However, modern drugs and technologies are capable of restoring tissue volume (even bone) by 60-80% and reducing inflammation within 1 year of treatment. But you need to understand that you won’t be able to be cured in one visit to the doctor and with just one drug – it requires a comprehensive and course-based approach. As well as the active involvement of the patient in oral care and maintaining the effect obtained from treatment by a doctor.
In children, periodontitis usually appears at around 9-10 years of age. The disease affects not fully formed growing tissues, which can give an inadequate response to the slightest irritation. Sometimes the pathology develops during pregnancy and is often characterized by a latent course in the first stages. Non-surgical methods of therapy are used as treatment.
On a note! According to WHO statistics[1], people aged 35 years and older are more likely to experience the disease. However, this does not indicate a direct dependence of the pathology on a person’s age. It is always necessary to take care of your teeth and maintain oral hygiene, since the disease can occur in representatives of any age category.
Treatment of gums for periodontitis with folk remedies, review of drugs
Tampons with sea buckthorn oil relieve inflammation and draw out pus.
- Take a sterile swab.
- Soak in sea buckthorn oil.
- Apply to the sore gum for a quarter of an hour.
- Repeat therapy 4 times a day.
Beekeeping products quickly kill pathogenic flora and heal wounds. A berry-honey mixture is suitable for treatment. Combine 1 tbsp. l. viburnum and rowan and mix with May honey 1:4. Take 1 tsp. after eating, slowly dissolving in the mouth until the signs of the disease disappear.
To rinse the gums, take medicinal herbs:
- Linden blossom;
- chamomile;
- oak bark.
1 tbsp. l. pour 200 ml of boiling water over the raw materials, cover with a lid and towel and leave for 2 hours. Strain the liquid and use as a rinse every 2 hours. To increase the effectiveness of the infusion, dissolve 1 tsp in it. honey Course 10 days.
Sea buckthorn oil can be used in complex therapy
You can cope with the symptoms of periodontitis within a week by treating your gums with a special medicine. Measure out 8 drops of calendula alcohol tincture and combine with 10 drops of hydrogen peroxide. Dilute the mixture with 2 tbsp. l. boiled cooled water. Wet the swab and gently wipe the affected areas 4 times a day.
Toothpastes for periodontitis, which is better?
For periodontitis, use medicated toothpastes containing antiseptics, fluoride, vitamins, and herbal extracts. They prevent the thinning of enamel, strengthen teeth, relieve swelling and inflammation of the gums.
For treatment and prevention, dentists recommend pastes:
- Parodontax;
- Spalt Active;
- Asepta;
- Elmex Sensitive;
- Lakalut Active;
- Forest balm;
- PRESIDENT EXCLUSIVE.
Brush with a multi-level, medium-hard toothbrush with cross bristles. Perform the procedure in a circular motion, avoiding excessive pressure, for 3-5 minutes. Clean hard-to-reach places with an irrigator. Afterwards, rinse your mouth with salted water. For 200 ml of water 1 tsp. salt.
The dentist will select you a good toothpaste specifically designed for the treatment of periodontitis.
Notes
- KY Zee.
Smoking and periodontal disease // Australian Dental Journal. - 2009. - T. 54 (September). — P. 44-50. — DOI:10.1111/j.1834-7819.2009.01142.x. - Suppression of overt gingival inflammation in tobacco smokers - clinical and mechanistic considerations.. Retrieved July 8, 2016.
- Association between periodontitis and mortality in stages 3-5 chronic kidney disease: NHANES III and linked mortality study. (English). Retrieved April 6, 2021.
- Catharine Paddock PhD.
Gum disease associated with kidney disease deaths. Medical News Today (18 February 2016). Retrieved March 14, 2021. - Mark Ide, Marina Harris et al.
Periodontitis and Cognitive Decline in Alzheimer's Disease // PLOS One. — March 10, 2021. - https://www.ncbi.nlm.nih.gov/pubmed/25571822, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4488989/
- Lyamzin Sergey Sergeevich.
Periodontitis (Russian). horoshiystomatolog.ru. Retrieved October 22, 2017.
Splinting teeth for periodontitis
With periodontitis, teeth begin to change position in the row and become loose. To strengthen them, doctors use splinting. The most common option is fiberglass splinting, which is done in two ways:
- The dentist drills a groove on the inside of the teeth, inserts a fiberglass cord, and secures it with composite. The method is used for long-term therapy;
- The thread is applied superficially from the inside. The procedure is advisable as a temporary measure after treatment or gum injury.
Fiberglass helps in the initial stages of periodontitis. In advanced cases, splinting with crowns or clasp prostheses is recommended.
Diagnosis methods
Diagnosis of chronic periodontitis should be carried out by a periodontist. You may also need to be examined by an endocrinologist, hematologist, gastroenterologist, rheumatologist, cardiologist and allergist.
To prescribe the correct treatment for chronic periodontitis
it is necessary to determine the severity of changes using orthopantomography and targeted radiography, and then a periodontogram is compiled. To determine the presence of microbes in periodontal pockets, a PCR scraping is taken. To confirm the endogenous origin of the disease, it is necessary to take a blood test for sugar.
Treatment of periodontitis with the Vector device
The Vector device provides impressive results. This is a device that provides treatment with ultrasonic vibrations. Wave frequency - 25 kHz. After the course the patient experiences:
- relieving inflammation;
- removal of tartar;
- improvement of blood circulation in tissues;
- healing of damage;
- disappearance of unpleasant odor;
- stopping bleeding;
- reduction of periodontal pockets;
- strengthening teeth.
The vector effectively cleanses periodontal pockets.
A paste containing calcium is placed on the tooth surface. Ultrasonic vibrations lead to cavitation. Tartar and plaque are easily separated from crowns and roots. Cleaning is done using different attachments.
Session duration is from 40 minutes to 2 hours. The dentist prescribes the number of procedures individually.
Laser
A modern and effective way to treat periodontitis is the use of a laser beam. It provides a biostimulating effect and destroys damaged cells. The use of a laser system guarantees:
- wound healing;
- elimination of swelling;
- destruction of bacteria;
- relieving inflammation;
- stop bleeding gums.
Photodynamic, diode, and CO2 lasers are in demand in dental practice. The equipment generates beams that sterilize periodontal pockets and clean tartar. The laser LED coagulates the affected tissue and eliminates pathogenic flora.
The laser has a biostimulating effect and destroys damaged cells
Surgery
If the depth of the periodontal pocket increases and the inflammation does not go away, surgical methods are used.
- Flap surgery. The doctor makes an incision in the gum and uses a curette or laser to clean the periodontal pockets. To stimulate bone tissue growth, the cavity of the pockets is filled with osteogenic preparations and sutures are applied.
- Gingivoplasty. Removes excess tissue, evens out the height of the gums, and gives an aesthetic appearance to the oral cavity after surgical operations.
- Gingivectomy. Prescribed to reduce the depth of periodontal pockets, prevent inflammation and destruction of bone tissue. The operation is performed under local or general anesthesia.
After surgical procedures, the patient is prescribed broad-spectrum antibacterial drugs to prevent complications.
Periodontitis is easier to prevent than to treat. To do this, follow the rules of personal hygiene, regularly clean tartar, enrich your diet with foods containing calcium, give up bad habits and undergo preventive examinations at the dental clinic every six months.
Popular preventive measures
To prevent the development of periodontitis, it is important to adhere to simple prevention methods, which include the following rules:
- daily brushing of teeth in the morning and evening,
- using floss, rinsing the mouth after eating,
- proper nutrition and maintaining the proper level of immune status,
- timely treatment of diseases,
- regular preventive examinations at the dentist’s office,
- Carrying out professional teeth cleaning to remove plaque, as well as supra- and subgingival calculus.
Experts also recommend periodically massaging your gums. To do this, you need to lightly press your fingers on the gum for 5-10 minutes to stimulate its blood supply. Following these simple rules will help you avoid the disease and its negative consequences.
Remember that periodontitis cannot be treated with just one drug or method. This is always only an integrated approach, which includes various procedures in the doctor’s office - and they must be repeated or alternated every month while the main treatment is ongoing. You need to take responsibility for your health in order to prevent complications and not lose all your teeth. Therefore, in no case do not forget your “homework” - regular hygiene, following all the prescriptions of the dentist and other doctors, and fortified nutrition. Periodontitis takes a long time to be treated, but it is treated (and not “frozen” at the current stage), and successfully. And the key to an excellent result is the joint work of the doctor and the patient.