What is the disease
Chronic duodenitis is a long-term inflammation of the duodenum. Most often, the disease is infectious in nature and develops against the background of existing diseases of the gastrointestinal tract.
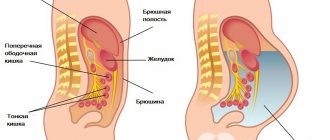
The duodenum is the initial section of the small intestine, adjacent directly to the stomach. This organ occupies one of the main places in the implementation of the secretory, motor and evacuation functions of the digestive tract.
Chronic duodenitis occurs as often as chronic gastritis. The disease is diagnosed in people of all ages. Men and women are equally susceptible to this disease.
During chronic duodenitis, there are phases of exacerbation and remission.
- During the period of remission, the disease may be asymptomatic.
- During an exacerbation, patients experience clinical symptoms of the disease.
Features of chronic duodenitis (video)
Etiology of the disease
Chronic duodenitis occurs due to ineffective treatment of gastrointestinal diseases. It is most often found in representatives of the stronger sex. It can be localized in the duodenum in the form of papillitis and diverticulitis (local), as well as in the entire intestinal area. In the latter case, they speak of widespread duodenitis. The duodenum is connected to the entire human digestive tract. Due to this, the disease spreads throughout the gastrointestinal tract, affecting nearby organs.
Classification of pathology
Depending on the cause and conditions of the disease, it is customary to distinguish primary and secondary chronic duodenitis.
- Primary chronic duodenitis can be considered as an independent disease.
- Secondary is concomitant or complicating other gastrointestinal diseases (duodenal ulcer, chronic pancreatitis, parasitic infestations, etc.)
Depending on the spread of the inflammatory process in the duodenum, the following types of duodenitis are distinguished:
- Diffuse (total) - inflammatory processes affect the entire length of the duodenum.
- Local (limited):
- proximal - the duodenal bulb becomes inflamed;
- papillitis - inflammation of the major papilla;
- distal duodenitis - characteristic changes in the mucosa are found in the final part of the organ, closer to the place of transition to the small intestine.
Depending on the depth of spread of the process and morphological changes in the mucosa, several forms of the disease are distinguished:
| Form | Sign |
| Catarrhal, or superficial | Redness and swelling of the mucous membrane. There are no ulcerative formations. |
| Atrophic | Against the background of inflammation, a decrease in the size of the villi of the mucosal epithelium (atrophy) is detected. |
| Hyperplastic or hypertrophic | Against the background of inflammation, thickening of the epithelial villi occurs due to increased cell division. |
| Ulcerative-erosive | Multiple mucosal defects (erosions) are detected. |
| Interstitial | Diffuse damage to the entire thickness of the mucous membrane is determined. |
How to treat duodenitis?
In adults, treatment of duodenitis includes several areas:
- elimination of acute inflammation
- preventing the disease from becoming chronic
- restoration of duodenal function
- normalization of digestion
Mostly treatment is carried out at home. For a speedy recovery, proper sleep, rest, diet, walks, and light physical activity in the absence of pain are necessary. It is necessary to avoid stress, quit smoking and alcohol. Such measures help normalize blood circulation in the duodenum and restore the protective properties of its mucosa.
Indications for hospitalization for duodenitis:
- exacerbation of duodenitis
- suspected tumor of the small intestine
- severe general condition of the patient, advanced cases of the disease
- inflammation of the serous covering of the duodenum (periduodenitis) and nearby organs
- presence or threat of bleeding (erosive or ulcerative form of duodenitis).
Causes
Primary form of the disease
Primary chronic duodenitis is very rare and develops, as a rule, after acute inflammation. Other reasons that cause changes in the mucous membrane of the duodenum are:
- Systematic eating disorders - eating excessively hot, spicy, and fatty foods.
- Bacteria, viruses, fungi and parasites that can enter the duodenal mucosa from other foci of infection through hematogenous and lymphogenous routes, as well as through systematic consumption of stale food. The bacteria Helicobacter pylori plays a decisive role in the development of chronic duodenitis
- Chronic autoimmune diseases. The proliferation of lymphoid tissue, swelling of the mucous membrane and its hypertrophic changes occur in response to the action of antibodies that are produced against the body’s own tissues.
- Toxic or chemical. These include alcoholic drinks, smoking, uncontrolled use of medications and other substances that cause severe irritation of the duodenal mucosa.
- Psychogenic factors or disorders of neuroendocrine regulation of the organ. In some cases, excessive mental activity leads to spasm of the small vessels of the organ. In this case, as a rule, an erosive form of pathology develops.
- Congenital features of the intestinal structure are excessive mobility or the presence of an additional loop. In these cases, the evacuation of food masses becomes difficult. Long-term stagnation of contents in the lumen of the organ can provoke chronic inflammation.
One of the reasons for the development of primary chronic duodenitis is the formation of adhesions in the abdominal cavity
- Formation of adhesions in the abdominal cavity. In this case, adhesions limit the mobility of the small intestine.
Secondary chronic duodenitis
The secondary form of pathology occurs against the background of already existing diseases of the gastrointestinal tract. A decrease in the level of production of digestive enzymes and impaired intestinal motility gradually cause a decrease in the protective functions of the duodenal mucosa. Chronic stagnation of bile leads to swelling of the papilla located in the bulbar part of the intestine and the development of inflammation in the adjacent tissues.
Diseases causing secondary chronic duodenitis:
- stomach ulcer. As a rule, it is accompanied by ulcerative processes in the duodenum;
- chronic cholecystitis, hepatitis;
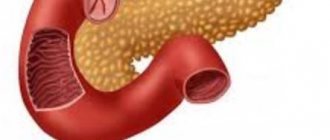
- chronic pancreatitis;
- parasitic infestations (giardiasis, amoebiasis, etc.);
- chronic renal failure;
- immunodeficiency states;
- chronic blood diseases;
- radiation injuries (most often as a result of radiation therapy for malignant tumors).
Gastric ulcer can cause the development of secondary chronic duodenitis
Prevention and prognosis
To prevent the disease, it is necessary to eat regularly and nutritiously, promptly identify parasitic diseases, treat them, as well as those in relation to the digestive organs, limit the intake of irritating and spicy foods.
Gastroduodenitis has a favorable prognosis if you follow the recommendations of a gastroenterologist on using a certain diet and maintaining a healthy lifestyle. If you do not complete the full course of treatment and do not follow the diet, chronic gastroduodenitis can develop into a stomach ulcer. In this case, more serious complications and deterioration of the patient’s condition will be noted.
Symptoms
Symptoms of chronic duodenitis mainly depend on the type of duodenitis. The following clinical forms are distinguished:
- ulcer-like;
- cholecyst-like;
- pancreatitis-like;
- gastritis-like;
- neurovegetative;
- mixed;
- latent.
| Form | Symptoms |
| Ulcer-like |
The pain symptom in chronic duodenitis is usually less pronounced than in peptic ulcer disease. In addition, with inflammation of the duodenum there is no strict seasonality; exacerbation of the disease often occurs due to errors in nutrition. |
| Cholecyst-like |
|
| Pancreatitis-like |
|
| Gastritis-like |
|
| Neurovegetative |
|
| Mixed | Characterized by a combination of symptoms of various forms of the disease. |
| Latent | Asymptomatic course of the disease. |
Forecast
When treating atrophic duodenitis, it takes time to restore the mucous membrane. It is necessary to remove the symptoms and stop the progression of the disease. If you follow your diet and lifestyle, the disease will not bother you.
If the endocrine system, nervous or immune, is disrupted, you need to go to the hospital to treat the disease, because at home it is impossible to stop the development of the disease.
Sources:
- https://academic.oup.com/ibdjournal/article-abstract/17/1/39/4631065
- https://www.niddk.nih.gov/health-information/digestive-diseases/gastritis
- https://www.ncbi.nlm.nih.gov/pubmed/361306
- https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315
- https://www.mayoclinic.org/diseases-conditions/gastritis/symptoms-causes/syc-20355807
Diagnostics
- To make a diagnosis, an endoscopic examination is necessary. Using gastroduodenoscopy, the condition of the mucous membrane is determined: the presence of edema, hyperemia, thickening or atrophy of the folds.
- For microscopy of ulcerative or atrophic areas, a biopsy (mucous area) is taken during gastroduodenoscopy. The resulting material is also examined for the presence of Helicobacter pylori bacteria.
- To determine the acidity and biochemical composition of bile, the contents of the stomach and duodenum, duodenal intubation is performed. The resulting material is examined for bacteria.
In order to diagnose concomitant diseases, the following is additionally carried out:
- blood chemistry. By changes in the level of enzymes and acids, the involvement of the liver, bile ducts or pancreas in the process is determined;
- stool occult blood test. A positive test indicates the presence of ulcerative intestinal bleeding;
An X-ray examination is carried out if for some reason it is impossible to do gastroduodenoscopy
- X-ray examination. If the patient refuses gastroduodenoscopy, an X-ray examination of the stomach and intestines is performed using a contrast agent.
Treatment
Drug therapy
Patients with chronic duodenitis are prescribed drug therapy, the purpose of which is:
- reduction of clinical symptoms of the disease;
- prevention of exacerbation frequency;
- prevention of complications of the disease (the appearance of ulcers on the mucous membrane, inflammation of the pancreas or biliary tract).
The selection of medications is carried out taking into account the form of pathology and concomitant diseases.
If an ulcerative form of the disease or a primary version of chronic duodenitis is diagnosed, and Helicobacter pylori bacteria are found in the gastric secretions, then the following treatment is indicated:
- Decreased secretory activity of the stomach. For this purpose, proton pump inhibitors (Omeprazole or Esomeprazole) are prescribed. These drugs effectively suppress the production of hydrochloric acid. Treatment with these drugs is carried out not only during exacerbation of the disease, they are also prescribed as maintenance therapy.
- Antacids, drugs that reduce the acidity of gastric juice, and also protect the mucous membrane of the stomach and duodenum from its damaging effects (Almagel, Phosphalugel and others).
- Antacids with adsorbing properties - bismuth preparations (De-nol and analogues). In addition to the protective effect, bismuth preparations also have an antibacterial effect.
- To eliminate Helicobacter pylori bacteria, a weekly course of antibiotics (Metronidazole, Clarithromycin and Amoxicillin) is prescribed.
The secondary chronic form of the disease occurs against the background of concomitant diseases. Therefore, drugs are selected taking into account what pathology caused inflammation of the duodenum. There are two main types of these pathologies.
Diagram of duct arrangement
With increased motility of the gallbladder, bile ducts and duodenum, patients are bothered by severe pain and frequent loose stools. Vomiting is often associated. Food is poorly digested.
- To eliminate severe pain, analgesics are prescribed in the form of injections:
- Analgin;
- Tramal;
- antispasmodics - for moderate pain.
- To eliminate spasm of the smooth muscles of the intestine and ducts, which causes increased motility of these organs, a solution of Atropine or Platyphylline is prescribed intramuscularly.
- To improve food absorption, enzymes and antiemetics (Cerucal, Bimaral) are prescribed.
Just as in the treatment of ulcerative forms of pathology, the following are prescribed:
- antacids, which protect the intestinal mucosa from the aggressive effects of excess bile;
- antibiotics, nitrofurans and sulfonamides to eliminate Helicobacter pylori bacteria;
- proton pump inhibitors;
- prebiotics to restore intestinal flora.
With a decrease in motility of the biliary tract and intestines, stagnation of bile and intestinal contents develops. The absorption of food and its evacuation into the small intestine are impaired. The goal of treatment for this form is to improve the contractile function of the digestive organs and eliminate congestion, against the background of which inflammation of the duodenal mucosa develops.
The following drugs are prescribed:
- Duspatalin - selectively relieves spasm of the smooth muscles of the intestine and ducts, but does not reduce its contractile activity.
- Motilium - improves the evacuation of food masses.
- Enzymes.
- Allahol or Cholenzym - have a choleretic effect.
- Salicylic acid preparations and mineral waters increase the liquid part of bile.
- Laxatives (for constipation).
The total duration of the treatment course is 1 month.
An additional method of unloading the contents of the duodenum and gall bladder is duodenal intubation. During this procedure, a three-stage evacuation of food secretions from the intestine is performed, then bile from the bladder and then from the ducts.
Treatment of the disease is always carried out against the background of dietary nutrition.
Drugs to treat the disease (gallery)
Metronidazole eliminates Helicobacter pylori bacteria
Cerucal improves food absorption
Analgin relieves pain
Cholenzym has a choleretic effect
Motilium improves the evacuation of food masses
Duspatalin relieves spasms of intestinal smooth muscles
Diet
Treatment of exacerbation of chronic duodenitis is best done in a hospital setting. This will be a kind of guarantee that the patient will strictly adhere to the prescribed diet. In addition, patients need a therapeutic and protective regime.
The concept of “therapeutic and protective regime” includes complete cessation of smoking and drinking alcohol.
The main role in reducing inflammation belongs to adherence to the principles of dietary nutrition:
- Meals should be fractional - 5-6 times a day.
- The temperature and consistency of food are as gentle as possible.
- The diet is selected depending on the form of the disease and concomitant pathology.
In case of chronic duodenitis, regardless of concomitant pathology, the following products are excluded:
- canned food;
- smoked meat;
- cold drinks and ice cream;
- alcohol;
- hot seasonings - pepper, mustard;
- onion and garlic;
- hot drinks, coffee and strong tea.
Recommended dishes:
- milk soups;
- vegetable puree soups cooked in meat broth. To prepare broths, lean varieties of meat and fish are used;
- vegetable purees from pumpkin, potatoes, zucchini, carrots and beets;
- non-acidic fruits, preferably baked;
- dairy products - cottage cheese, sour cream, milk, cheese;
- lean meat, chicken and boiled fish;
- drinks: tea with milk, diluted vegetable and fruit juices, rosehip decoction.
Depending on the clinical form of chronic duodenitis, one or another diet is prescribed:
- For ulcerative variants, as well as in combination with chronic enteritis, diet No. 1.
- For gastritis due to secretory insufficiency - diet No. 2.
- When combined with diseases of the liver and biliary tract - diet No. 5.
- When combined with pancreatitis - diet No. 5p.
Products prohibited for duodenitis (gallery)
Coffee
Onion and garlic
Alcohol
Ice cream
Smoked meat
Canned food
Diet No. 1
This diet excludes foods that stimulate the production of gastric juice. As part of this nutrition system, patients with chronic duodenitis are allowed to:
- Boiled eggs, no more than two per day.
- Yesterday's baked goods made from wheat flour, crackers and cookies.
- Low-fat dairy products - cottage cheese, sour cream, milk.
- Any vegetables, boiled and pureed.
- Buckwheat, oatmeal, semolina and rice porridge.
- Ripe sweet fruits (bananas, apples and pears).
- Steamed cutlets made from lean meat, fish and chicken.
- Soups with vegetable broth.
- Milk soups with well-cooked cereals.
- Vegetable puree soups made from carrots, cauliflower, potatoes, pumpkin, zucchini and green peas.
Prohibited on this diet are foods that cause increased formation of hydrochloric acid in the stomach:
- Fresh cabbage, radish, radish.
- Millet and corn cereals, brown and brown rice.
- Rye flour products and fresh baked goods.
- Peas and red beans.
In case of erosive form of duodenitis, cream soup and vegetable salads are allowed
Sample menu:
- breakfast - rice porridge from glutinous cereals, tea with milk and cookies;
- second breakfast – baked apple or banana;
- lunch – vegetable puree from zucchini and potatoes, steamed chicken cutlet, tea with milk;
- afternoon snack - jelly with crackers;
- dinner - milk noodle soup, boiled beet salad with sour cream, rose hip decoction;
- 2 hours before bedtime – low-fat cottage cheese with sour cream, dried fruit compote.
Diet No. 5
When chronic duodenitis is combined with diseases of the biliary tract and pancreas, diet No. 5 is prescribed. The goal is to normalize bile secretion, reduce the load on the liver and pancreas.
Authorized products:
- “yesterday’s” wheat and rye bread;
- boiled meat and fish from low-fat varieties;
- fresh vegetable salads from cabbage, carrots, green peas;
- boiled and baked vegetables (pumpkin, zucchini, potatoes, carrots);
- milk and cereal soups;
- porridge from oatmeal and buckwheat, as well as pilaf.
Diet No. 5 excludes:
- hard-boiled and fried eggs;
- meat and fish broths;
- legumes;
- mushrooms;
- cocoa and chocolate;
- fat cottage cheese and sour cream;
Butter and cheese are limited. Soft-boiled eggs - no more than two per week.
Sample menu:
- breakfast – 1 egg omelet, low-fat cottage cheese with honey, compote;
- second breakfast – fruit salad with yogurt;
- lunch - vegetable puree soup in water, boiled potatoes with steamed fish meatballs;
- afternoon snack – a glass of low-fat kefir with cookies;
- dinner - boiled noodles with a steamed cutlet of lean meat, tea with breadcrumbs;
- 2 hours before bedtime – a glass of jelly.
Diet No. 5p
Authorized products:
- vegetarian pureed soups (carrots, potatoes, pumpkin, etc.);
- dried or yesterday's bread;
- unsweetened dry biscuits;
- lean meat: rabbit, chicken, turkey;
- low-fat dairy products;
- pureed and semi-viscous porridge (oatmeal, buckwheat, semolina);
- boiled vegetables (potatoes, carrots, beets, zucchini, pumpkin);
- non-acidic fruits and berries
- tea with lemon, rosehip infusion, diluted juices.
Prohibited products:
- soups with meat broth, milk soups, cabbage soup;
- fresh bread, puff pastry and pastry products;
- fatty meats (pork), fried and salted fish, caviar, canned food;
- fatty dairy products;
- legumes;
- radish, turnip, radish, onion, garlic, sorrel, spinach, sweet pepper, mushrooms;
- grapes, dates, figs, bananas, confectionery, chocolate, jam, ice cream;
- coffee, cocoa, carbonated and cold drinks, grape juice.
Sample menu:
- First breakfast: boiled meat, oatmeal, unsweetened tea.
- Second breakfast: steamed omelette, rosehip decoction.
- Lunch: vegetarian vegetable soup, steamed chicken cutlet, boiled potatoes, pureed dried fruit compote.
- Afternoon snack: cottage cheese, tea.
- Dinner: boiled fish, apple puree, tea.
- At night: kefir.
Functions of the duodenum
The duodenum is the most important component of the digestive system. This organ is responsible for cavity digestion. It is in the duodenum that the final stage of the breakdown of useful substances takes place.
The duodenum is also responsible for the production of hormones. It is the walls of the duodenum that produce the hormone enterogastron. It is responsible for suppressing excessive secretion of gastric juice. This hormone also relaxes the walls of the stomach. The duodenum also secretes equally important hormones:
- cholecystokinin;
- pancreozymin;
- secretin.
These hormones are responsible for the healthy functioning of the gallbladder and pancreas. They also stimulate the intestinal glands, which are especially active in stimulating intestinal motility. Hormones secreted by the duodenum also play an important role in the functioning of the nervous, endocrine and cardiovascular systems.
Surgical treatment of the disease
This treatment method is used in cases of ineffective conservative therapy.
Surgical treatment is indicated for the following conditions:
- Spasm of the sphincter of the bile duct, which opens into the lumen of the duodenum. In this case, an endoscopic incision is made into the smooth muscle of the sphincter - papillosphincterotomy.
In case of spasm of the sphincter of the bile duct, papillosphincterotomy is performed
- The presence of adhesions. In this case, they are excised. Further tactics depend on how well the motor function of the duodenum is preserved.
- Impaired contractility of the smooth muscles of the duodenum, which could not be cured with medications. In this case, an operation is performed - the creation of an intestinal anastomosis.
- The presence of an additional loop and associated excess mobility. In this case, an operation is performed to fix the loop to the mesentery.
After such operations, stagnation of intestinal contents is eliminated and food evacuation is improved. Symptoms of chronic inflammatory process gradually disappear.
Other treatments
Physiotherapy
To improve the motility of the intestinal tract, therapeutic exercises are recommended.
Important! To achieve the desired effect, you must perform exercises regularly (1-2 hours before meals).
The following types of exercises are recommended:
- Alternately raising straight legs from a lying position 7–8 times.
- Bending one and the other leg at the knee while lying on your back 7 to 8 times successively.
- In a standing position, take a dumbbell in one hand and lower it along your body. As you inhale, raise your hand from the dumbbells above your head, and as you exhale, lower it back down. Perform alternately for each hand 10 - 12 times.
- Exhale squats with dumbbells. During a squat, your arms are spread to the sides. As you inhale, return to a standing position.
- While standing on all fours, straighten your knees while inhaling. During this movement, the leg rests on the toe. Alternately straighten each leg 7 - 8 times.
- In a knee-elbow position, slowly move your legs so as to bring your knees closer to your elbows. The back is rounded during this movement. Repeat 5 - 6 times.
- While sitting on a chair, while inhaling, tilt your torso forward, trying to bring your chest as close to your legs as possible. As you exhale, slowly return to the starting position.
- While standing, perform rhythmic turns of the body to the right and left at least 10 times.
There are quite a few exercises to stimulate intestinal motility; your doctor will help you choose the right ones. The result will appear gradually, after several weeks of regular exercise.
Set of exercises (video)
Treatment with folk remedies
The use of folk remedies effectively complements drug therapy and a set of exercises. The purpose of this therapy is:
- suppression of hydrochloric acid secretion;
- acceleration of erosion healing;
- destruction of harmful bacteria;
- stimulation of bile duct motility.
For this purpose the following is prescribed:
- Decoctions of chamomile and yarrow. The herb is poured with hot water and infused for half an hour. Take 100 ml decoctions half an hour before meals.
A decoction of chamomile and yarrow is recommended for the erosive form of chronic duodenitis
- Aloe juice has good wound healing properties. The fresh leaf of this plant must be crushed and the juice squeezed out. Take half a teaspoon several times a day an hour before meals.
- Natural honey (1 tsp an hour before meals) has pronounced antimicrobial and wound-healing properties.
Honey has antimicrobial and wound-healing properties
- When bile duct motility decreases, corn silk is prescribed. This remedy stimulates the emptying of the gallbladder and reduces the viscosity of bile. The preparation is similar to chamomile decoction.
Folk remedies
Folk remedies for the atrophic type of the disease are very effective in combating symptoms. They are even prescribed in clinics. Traditional medicine often becomes one of the components of complex therapy.
Important: It is believed that herbal infusions are the safest for self-treatment. However, it is not. If the patient has diseases accompanying duodenitis, such as a stomach ulcer, some preparations may be harmful. That is why it is not recommended to prescribe herbal treatment on your own. It is better to consult a doctor who will make a prescription based on the diagnostic results.
There are several methods that are especially recommended for use by patients with duodenitis:
- Plantain . The juice of this plant in the amount of 3 tablespoons should be mixed with a tablespoon of honey. You need to take the product before meals three times a day in the amount of one tablespoon. This product has an enveloping and healing effect.
- Chamomile . This plant can soothe the tissues and mucous membranes of the gastrointestinal tract, as well as relieve symptoms of heartburn and reflux. It is enough to pour half a glass of dried chamomile with one liter of boiling water and let the broth brew and cool. You need to drink this herbal decoction twice a day, one glass.
- St. John's wort . The drug is indicated for the treatment of various stages of duodenitis. Two tablespoons of dried St. John's wort should be poured with a glass of boiling water and left for half an hour. You need to drink the strained infusion three times a day, one-third of a glass.
There are many other methods to combat duodenitis. Be sure to consult with your doctor which one is right for you, and feel free to fight your illness.