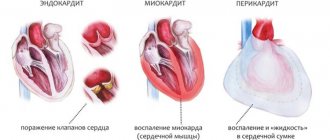
Pericarditis is an inflammatory disease of the outer lining of the heart (pericardium), which can be infectious or non-infectious.
This pathology occurs as a complication of various organic lesions or against the background of injuries, and can also be a manifestation of some autoimmune diseases.
Pericarditis can cause the development of deadly complications, such as cardiac tamponade (compression of the heart by the increasing accumulation of fluid in the pericardial cavity), heart failure!
From an anatomical point of view, the pericardium is a two-layer sac that protects the heart from external influences. The inner and outer layers (sheets) of the pericardium consist of tissue penetrated by nerve endings, as well as blood and lymphatic vessels.
The “lubricant” that promotes normal heart function is a small amount of serous fluid in the pericardial cavity.
1 Ultrasound of the heart for pericarditis
2 ECG for pericarditis
3 Ultrasound for pericarditis
Accumulation of effusion due to exudative pericarditis?
Exudative pericarditis acts as a clinical manifestation or complication of certain cardiac, pulmonary and other organ diseases. It is typical for effusion pericarditis to go through the stage of dry pericarditis in most cases, but sometimes the accumulation of exudate in the pericardial fissure begins from the very beginning. With exudative pericarditis, the hemodynamic value of the effusion is determined by the rate of entry and volume of fluid, as well as the adaptive ability of the outer lobe of the pericardium:
- With the slow accumulation of exudate, the volume and stretching of the pericardium slowly increases, so for a long time the increase in intrapericardial pressure and changes in intracardiac hemodynamics are practically unnoticeable. With pericardial effusion, up to 1-2 liters of fluid can accumulate near the heart, which begins to put pressure on the nerve pathways and organs adjacent to the heart.
- If the accumulation of exudate occurs quickly or the pericardium cannot increase its volume, then the pressure in the pericardial region quickly increases and cardiac tamponade is formed.
conclusions
The pericardium is the sac surrounding the heart, which is made up of different layers. The main function of fibrous is protective, serous is the production of shock-absorbing fluid. The pericardial sac protects the organ from displacement, injury and penetration of microorganisms. The main diseases of the pericardium: exudative inflammation with different types of effusion, armored heart, tumors and cysts.
The doctor’s professionalism will help you choose the best treatment method: conservative (use of medications) or surgical (minor surgical intervention - puncture or full-fledged operation).
Types of exudative pericarditis
According to clinical manifestations, this disease can be divided into:
- acute exudative pericarditis, lasting no more than 6 weeks;
- subacute exudative pericarditis, lasting from 6 weeks to six months;
- chronic exudative pericarditis, lasting over six months.
The disease can also be classified according to the characteristics of the inflammatory fluid:
- serous exudate, formed in the early stages of the disease, contains albumin in addition to water;
- in serous-fibrous effusion there are many fibrin threads;
- in the hemorrhagic exudate formed in case of severe damage to blood vessels, there are many red blood cells;
- purulent effusion contains an excess of leukocytes and particles of dead tissue;
- putrefactive effusion occurs when anaerobic microflora enters it;
- cholesterol exudate contains a lot of lipids.
This disease can be classified according to the reasons that caused it:
- non-infectious (mechanical, toxic, immunogenic);
- infectious (specific and nonspecific);
- idiopathic.
Causes of effusion pericarditis
What is characteristic of exudative pericarditis is that it rarely appears as an independent pathology, but more often accompanies polyserositis or another disease that affects the pericardium.
Nonspecific forms of infectious effusion pericarditis are usually caused by pneumococcus, streptococcus and staphylococcus, as well as viruses (Coxsackie, ECHO, influenza). Pathogens of typhoid fever, tuberculosis, tularemia, smallpox, and brucellosis can lead to a specific form Less common are fungal (histoplasmosis, candidiasis), rickettsial and protozoal (echinococcosis, amebiosis) forms of pericardial damage.
Tuberculous pericarditis most often forms when mycobacteria penetrate into the pericardium from the tracheobronchial and mediastinal lymph nodes. With infective endocarditis, rupture of a lung abscess, against the background of immunosuppressive therapy and after heart surgery, purulent effusion pericarditis can develop.
Non-infectious exudative pericarditis can result from:
- mesothelioma – a malignant tumor of the pericardium, carcinomatosis (cancerous contamination) of the pericardium;
- metastases and invasions in breast cancer, lung cancer, lymphoma, leukemia;
- end-stage uremia in chronic renal failure;
- serum sickness and other allergic processes;
- irradiation of the mediastinum;
- diffuse connective tissue diseases (systemic lupus erythematosus, rheumatism, rheumatoid arthritis).
Effusion pericarditis can begin in the early stages after myocardial infarction - this is the so-called epistenocardial pericarditis, as well as in cases of impaired cholesterol metabolism (xanthomatous form) and hypothyroidism. There are also many cases where the etiology of pericardial effusion cannot be determined.
The following events can also be the causes of exudative pericarditis:
- chest injuries (compression, bruises, penetrating wounds);
- Iatrogenic injuries (arising during medical procedures) are most often possible after thoracic operations;
- perforation of the esophagus;
- severe intoxication (uremia);
- pneumonia;
- radiation damage;
- severe MI, rupture of dissecting aortic aneurysm.
When exudative pericarditis develops against the background of the underlying disease, most often its severity begins to prevail, and its symptoms overshadow the signs of the root cause of the disease.
The appearance of pericarditis in childhood
In rare cases, pathology is diagnosed even in a newborn. The cause of the disorders may be abnormal development of the fetus in the womb. In an infant, pericarditis is provoked by streptococcal and staphylococcal infections. In older children, symptoms of the disease are detected against the background of viral invasions, arthritis, arthrosis and other abnormalities associated with the connective tissues of the body. Excess fluid in the pericardium can also be caused by:
- hereditary factors;
- hormonal disorders;
- thyroid dysfunction;
- oncology of cardiac structures;
- blood diseases;
- lack of vitamins;
- a side effect of certain medications.
Symptoms of effusion pericarditis
The rate at which fluid accumulates in the pericardial cavity is more important than its quantity.
If the effusion accumulates slowly, then the body has time to partially adapt, so even a significant volume (exceeding a liter) may not cause any special complaints or worsening of the patient’s condition. But if the exudate accumulates rapidly, then a critical situation may occur within a few hours.
Subjective complaints of patients and signs of exudative pericarditis can be as follows:
- chest pain, especially worse when swallowing;
- hiccups, hoarse voice, cough, which are caused by compression of the respiratory tract, nerve trunks and diaphragm by accumulated fluid.
With effusion pericarditis, shortness of breath in a supine position increases sharply, sometimes reaching suffocation. In an effort to reduce it, patients instinctively sit in a characteristic position - resting their hands on their knees or a pillow placed on them.
The examination reveals the following symptoms indicating pericardial effusion:
- the upper half of the body and the skin of the face take on a pale appearance with a bluish tint, in addition, swelling appears;
- On auscultation, muffled heart sounds are noted;
- the neck veins swell;
- the boundaries of the liver increase;
- the presence of tachycardia, paradoxical pulsation also sometimes appears - when the pulse weakens during inspiration;
- X-rays show a decrease in cardiac pulsation, expansion of the cardiac shadow, straightening of the cardiac arches - a typical picture called a “triangular heart”.
If rapid formation of exudate occurs between the pericardial layers, even in moderate quantities (no more than 300 ml), then life-threatening cardiac tamponade can quickly develop. The heart is compressed by the rapidly accumulated fluid, which makes its motor function very difficult, cardiac output decreases, which can quickly cause acute heart failure and death.
Having reached cardiac tamponade, effusion pericarditis exhibits the following symptoms:
- all symptoms of pericarditis (shortness of breath, edema, developing into ascites) become sharply more pronounced;
- to them is added a disturbance of consciousness (fear of death, depression or, conversely, excitement);
- in the absence of urgent medical care, loss of consciousness occurs, collapse, ending in death.
Diagnostic signs
Diagnostic examination methods are available in therapeutic hospitals:
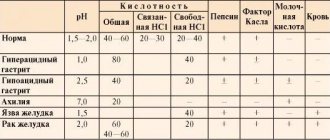
- In the blood test, leukocytosis and a change in the formula, accelerated ESR, are observed.
- Biochemical tests show an increase in total protein. Changes in the balance of protein fractions, c-reactive protein, increase in the enzyme creatine phosphokinase, liver transaminases.
- X-ray examination: dry pericarditis has no manifestations. The exudative form is accompanied by a characteristic silhouette of a cardiac shadow (expansion in all directions resembles a house with a chimney). With adhesive pericarditis, a “small” round heart is determined, and mobility is reduced. When calcium salts are deposited, the picture is called an “armored heart.”
- On the ECG, typical changes are most often absent. In acute pericarditis, infarction-like manifestations are possible, this indicates the spread of inflammation from the pericardium to the anterior wall of the myocardium.
- Phonocardiography allows you to record heart murmurs. With pericarditis, it registers extraneous noises that do not come from the heart cavity.
- Echocardiography has the greatest ability to detect fluid in the pericardial cavity, thickening and changes in the layers.
- A puncture of the pericardium is performed with examination of the resulting fluid and bacterial culture.
Diagnostics
In the case of effusion pericarditis, the patient's anterior chest wall swells slightly, slight swelling is observed in the precordial region, a weakening of the apical impulse or its complete disappearance is noted, dullness of the percussion tone at the angle of the left scapula, and the relative and absolute boundaries of cardiac dullness expand.
A drop in blood pressure, an increase in central venous pressure, paradoxical pulsus and tachycardia with transient arrhythmia indicate the appearance of cardiac tamponade.
To diagnose effusion pericarditis and distinguish it from other heart diseases (acute myocarditis, acute MI), in addition to examination, it is necessary to carry out:
- ECG. An ECG with effusion of pericarditis shows a reduced amplitude of all waves. Multislice CT can confirm thickening of the pericardial layers and the presence of pathological effusion.
- EchoCG. This is the most accurate and specific way to diagnose pericardial effusion, especially with a small volume of fluid. An echocardiogram is able to visualize echo-negative, i.e., free space between the pericardial layers, thickening of the pericardium, as well as diastolic separation of the epicardium and the parietal plate. In severe cases, abnormal heart contractions are recorded, and with tamponade, diastolic collapse of the right chambers of the heart is detected.
- Chest X-ray . With a significant volume of exudate, the radiograph shows a smoothing of the cardiac contour and an increase in the shadow, a weakening of the pulsation of the heart and a change in its shape with a prolonged excess of exudate to a triangular shape.
- Multislice computed tomography.
- Perform a pericardial puncture , after which the pericardial fluid is examined, performing general clinical, cytological, bacteriological and analysis for LE cells and ANAT. If necessary, a pericardial biopsy is performed to morphologically examine the resulting tissue sample.
What is the pericardium and what function does it perform?
The pericardium is a serous (consisting of connective tissue) closed sac where the heart is located. In shape, it resembles an obliquely cut cone, the wide part of which is firmly attached to the center of the diaphragm (the demarcation between the chest cavity and the abdomen, running along the bottom of the ribs). The upper edge of the structure ends at the angle of the sternum (it feels like a slight bulge when you slide your fingers down from the hollow between the collarbones).
Structure
The wall of the pericardial sac is double, it includes:
- The outer layer (fibrous), consisting of coarse collagen fibers (in the body, these structures are used in places where the greatest strength is required). In addition to the heart, this membrane also covers the vessels connecting to it.
- Inner layer (serous, formed by a thinner layer of connective tissue). Includes two sheets:
- underlying (subserosal), consists of thin fibers of connective tissue;
- directly serous (covered with mesothelium - a layer of cells with thin outgrowths-cilia, they are able to move the liquid part of the lymph into the space between the sheets of the pericardium), includes two plates: parietal (fused with the outer fibrous layer);
- splanchnic (the outer shell of the heart, fused with the myocardium).
A pericardial gap is formed between the parietal and splanchnic plates. It is filled with serous fluid (close in composition to blood, without red blood cells and other formed elements) that has moved due to the work of the mesothelium (15-20 ml in an adult). It plays the role of a lubricant, allowing the outer and inner layers of the pericardium to slide freely during different phases of the organ’s work.
If the pericardial sac is affected by an inflammatory process, the amount of contents increases. Fibrin, a special protein responsible for the formation of blood clots (while in the blood), may fall out on the inner surface of the leaves. Here it forms adhesions (lumps between the plates that glue them together and prevent them from sliding along each other).
Liquid can also accumulate in bags (physiological expansions of the gap between the plates of the serous layer, which is part of the inner layer). There are two of them: transverse (at the base of the heart, on top) and oblique (located on the lower side of the pericardial sac facing the diaphragm).
The pericardium is conventionally divided into several parts:
- anterior (adjacent to the sternum - the flat bone on the front surface to which the ribs are attached);
- lower (attached to the tendon center of the diaphragm, adjacent to the esophagus, thoracic aorta, azygos vein, main bronchi);
- lateral (right and left), they come into contact with the pleura, which envelops the lungs.
From each of these parts, ligaments extend to the surrounding organs - dense bundles of connective tissue fibers that ensure a stable position of the pericardium and the organ it protects in the chest cavity. Thanks to this fixation system, the heart will not jump out of the chest even in extreme fright.
Main tasks and mechanisms for their implementation
The main functions of the pericardium and the elements involved are presented in the table.
| Task | Executive structure | Implementation mechanism |
| Heart fixation | Ligaments and outer (fibrous) membrane | One end of the ligament is fixed on the pericardium, the other - on nearby organs: sternum, diaphragm, ribs, trachea, spine, large bronchi and aorta |
| Depreciation | Ligamentous apparatus | The dense connective tissue that forms the basis of the ligaments is capable of stretching slightly and returning to its original state. This ensures a reduction in shocks coming from outside (for example, a fall) |
| Fluid in the pericardial cavity | By ensuring the sliding of the sheets, it somewhat protects the heart from displacement during sharp turns. | |
| Protection | Multilayer structure of the pericardial sac, pericardial fluid | Mechanical barrier to external damage. In addition, it makes it difficult to damage the myocardium and endocardium by microorganisms from the chest cavity |
| The liquid contains bactericidal substances and cells that can exhibit immunological activity (destroy the pathogen) | ||
| Preventing myocardial overstretching with blood | Dense collagen fibers of connective tissue within the layers of the pericardium | A fairly rigid external frame prevents the muscles from dangerously stretching and deforming |
| Protection of surrounding organs | The pericardial cleft and the fluid contained in it | The apical impulse (the movement that the sharp apex of the heart makes with each contraction) works no worse than a jackhammer. As the layers of the pericardium slide along each other, they weaken the intensity and amplitude of movements, which protects the ribs from destruction |
Treatment of exudative pericarditis
After the diagnosis of effusion pericarditis is made, its treatment continues under the supervision of a doctor in a hospital. Drug therapy is mainly used, although in some cases surgery is required.
It is impossible to cure pericarditis with only one therapeutic method (especially a folk one).
If pericarditis is infectious in nature, then antiviral and antibacterial therapy is required - in accordance with the specific pathogen.
In case of oncological causes, radiotherapy and chemotherapy are used.
If effusion of pericarditis was caused by surgical complications or chest trauma, then surgical treatment is required in such a case. Cardiac tamponade always requires urgent treatment, since the severity of the condition rapidly increases. In this case, the following activities are carried out:
- potent (including narcotic) analgesics are urgently administered;
- as part of anti-shock therapy, large doses of corticosteroids are given;
- loading doses of diuretics;
- the patient is given oxygen-enriched breathing mixtures;
- a puncture of the pericardium is performed with the insertion of a needle into the pericardial cavity and pumping out the exudate - this should be done slowly so that cardiac weakness does not sharply worsen.
Drug treatment
Its goal is not only to get rid of pericarditis itself, but also from the causes that caused it. This includes:
- Non-steroidal anti-inflammatory drugs, of which ibuprofen, which has fewer side effects, is most often used. If the background for pericarditis is ischemia, then aspirin with diclofenac is chosen. Indomethacin is considered a third-line drug.
- Glucocorticosteroids (prednisolone) are used for advanced disease.
At the same time, the root cause is treated with cytostatic, antibacterial and anti-tuberculosis drugs. Hemodialysis can be used to cleanse the blood.
Surgery
If a very large amount of exudate is formed, it is pumped out by puncturing the pericardium and inserting a hollow needle into the pericardial space. This operation is considered safe.
If drug treatment is ineffective, it is necessary to resort to thoracotomy (dissection of the chest and resection of the pericardium without affecting the areas of nerve passage). With such operations, the mortality rate does not exceed 10%.
Methods of assisting a patient with hydropericardium
A person with hydropericardium must be hospitalized in a hospital. The motor mode, as well as the consumption of salt and water, are limited as much as possible. Treatment is primarily aimed at eliminating the cause of the effusion. If it is congestive heart failure, then diuretics are used. Anti-inflammatory therapy is required.
Drugs that are indicated in the presence of effusion:
Furosemide;- Torasemide;
- Ibuprofen;
- Prednisolone or Methylprednisolone;
- Antibiotics (depending on the sensitivity of the identified pathogen).
In cases where drug treatment is ineffective, or hemopericardium has formed, as well as in urgent conditions, surgical intervention is performed - pericardiocentesis.
The procedure consists of puncturing the chest between the xiphoid process and the left costal arch (access to the pericardial space) and actively collecting fluid under ultrasound or radiography guidance. The selected substance is sent for microscopic, microbiological and cytological laboratory testing, which makes it possible to differentiate the nature of the effusion and adjust treatment (if necessary).
If the disease has a recurrent course and repeated puncture is not sufficiently effective, the issue of performing pericardiectomy is considered. Surgery involves removing the heart sac, which frees it from compression.
Complications of exudative pericarditis
The most common complication from exudative pericarditis is cardiac tamponade, observed in 40% of cases. The fluid accumulated between the layers of the pericardium puts pressure on the heart, preventing it from contracting normally.
In approximately 30% of cases, pericarditis causes supraventricular tachycardia or paroxysmal atrial fibrillation, but this requires inflammation to spread to the myocardium.
A special case of complication is a change in the type of pericarditis into a chronic or constrictive form.
When it becomes chronic, exudative-adhesive pericarditis develops, in which the symptoms of the disease do not completely disappear, but become less acute. Massive adhesions or individual adhesions are formed between the outer (parietal) and inner (visceral) sheets of the cardiac shirt. In the most severe cases, the pericardial cavity can become completely filled with adhesions, leading to a permanent decrease in cardiac output. In this case, only surgical treatment is possible.
Treatment of fluid in the pericardial cavity
Treatment procedures are divided into surgical and medical.
Medicines used for pericarditis:
- antibacterial drugs (Amoxicillin containing clavulanic acid, Cephalosporin, Macrolide);
- diuretics "Furosemide", ethacrynic acid;
- the use of anti-inflammatory drugs, both steroidal and non-steroidal (Ibuprofen, Indomethacin) is indicated;
- antifungal and antiparasitic agents;
- tuberculous pericarditis requires the appointment of “Rifampicin”, “Isoniazid”;
- “Aspirin” is actively used for various types of diseases;
- immunosuppressive drugs (for autoimmune type of pathology).
Other medications are also used, their choice will be dictated by the immediate cause of the disease. And the main goal of treatment is to combat the underlying pathology.
Surgery comes to the rescue in emergency cases, for example, when tamponade develops. In this situation, using a special device, excess fluid is sucked out from the pericardial cavity.
To treat patients with a “shell heart,” surgery is necessary to remove the calcified capsule that has formed around the myocardium.
Forecast
The prognosis of effusion pericarditis is largely determined by the reasons that caused its appearance and the treatment that took place. Most often it is favorable - over 70% of patients who have undergone it survive for 5 years. But when it comes to cardiac tamponade, the mortality rate in this case exceeds 50%.
In the most favorable course, the exudate resolves on its own and the patient’s condition returns to normal.
Have you or your loved ones already encountered exudative pericarditis? How and with what do you fight it? Tell us about it in the comments - give hope to other readers!