- Causes of tuberculosis of bones and joints
- How does infection occur?
- Provoking factors
- What's happening?
- Classification
- Symptoms and first signs
- Diagnostics
- Treatment of tuberculosis of bones and joints
Tuberculosis is a specific infectious disease that is characterized by a chronic progressive course with a gradual deterioration of a person’s condition. In the absence of adequate etiotropic treatment aimed at destroying the pathogen, it can lead to death. Pulmonary tuberculosis is the most common. In second place in frequency is bone damage.
Epidemiology
In the last decade, there has been an increase in osteoarticular tuberculosis by 30%. Today, this pathology accounts for 10% of all extrapulmonary forms of the disease. The disease is increasingly being reported in older patients. In 80% of cases, tuberculosis of bones and joints is complicated by limitations in joint mobility (contractures).
Diagnosis of the disease is difficult and in total lasts about 1 year. In 64% of patients, Mycobacterium tuberculosis (MBT) is resistant to anti-TB drugs, which significantly complicates the healing process.
Predisposing factors for the development of the disease:
- physical overload,
- frequent injuries of the musculoskeletal system,
- unsettled life,
- malnutrition,
- alcoholism.
Causes of pathology
- The development of tuberculosis is provoked by bacteria or, as they are also called, Koch bacilli. They affect the bones, which contain a spongy substance containing a network of blood vessels. The activity of pathogenic bacteria leads to non-healing abscesses and fistulas. The patient complains of impaired joint mobility. In the most severe cases, there is complete destruction of the bone and a decrease in its length.
- If Koch's sticks affect the spine, this leads to complete paralysis, deformation of the spine, its curvature and the appearance of a hump.
The Koch bacterium enters the body in different ways. The most common method is airborne.
When a sick person produces sputum, for example, when coughing, some of it settles on objects, surfaces or food.
They enter the body of a healthy person through unwashed hands or food, and quickly spread through the circulatory system throughout the body, ending up in organs and bones.
But not everyone develops tuberculosis when pathogenic bacteria enter the body. Its development is helped by many factors, the main one of which is immunity.
In a healthy person, the body's defenses cope with bacteria; they do not harm the body.
If the body is weakened or the patient has recently suffered from a serious illness, then mycobacteria begin to develop in any organ. The impetus for the development of the disease will not be living conditions or unsanitary conditions.
Among the causes of bone tuberculosis, doctors:
- Severe physical overload;
- Bone injuries;
- Hypothermia of the body;
- Frequent general diseases, relapses of old diseases;
- Difficult working conditions.
The causative agent of tuberculosis
The causative agent of tuberculosis was discovered in 1882 by Robert Koch, for which the researcher was awarded the Nobel Prize in 1905. Of the 30 species of mycobacteria, only 3 cause the development of disease in humans - human, bovine and avian. The pathogen is very stable in the external environment: it lives up to 10 years in manure, up to 19 days in the milk of a sick animal, up to 300 days in butter, up to 1 year in frozen meat. Mycobacteria cannot be frozen out. Maintain boiling for the first 15 minutes. They live up to 3 years in a dried state. Bacteria quickly develop resistance to anti-TB drugs.
The complex nature of bacterial metabolism ensures resistance and survival in the external environment. A powerful 3-layer shell protects against macrophages, which are the first to fight infections. Under conditions unfavorable for the microbe, they transform into the L-form and remain viable in this form for decades.
Rice. 1. Mycobacterium tuberculosis was discovered by Robert Koch in 1882.
Rice. 2. Pathogens of tuberculosis.
Rice. 3. The photo shows a colony of mycobacteria in an electron microscope.
How the disease develops
The disease occurs either during the first meeting of a person with Mycobacterium tuberculosis, or during the generalization of the infectious process with secondary tuberculosis. MBT penetrates through the blood and lymph into bone structures, settling in the red bone marrow. Specific granulomas form around them. As the disease develops, the granulomas merge, forming a conglomerate, in the center of which there is a zone of cheesy necrosis. Destruction of a bone or joint is accompanied by certain complaints. The larger the volume affected by the tuberculosis process, the brighter the clinical picture of the disease. The degree of organ destruction determines the development of complications.
Therapy based on antibacterial drugs
It is prescribed in the early stage of the disease in order to stop pathogens, prevent the development of inflammation and complications, and accelerate the attenuation of pathology. Streptomycin, Kanamycin, Viomycin are the most commonly used antibacterial agents.
To increase effectiveness, combine with anti-tuberculosis drugs:
- isonicotinic acid hydrazide and its analogs;
- para-aminosalicylic acid derivatives.
The course of treatment includes simultaneous administration of two or three drugs at the maximum dosage. The duration of therapy ranges from 12 to 18 months. It has been noted that the combined use of these drugs stops the tuberculosis process in 95% of cases.
In addition to specific treatment, the doctor may prescribe hormonal drugs (cortisone, hydrocortisone) to correct the general condition, reduce local inflammatory processes, and prevent ankylosis of the joints.
Spinal tuberculosis (tuberculous spondylitis)
Spinal tuberculosis is a disease that often results in the patient being unable to work and leading to disability. Starting with damage to the body of one vertebra, the process gradually spreads to neighboring vertebrae. Their destruction leads to deformation of the spinal column and a number of serious complications. Among all diseases of bones and joints of a tuberculous nature, damage to the spine accounts for 60%. More often the disease is registered in men. In 60% of cases, the disease affects the thoracic and in 30% - the lumbar spine. In 65% of patients who sought medical help for the first time, damage to 3 vertebrae was noted. Over the next years, the disease can affect up to 10 vertebrae.
How does spinal tuberculosis develop?
Prespondylytic phase
Spinal tuberculosis begins with damage to the body of one vertebra. Very rarely, the lesion is localized in the arch or process of the vertebra.
Spondylytic phase
Characterized by the spread of the disease to adjacent vertebrae. There are two ways the infection can spread.
- Intradiscal path, when the infection penetrates into adjacent vertebrae through the intervertebral disc, which is first partially destroyed and then completely destroyed.
- The extra-discal path, when the cortical (outer) layer of the vertebrae is destroyed and the tuberculosis process spreads to nearby soft tissues, where specific granulations are formed, which are the source of damage to other vertebrae.
Rice. 4. Spread of infection to adjacent vertebrae through a destroyed intervertebral disc (macro specimen).
Rice. 5. Spread of infection to adjacent vertebrae through a destroyed intervertebral disc (macro specimen). The curdled masses compress the spinal cord.
Rice. 6. The photo shows a leaky abscess with a dense fibrous capsule and thick contents (macropreparation).
Over time, the destroyed vertebrae sag with the formation of spinal curvature like kyphosis (hunchback). Cavities often form - abscesses (previously called leaks), which are surrounded on the outside by dense connective tissue that forms its outer wall. The inner wall of the abscess is tissue consisting of tuberculous granulations. The abscess is filled with destroyed (necrotic) masses and pus. Under the influence of gravity, the purulent sac moves down along the connective and muscle layers. The abscess gradually increases in size and changes its original location. Often, the connection between the abscess and the primary focus is lost, but, despite this, it continues to function. When the skin is destroyed, the inflammatory process breaks out, forming fistulas.
If the wall of a hollow organ (uterus, rectum, bladder, pleural cavity) is destroyed, internal fistulas are formed. If the process spreads along the vertebral bodies from behind, then the destroyed bone structures and granulation tissues compress the spinal cord. The fibers of the spinal cord become inflamed. Spinal disorders develop. Tissue swelling caused by compression of blood vessels aggravates the situation. More often, such complications occur when tuberculosis damages the thoracic spine, which is associated with the anatomical features of the structure of the body.
Postspondylytic phase
Degenerative-dystrophic changes in the spine, as the outcome of a specific process, lead to the development of osteochondrosis and spondylosis with pronounced muscle atrophy. Kyphosis or scoliosis is pronounced in this phase. Severe deformation of the chest.
Rice. 7. The photo shows spinal tuberculosis. We see a formed hump (kyphosis). The spinal cord is deformed and compressed. MRI picture.
Rice. 8. The photo shows spinal tuberculosis (severe curvature).
Rice. 9. The photo shows a pronounced curvature of the thoracic spine.
Rice. 10. The red circle on the x-ray shows a typical injury to the lumbar vertebra.
Rice. 11. Typical lumbar vertebral injury.
Symptoms of spinal tuberculosis and clinical picture of the disease
Symptoms of spinal tuberculosis and the clinical picture of the disease depend on the location of the process and the degree of organ destruction.
Symptoms of spinal tuberculosis and clinical picture in the prespondylytic phase
This phase is characterized by the fact that the process is limited to the body of one vertebra and does not go beyond its limits. Intoxication of the body manifests itself weakly, somewhat more clearly in children. Phenomena such as a feeling of heaviness and minor pain in the spine disappear after rest. During this phase, patients practically do not seek medical help.
Symptoms of spinal tuberculosis and clinical picture in the spondylitis phase
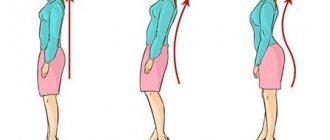
During this phase, the process spreads beyond the vertebral body affected by tuberculosis. Symptoms of intoxication appear clearly during this phase. Pain in the spine increases significantly and has different colors and irradiations. The mobility of the spine is limited. Muscle rigidity (tension) is noted, which occurs as a response to pain. The patient's gait changes. The usual body position (posture) changes. There is atrophy of the back muscles.
Symptoms of spinal tuberculosis and clinical picture in the post-spondylytic phase
Symptoms of the disease in this phase are caused by the development of degenerative-dystrophic changes, with the development of osteochondrosis and spondylosis. Muscle atrophy is pronounced. Kyphosis or scoliosis is obvious. The chest is sharply deformed. The spine is unstable. The patient experiences severe pain localized in the area of spinal curvature. Exacerbations of the disease are severe.
Orthopedic correction methods
This treatment is based on unloading and immobilization. For tuberculosis of the spine and hip joint, the patient is placed in a plaster bed (semi-corset). During the activation phase of the process, the patient remains in a semi-corset.
If there is deformation or incongruence of the articular surfaces during the attenuation phase, it is necessary to wear a corset or orthosis.
Important! An orthosis is a medical device designed to fix a joint (knee, ankle, wrist) and prevent further damage to the ligamentous apparatus.
Tuberculosis of bones
Rib lesions
The disease is rare. Children over 10 years of age become ill more often. The tuberculous process spreads to the rib from the lymph nodes or pleura affected by the pathological process. First, the rib thickens, then collapses, abscesses and fistulas form. Fistulas quickly break out. The course of the disease is persistent.
Rice. 12. The picture shows a rib lesion. The rib is thickened.
Rice. 13. The image shows a marginal rib defect with a contrasting mass. Child 9 years old.
Damage to the bones of the skull and face
The disease is rare. Young children get sick more often. Tuberculosis affects the frontal and parietal bones, less commonly the temporal bone. The dura mater prevents further spread of infection.
Rice. 14. Child 1 year 3 months. The x-ray shows damage to the parietal bone of the skull.
Rice. 15. On the x-ray we see damage to the pelvic bones.
Joint tuberculosis
How does joint tuberculosis develop?
Tuberculosis of the joints begins with damage to the epiphyses and metaphyses of long tubular bones, that is, from the periarticular zones, where there is a large accumulation of spongy substance. In these areas, the vessels have close contact with bone tissue. Granulomas form around the office, which eventually merge into a single conglomerate with a cheesy disintegration in the center. Granulation tissues gradually grow, reaching the synovial membrane of the joint and destroying it. For reference: the metaphysis is a section of a long tubular bone that is intimately connected to the diaphyseal plate, due to which bone growth occurs. The metaphyses are well supplied with blood, which is why they are more vulnerable to infection that spreads through the bloodstream.
Rice. 16. The structure of a long tubular bone.
Symptoms of joint tuberculosis and clinical picture of the disease
Symptoms of joint tuberculosis and clinical picture in the prearthritic phase
At the beginning of the disease, the patient experiences pain that occurs when pressure is applied to the area affected by tuberculosis. Hyperextension of the joint due to pain is limited. Passive joint extension is stepwise. Symptoms of intoxication are mild.
Symptoms of joint tuberculosis and clinical picture in the arthritic phase
During the arthritic phase of the disease, a breakthrough of specific inflammation into the joint cavity is noted, which is accompanied by increased body temperature. The affected area has an elevated temperature. The skin fold is thickened when grasped. The soft tissue around the affected joint swells. The contours of the joint gradually begin to smooth out. The joint becomes inactive, sometimes complete blockage occurs. When the joint is immobilized, the symptoms of inflammation decrease after a week. Symptoms of intoxication during the height of the disease are more pronounced. The volume of the affected joint increases, the articular ends are displaced, the installation is incorrect (flawed), which is why dislocations and subluxations of the joint often occur. During the period of remission of the disease, all symptoms gradually subside, but functional impairment remains.
Symptoms of joint tuberculosis and clinical picture in the post-arthritic phase
During this phase of the disease, the patient's condition is assessed as satisfactory. The limb is shortened. The diseased joint is deformed. Soft tissues are atrophied. Functional disability of the limb and pathological changes cause pain when walking and at rest.
Rice. 17. The photo shows tuberculosis of the left hip joint. The head of the joint is completely destroyed. 1 - dead areas of bone tissue (sequestra), 2 - a leaky abscess is visible in the soft tissues of the thigh.
Rice. 18. The photo shows tuberculosis of the hip joints. The head and neck of the femur on the right are completely destroyed.
Rice. 19. The photo shows tuberculosis of the left hip joint. The greater trochanter of the femur is completely destroyed.
Rice. 20. The photo shows tuberculosis of the knee joint. A large area of necrosis (sequestrum) is visible under the cartilage. The condyles of the femur and tibia are destroyed.
Rice. 21. The photo shows tuberculosis of the knee joints.
Rice. 22. The photo shows tuberculosis of the wrist joint in a 72-year-old woman. The duration of the disease is 5 years. A bone cavity with a characteristic sequestrum is visible.
Rice. 23. The photo shows a tuberculous lesion of the calcaneus.
Expert opinion
Confirming the need for early detection and timely treatment are prognostic theses formulated by the Federal State Budgetary Institution “St. Petersburg Research Institute of Phthisiopulmonology of the Ministry of Health of the Russian Federation” and the Federal State Budgetary Institution “Children’s Sanatorium for Patients with Extrapulmonary Forms of Tuberculosis.”
- In 99% of cases, with complex treatment, a complete cure is observed.
- The transition to the chronic phase (including the formation of fistulas) is caused by non-radical methods.
- Clinically important functional disorders of the skeletal system in the period from 4 to 12 years after surgery occur in 3-30% of cases.
Rare forms of tuberculosis of bones and joints
Tuberculosis of the diaphysis of long bones (Spina ventosa tuberculosa)
Tuberculosis of the diaphyses of long bones is more common in childhood. The short tubular bones of the hands and feet are affected. Less commonly, long tubular bones. MBTs settle in the bone diaphysis (the part of the bone between the two epiphyses), where granulomas form. Over time, granulomas merge into a single conglomerate, which leads to thickening of the periosteum. The bone takes on the appearance of a spindle. This disease is called spina ventosa, which means swollen spine. Gradually, the affected tissues are destroyed. At the site of destruction, a purulent cavity is formed, filled with small sequestration. If the process extends beyond the bone, leaks are formed. When the process goes beyond the bone structures into soft tissues, fistulas are formed. At this time, pathological fractures and dislocations are recorded.
Rice. 24. Damage to the phalanx of the third finger (spina ventosa tuberculosa). The x-ray shows multiple areas of destruction, sequestration and compacted soft tissue in the affected area.
Rice. 25. The picture shows Spina ventosa tuberculosa of the phalanges and metacarpal bones of the child.
Rice. 26. Spina ventosa tuberculosa in a 2-year-old child. Damage to the tibia. A and B – the height of the disease; C and D - after successful treatment 9 months later.
Tuberculosis-allergic joint damage (Ponce's disease)
The disease was first described in 1896 and named after the author who first described it. Damage to the synovial membrane of the joint in Ponce's disease is a consequence of paraspecific allergic reactions, as a pathological response of the body to an infectious process located in another organ (usually the spine). Cases of damage to the knee joints have been described.
As a result of the disease, the joint space gradually narrows, and osteoporosis is noted in the bone. The course of the disease is persistent and undulating and does not respond to antirheumatic therapy. A characteristic feature of the disease is the absence of any changes in the bones. Sometimes abscesses and fistulas appear. With a long course, amyloidosis of internal organs develops. Over time, joint deformation occurs. In 20% of cases, the deformity is severe, up to ankylosis (complete immobility).
Rice. 27. The photo shows tuberculous polyarthritis of Ponce in a 15-year-old girl.
Multiple cystic or cavernous tuberculous osteitis of Yuengling
The disease is one of the types of bone tuberculosis, which manifests itself during puberty. Young men get sick more often. Some authors believe that Yuengling's osteitis is caused by weakened tuberculosis infection. The disease affects the phalanges, metatarsals and metacarpal bones of the limbs. Cases have been described in which the bones of the cranial vault, pelvic bones and vertebral bodies are affected. Very rarely the disease is widespread. With Yuengling's osteitis, cheesy necrosis never occurs in tuberculous granulomas, sequesters never form in the cavities, and osteoporosis never occurs in the bones. The course of the disease is benign. Its duration is 15 - 20 years. There is minor pain in the fingers. Yuengling described three forms of the disease:
- In the first case, the cysts in the bones are multiple and small in size. Almost all phalanges are affected.
- In the second case, the centers of destruction are rough. Their shape is cellular. Cysts almost completely replace the normal bone pattern. The cortex (the outer layer of the compact substance) becomes thinner and never becomes sclerotic. Often the entire heel bone is affected.
- In the third case, the disease proceeds with severe destruction (osteolysis). The phalanges are severely deformed. Pathological fractures often occur. The disease greatly cripples a person.
Rice. 28. Yuengling's tuberculous osteitis.
Still's or Still-Shofar's disease
The causes of Still's disease have not yet been fully identified. Many scientists believe that this is not an independent disease. A number of researchers believe that there are many causes of the disease. Some of them dispute the tuberculosis nature of the disease. Still's disease is more common in girls 2-3 years old. Characterized by an acute onset. Body temperature rises significantly. A quickly passing rash appears on the skin.
The process quickly becomes chronic and progresses rapidly. The interphalangeal joints of the three middle fingers of the hands are symmetrically affected. The soft tissues over the affected area swell. No changes are noted on radiographs. Over time, the cartilage surfaces of the joints are destroyed. The joint spaces narrow. The joints become deformed. Stiffness, flexion contracture and ankylosis develop, crippling the patient. Osteoporosis develops in the epiphyses of the bones, which gradually reaches a severe degree. With the negative development of the disease, the hip joints begin to be affected. Cases of damage to the cervical vertebrae have been described. The bone structure of the affected areas is coarse, almost transparent. The periosteum of the phalanges thickens and resembles spina ventosa.
Rice. 29. An x-ray shows a typical picture of Still’s disease in a 10-year-old boy.
Rice. 30. Schematic representation of Still's disease. On the left is the healthy hand. On the right is the affected one.
Complications of tuberculosis of bones, joints and spine
Tuberculosis of bones and joints always ends tragically. Degenerative-dystrophic changes that develop as a result of the disease are the cause of osteochondrosis, spondylosis and arthrosis.
Types of complications of tuberculosis of bones, joints and spine:
- Joint deformity.
- Spinal deformities – lordosis, kyphosis, kyphoscoleosis.
- External and internal fistulas.
- Swelling abscesses.
- Protein metabolism disorder (amyloidosis of internal organs).
- Neurological disorders up to dysfunction of the pelvic organs.
Rice. 31. Severe curvature of the thoracic spine as a result of tuberculosis.
Rice. 32. The photo shows tuberculosis of the left knee joint. Atrophy of the thigh muscles. The lower leg is bent and deviated from the outside.
Rice. 33. The photo shows tuberculosis of the left knee joint in a child. The lower leg is bent due to muscle contracture and is swollen. Significant shortening of the limb.
Rice. 34. On the radiograph, there are edema abscesses (indicated by arrows) on both sides of the spine affected by tuberculosis.
Omartritis
Inflammation of the shoulder joint occurs quite rarely, but the disease is diagnosed in men more often than in women.
Symptoms
- Intoxication,
- Joint pain,
- Joint dysfunctions
- Amyotrophy.
Diagnostics
A clinical examination of the patient is carried out.
A radiograph is used.
Treatment
Fixation of the limb, use of physiotherapeutic treatment. Puncture is also used and surgery is possible.
In case of a purulent form of the inflammatory process and swelling, a wide opening of the joint is applicable.
Diagnosis of tuberculosis of bones and joints
Tuberculosis of bones and joints is difficult to diagnose, especially in the early stages of the disease. Diagnosis of tuberculosis of bones and joints consists of a combination of studies:
- clinical,
- X-ray,
- laboratory
- Carefully collected anamnesis.
- General clinical studies.
- X-ray examination, which confirms and clarifies the diagnosis.
- Tuberculin diagnostics.
- Microbiological examination of any tissue material obtained during biopsy or surgical interventions.
- Histological and cytological examination of any tissue material.
- Arthrography and arthroscopy.
- Thermography.
- Rheography.
- Radionuclide research.
- Trial treatment.
Rice. 35. X-rays of bones and joints are an important component of diagnosis.
Fig.36. Arthroscopy of the hip joint.
Rice. 37. Conducting tuberculin diagnostics.
Rice. 38. To detect the causative agent of tuberculosis in pathological material, bacterioscopic and bacteriological methods are mainly used.
Rice. 39. Mycobacterium tuberculosis. Luminescence microscopy.
Rice. 40. Sowing on Lowenstein-Jensen medium M. Bovis.
Changes in laboratory tests
Another method for diagnosing bone tuberculosis is laboratory tests. These studies are the same for all forms of tuberculosis; they are used if other diagnostic methods cannot give an unambiguous answer about the presence of the disease.
Bacterioscopic examination rarely reveals the presence of Koch bacteria in the material being examined. To identify them, cytological examination is often used.
The material is collected by puncturing the bone marrow, lymph nodes, joint fluid, bone and soft tissues. The disadvantage of this method will be its unreliability if normal sampling of material is impossible due to limited space.
In case of bone tuberculosis, its complications, for example, abscesses or fistulas, a detailed blood test shows an increased level of ESR, neutrophilic leukocytosis.
Treatment of tuberculosis of bones and joints
Treatment of tuberculosis of bones and joints is a long process and requires great patience and self-discipline from the patient. The main directions of the treatment process are:
- elimination of the infectious agent,
- preventing destruction of bone structures,
- increasing the patient's immune status,
- restorative treatment.
Anti-tuberculosis chemotherapy
In the first stages, the selection of chemotherapy regimens is carried out in a hospital setting. In the arsenal of doctors there are more than 11 groups of drugs (first and second line) for the treatment of tuberculosis and a whole arsenal of surgical treatments.
First line drugs
First-line drugs are the most effective in treating tuberculosis. They are low toxic. Rarely cause side effects. This group includes:
- rifampicin,
- isoniazd, metazide, ftivazide, phenazide,
- aminoglycosides (kanamycin, amikacin, streptomycin),
- ethambutol,
- pyrazinamide
Second line drugs
If first-line drugs are poorly tolerated or if resistance to them develops, second-line drugs are prescribed. This group of drugs is less effective against the pathogen and is highly toxic. This group includes:
- fluoroquinolones,
- PASK,
- cycloserine,
- prothionamide,
- ethionamide,
- capriomycin, etc.
When prescribing anti-tuberculosis drugs, the following are taken into account:
- patient's weight,
- patient's age,
- concomitant pathology,
- side effect of the drug,
- process phase,
- resistance of mycobacteria to this drug, etc.
The treatment regimen for the disease includes at least 3 drugs. Rifampin and isoniazd are the “core” anti-tuberculosis drugs. Treatment of the disease is significantly more difficult in the case of late detection of the disease, when the affected organ is significantly destroyed, serious complications have appeared, and the patient himself is exhausted and anemic. Proper management of the patient by physicians and the proper attitude of the patient towards his treatment can achieve significant success in the treatment of osteoarticular tuberculosis.
Surgery
Direction of surgical treatment:
- removal of the damaged area of bone,
- creating favorable conditions for treatment (therapeutic and auxiliary techniques),
- correction of the consequences of previous tuberculosis.
Orthopedic treatment
Orthopedic treatment is aimed at immobilizing the limb during the active period of the disease.
Abscessectomy.
Physiotherapy.
Physiotherapy.
Sanatorium treatment.
Rice. 41. Traction on pillows with a cuff for damage to the knee joint.
Rice. 42. Traction in two planes in a hammock box.
Rice. 43. Plaster bed for spinal lesions.
Rice. 44. Twisting to correct contracture of the knee joint using two pairs of squares embedded in a plaster cast.
Rice. 45. Surgical treatment of spinal tuberculosis. Excision of affected areas of the vertebrae with subsequent correction of spinal column deformity.
Therapeutic gymnastics: recommendations
Therapeutic gymnastics is an important and mandatory component in complex therapy for the treatment of bone tuberculosis. If the disease is in the active phase, exercises are carried out to improve general well-being, prevent secondary deformation, and also prevent muscle atrophy. The part of the body that is fixed by the plaster bandage should not move.
When the disease activity decreases, you can perform exercises that involve the affected organ. The back muscles located near the vertebrae, gluteal muscles, and lower limbs are massaged. Only those joints that are directly affected are not massaged. You can actively work with them only with arthritis, osteitis, or with superficial destruction. But this is possible only in the absence of abscesses and caseous-necrotic foci.
When the course of the disease has subsided and stabilized, the patient begins to perform exercises while standing. The main task here is to develop correct posture and learn how to walk correctly. In addition to physical therapy, patients will benefit from salt-pine baths and some traditional medicine methods. With their help, motor activity and range of motion will quickly be restored.
© 2021, Golub Oleg Vasilievich. All rights reserved.
Prevention of tuberculosis of bones and joints
- Tuberculosis is an infectious contagious disease. Work on its prevention is aimed at the source of infection, the routes of its transmission and the susceptible population.
- The second direction in the prevention of the disease is a set of measures for the timely identification of patients suffering from osteoarticular tuberculosis and the prevention of their disability.
General medical doctors - surgeons, orthopedists, therapists, neurologists - are prescribed to detect tuberculosis of bones and joints. Knowledge of risk groups for tuberculosis, early symptoms of the disease and diagnostic methods helps to detect the disease in a timely manner.
At the initial stages of development of osteoarticular tuberculosis, the disease often occurs under the guise of chronic arthritis and synovitis, deforming arthrosis, osteomyelitis, and osteochondrosis.
Spinal tuberculosis in the initial period manifests itself in the form of intercostal neuralgia and myositis, the origin of which is difficult to determine. Intoxication syndrome has varying degrees of severity. There is local pain in the area of the affected vertebra. The patient's posture changes, stiffness of the back muscles appears, and movement in the spine is limited due to pain. The appearance of leaks manifests itself in the form of retropharyngeal, intra-abdominal and retroperitoneal abscesses.
Joint tuberculosis in the earliest stages is characterized by pain and limited mobility. The contours of the joint gradually smooth out, the temperature above the affected area rises. Breakthrough of the lesion into the articular cavity imitates an acute process. At the slightest suspicion of joint tuberculosis, an X-ray examination, general clinical tests and microbiological examination of any tissue material obtained during biopsy or surgical interventions are carried out in a clinic or hospital.
Transmission routes
Is bone tuberculosis contagious? Unfortunately, Koch's bacillus easily spreads from one person to another. This is facilitated by two factors - the long life span of the bacillus and high resistance to adverse factors.
How is bone tuberculosis transmitted? Infection occurs in one of 6 ways:
- Airborne - through coughing, is considered the most common route of transmission, with a large radius of damage;
- Airborne dust - when the sputum particles dry out, the bacilli go into a dormant state, but at the same time retain their destructive ability;
- Food - through the consumption of contaminated products (usually food of animal origin);
- Intrauterine - during labor (provided that the mother had an active form of tuberculosis at the time of pregnancy);
- Secondary or autoinfection - through the blood or lymph after activation of the primary source of infection;
- Contact - through clothing, household items, blood, personal belongings, as well as during kissing, sexual intercourse, surgical interventions and organ transplantation.