The accumulation of fluid in the lung tissue, or pulmonary edema, is a serious condition that requires medical intervention and long-term treatment. The rate at which the disease develops depends on the causes and the body’s immune system.
Sometimes it can take several weeks before the first symptoms appear. Acute edema develops in just a few hours.
The causes of the disease can be not only pulmonary diseases, but also pathologies of other organs. Before prescribing treatment, your doctor will need to determine the causes and symptoms of fluid in the lungs.
- How to remove fluid from the lungs?
- Drug treatment
- Alternative medicine
Causes of fluid in the lung
Pulmonary edema can occur not only with cancer. All causes of this condition are divided into two large groups:
- Cardiogenic - associated with disruption of the heart.
- Non-cardiogenic - associated with other pathological processes in the body, for example, with an increase in the permeability of pulmonary capillaries.
Read more about possible causes of edema:
- Oncological diseases of internal organs
- Various diseases causing sepsis, pneumonia, circulatory congestion
- Overdose of a number of drugs, as well as narcotic drugs
- Effects of radiation on lung tissue
- Heart disease in the stage of decompensation
- Thromboembolism of blood vessels and capillaries of the lungs
In cancer, there are both cardiogenic and non-cardiogenic causes.
Cardiogenic form
Cardiogenic OB occurs as a manifestation of left ventricular heart failure. The following diseases can lead to the development of pathology:
- myocardial infarction, post-infarction conditions;
- acquired heart defects (both aortic and mitral);
- hypertensive crisis;
- disturbances of heart rhythm and conduction (arrhythmias, blockades).
The mechanism of development of the cardiogenic form of edema is associated with an increase in pressure in the pulmonary capillaries. This occurs due to increased diastolic pressure in the left ventricle.
The left ventricle cannot contract enough to push all the blood out of the cavity into the aorta. This leads to an increase in pressure first in the left ventricle and then in the left atrium. Since the pulmonary veins flow into the left atrium, over time the pressure also increases in the pulmonary circulation. The fluid sweats first into the interstitial tissue and then into the alveoli.
By the same principle, the lungs swell due to hypervolemia (increased blood volume).
Hypervolemia can develop as a complication of infusion therapy.
Folk remedies
There are many “folk” methods for treating pulmonary edema. Among the recipes that should help relieve swelling, the most common are formulations based on the following plants:
- Cherry
- Linen
- Liquorice root
- Juniper fruits
- Lovage root
- Steelwort root
- St. John's wort
- Dog-rose fruit
- nettle leaves
- Plantain leaves
- bearberry leaf
These and some other plants in various proportions are offered to be brewed, steamed or infused. Such a solution should help in the treatment of pathology.
Some substances contained in these plants may indeed help relieve symptoms, but are not very effective as a primary treatment.
Consequences for life
The prognosis depends on several factors: timeliness of care, concomitant pathology and severity of the condition. The danger of the disease is the development of acute respiratory failure. Because of this, not only the respiratory system suffers, but also all organs that do not receive enough oxygen.
In many cases the prognosis is poor. Old age is one of the risk factors that aggravates the course of the disease.
With OL, patients die from asphyxia. With early treatment (at the stage of interstitial edema), complete recovery is possible. The prognosis largely depends on the cause; with cardiogenic shock or sepsis, the mortality rate is several times higher.
Fluid in the lungs with cancer
In cancer patients, pulmonary edema often occurs as a complication of chemotherapy.
Some anticancer drugs (anthracyclines, cyclophosphamide) and high-dose radiation therapy cause damage to the heart muscle - cardiomyopathy . In this case, the muscles of the ventricles of the heart weaken and cannot adequately cope with their functions, heart failure develops, which leads to pulmonary edema. Symptoms often increase gradually.
Acute non-cardiogenic pulmonary edema can develop during treatment with interleukin-2, mitomycin, and vinblastine. Patients who receive chemotherapy have a weakened immune system and are at increased risk of infections, which can lead to acute respiratory distress syndrome , a condition in which the lungs become inflamed and fill with fluid. Tretonin treatment may cause systemic capillary leak syndrome , a rare condition in which fluid accumulates in the lungs and other organs.
Patients who have had radiation therapy to the chest area have an increased risk of damage to the coronary arteries and heart valves. In this case, the functioning of the heart is disrupted and heart failure develops.
Cardiogenic pulmonary edema can also be caused by the tumor itself during the development of heart failure as a result of the following conditions:
- Metastasis of the lymph nodes in the chest and compression of the heart.
- Metastases of tumors in the cardiac membrane - pericardium .
- Superior vena cava syndrome, when the return of blood to the heart from the upper part of the body is disrupted as a result of blockage of the lumen of the vein by a tumor and blood clots.
Sometimes cancer has nothing to do with it: it is simply combined with severe cardiovascular disease, which leads to heart failure and fluid accumulation in the lungs.
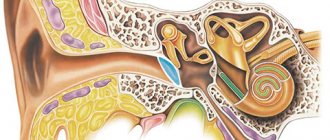
Diagnostics
At the initial appointment, the doctor conducts an examination (when breathing, the right or left side of the chest may be delayed), taps, and listens to the patient with a phonendoscope.
The purpose of diagnostic studies is to establish not only the fact and severity of pulmonary edema and/or hydrothorax, but also its cause.
A biochemical blood test, an analysis of the content of gases in the blood, and coagulation help to do this.
Using an X-ray, you can clearly see the accumulation of fluid, estimate its volume, detect a tumor, and damage to the lymph nodes.
More detailed, additional information is provided by computer and magnetic resonance imaging (CT, MRI), ultrasound of the chest.
To confirm or exclude cancer, a puncture or biopsy is performed, followed by a morphological examination (cytological, histological). In the first case, fluid is taken from the pleural cavity, in the second, a fragment of pleural tissue is taken.
Make an appointment with a doctor now
What are the symptoms of pulmonary edema?
Fluid in the lungs can build up quickly or gradually. Depending on this, acute and chronic pulmonary edema are distinguished. Their symptoms vary:
| Acute pulmonary edema | Chronic pulmonary edema |
|
|
Symptoms
The picture of symptoms depends on the amount of fluid that has accumulated and on what disease caused the process.
Oxygen starvation
Lack of oxygen causes blue skin, as well as other consequences. A state of anxiety appears in patients.
Chest pain from below
Manifestations of pain in the lower chest intensify when coughing. If the disease bothers a small child, then after an attack he cries for a long time (with a hoarse tinge).
Intermittent cough
As the pathological process worsens, a peculiar intermittent cough occurs. During it, mucus is released. In parallel with the cough, dizziness, increased breathing, fainting, excitement of the nervous system, and temperature instability occur.
Attacks of shortness of breath that become more frequent over time
When the disease progresses slowly, difficulty breathing can appear unpredictably. Along with an attack of shortness of breath, weakness occurs.
The peculiarity is that the symptom can manifest itself in a calm state. If the swelling is large and affects two lungs, then the fluid inside the organ in question can cause suffocation.
During the accumulation of fluid, attacks of shortness of breath most often appear in the morning. They are also provoked by stress, heavy physical activity or regular hypothermia. If a person suffers from heart failure, then the state of suffocation may appear at night, for example, during a nightmare.
How dangerous is fluid in the lungs and what complications are possible?
Acute and advanced chronic pulmonary edema is life-threatening. The lungs cease to cope with their function, oxygen starvation increases in the tissues.
The lack of adequate treatment can result in a number of complications that can threaten the vital systems of the body:
- The development of fulminant edema is a dangerous condition that can cause death within a few minutes
- Airway obstruction due to the formation of large amounts of foam
- Difficulty and depressed breathing
- Tachyarrhythmia and asystole - extreme increase in heart rate
- Destabilization of blood pressure
If prompt treatment measures are taken, many of these complications are treatable.
Non-cardiogenic form
Toxic OA is more common in older people than in other age categories. Non-cardiogenic edema is caused by damage to the blood-air barrier. As a result, there is a violation of the permeability of fluid into the interstitial space and alveoli. This is possible under the following conditions:
- respiratory tract burn;
- pneumonia;
- chest injury;
- septic conditions;
- pancreatitis;
- renal failure;
- acute cerebrovascular accident;
- poisoning with drugs (for example, salicylates);
- poisoning with toxic substances.
The mechanism of development of pulmonary edema in these conditions is associated with the action of toxins (poisons, bacterial exotoxins, metabolites in renal failure, etc.) on the endothelium of the pulmonary capillaries.
How to treat a patient who has fluid in the lungs?
The first aid measure for acute pulmonary edema is oxygen supply through a mask. This helps reduce symptoms. Sometimes artificial ventilation is indicated. In order to remove excess fluid from the body, furosemide (Lasix) is prescribed. Morphine and other drugs help reduce shortness of breath and anxiety. Vasodilators (for example, sodium nitroprusside) dilate blood vessels and reduce the load on the heart.
If a patient with pulmonary edema has high blood pressure, they are prescribed drugs that help bring it down; if it is low, they try to increase it.
Treat a condition that causes fluid to accumulate in the lungs. If the cause is side effects of chemotherapy, the doctor may stop the drugs and replace them with others.
Treatment
Removal of fluid from the lungs occurs only after a qualitative examination. At the very beginning, the patient is hospitalized. In the case when the volume of exudate is small, it can be removed with the help of medications.
Among the drugs that are often used in such situations are:
- analgesics;
- antibacterial drugs;
- drugs to speed up urine excretion;
- anti-inflammatory agents .
If drug therapy is ineffective, a catheter is used. Doctors may prescribe oxygen inhalation during pulmonary failure.
If the accumulation of fluid was caused by some kind of disease, then the first thing to do is to eliminate the source of the pathology so that serious complications do not appear.
Prevention
Prevention of fluid accumulation in the pleura during oncology consists of measures aimed at eliminating the disease that can provoke it. Fluid in the lungs during cancer can accumulate due to diagnoses such as pulmonary tuberculosis, other pulmonary diseases of non-tuberculous origin (pneumonia), and rheumatism. Other measures to prevent it are related to general recommendations for improving the health of the body: a balanced diet, regular exercise, hardening, maintaining a sleep schedule and giving up bad habits that can reduce immunity.
Book a consultation 24 hours a day
+7+7+78
Diet and exercise
The effectiveness of treatment depends, among other things, on the patient’s diet and physical activity. In order not only not to aggravate the problems, but also to improve the condition, nutritionists advise adhering to a special diet:
- first of all, you need to maintain a drinking regime - you should drink at least one and a half liters of water a day;
- Before going to bed, you should limit yourself to dense foods - it is better to eat a light snack;
- It is better to eat every 3-4 hours, avoiding snacks;
- The patient's diet should be as varied as possible - it should include meat, fish, poultry, vegetables, fruits and whole grains.
Not only a proper diet, but also moderate physical activity will help improve your immunity and relieve an attack of suffocation. Doctors advise doing exercises every day, which includes the following exercises:
- Hands should be placed along the body. They should be raised as you inhale, and lowered as you exhale.
- This exercise is similar to the previous one. Only when you inhale, you need to raise your arms to the side, and when you exhale, lower them as well.
- For the next exercise, you need to lie on your back, alternately bend your left and right legs at the knee joint.
- Lying on your back, you need to rest your elbows on the floor and lift your chest for a one-two count.
Thoracentesis
When and how is fluid pumped out of the lungs? Usually transudate, which is caused by a non-infectious nature, is removed. If the pathology is associated with inflammation and there is an admixture of pus in it, then this is exudate.
In such cases, the inflammation should be treated before the procedure. If liquid remains after this, it is removed. It should be borne in mind that pumping occurs from the pleural cavity; it is impossible to do this by suction. In these cases (pulmonary edema, for example), treatment is medicinal.
What is pumping fluid from the lungs called? Thoracentesis or thoracentesis. During these procedures, fluid is mechanically removed. Pain relief is performed with local anesthesia. No special preparation of the patient is required. Usually, the doctor tries to stabilize the state of the cardiovascular and respiratory systems with the help of symptomatic therapy before centesis. The patient is in a sitting position, slightly leaning forward, placing his hands on a special table or placing them behind his head.
How is the procedure for pumping fluid out of the lungs? First, using ultrasound or x-ray, the location of the accumulation of exudate is determined, then a local anesthetic is administered and an injection of novocaine is given.
The skin is wiped with alcohol, and the doctor carefully pierces the pleural cavity in the area under the scapula (in the middle between the mid- and posterior axillary lines) strictly along the upper edge of the rib between the 6th and 7th intercostal spaces with a thin injection needle. In this way, tissue infiltration is carried out with novocaine or lidocaine. Actions must be extremely careful, because there is a possibility of damaging the neurovascular bundle.
The depth must also be precise, so periodically the syringe plunger is pulled back to check. If the needle is inserted too deeply, the lung parenchyma may be damaged. The needle is inserted until a sensation of failure is felt - at this point the depth of penetration is measured. The upper lining of the lung (pleura) is denser than its contents.
Next, the anesthesia needle is removed, and a thick thoracentesis needle is inserted (to the measured depth). Through an adapter, the needle is connected to the electric suction pipe. Part of the effusion goes to the laboratory for analysis, the adapter is switched to suction and the effusion is evacuated. A device for pumping fluid from the lungs is an electric suction device or a drainage-suction device. In the absence of an electric suction, a Janet syringe is used.
The fluid is pumped out (aspiration of fluid from the pleura), catheters are inserted, through which exudate is released for some time. Pumping out fluid from the lungs does not take much time - about 15 minutes. After this, the catheters are removed and the puncture site is again lubricated with alcohol. A sterile dressing is applied. Sometimes catheters are left in place if necessary. A control x-ray is performed.
The procedure for pumping out fluid must be performed exclusively under sterile conditions. Therefore, pumping fluid from the lungs at home is not carried out. Depending on the purpose, aspiration can be therapeutic or diagnostic.
You can pump out no more than 1 liter of liquid at a time. If the volume is exceeded, complications arise and even death is possible. With a gradual decrease in the fluid level during the process of pumping it out, the patient becomes clearly relieved.
After pumping out fluid from the lungs, it can collect again, since the main cause of the disease itself is not eliminated during the procedure, and there are no guarantees for complete primary removal. For etiotropic treatment, other methods are used. Repeated thoracentesis is very difficult for patients to tolerate, because there are already adhesions that complicate the operation.
Weakening of the immune system always contributes to the re-accumulation of fluid. Patients over 60 years of age are at risk. Normalizing fluid levels in the lungs often requires treatment of other organs, judging by the list of diseases. Artificial removal of exudate from the lungs by puncturing them is another name for pumping out fluid from the lungs. The most radical method is bypass surgery. When a shunt is installed, it transfers the accumulated fluid from the pleural cavity to the abdominal cavity.
In case of non-surgical pathology, proper treatment of the underlying disease allows the amount of fluid to normalize on its own - this option is not excluded. But this does not apply to severe pathologies. Thus, the consequences of pumping fluid from the lungs are a short-term improvement in the patient’s well-being. To influence the cause of the pathology, pleurodesis is used.
Localization
You will be interested: Vishnevsky Institute in Moscow: services, doctors, address, patient reviews
This pathological process can occur in several forms, the distinguishing feature being its localization:
- right-sided;
- left-sided hydrothorax of the lung;
- double-sided
The most common occurrence is bilateral hydrothorax. This phenomenon can be explained by the following fact. The presence of an underlying disease causes the accumulation of pleural fluid first in one lung (right or left). The absence of pronounced symptoms most often means the absence of correct treatment, which means that over time a similar process develops in the second lung.