According to the World Health Organization, many patients die from a heart attack in the prehospital stage. Observations show that men die more often than women, and the cause of death is usually sudden death. The frequency of such sad outcomes is not related to the month of the year, but depends on other factors: time of day (usually in the early night or morning hours), day of the week (usually on weekends).
According to some statistics, approximately half of the men and 1/3 of the women who died due to myocardial infarction did not know that they had some kind of pathology of the heart and blood vessels. And the main factor predisposing to the development of this acute condition and subsequent death is arterial hypertension.
Cardiologists say that the patient’s life depends on the quality and timeliness of pre-hospital and emergency care for myocardial infarction. And this means that everyone, especially patients with coronary heart disease, should know the first signs of this acute heart pathology and the correct algorithm of action before the ambulance arrives.
The first signs of myocardial infarction
The onset of a myocardial infarction is signaled by the following symptoms:
- sudden or paroxysmal severe pain in the chest, lasting more than half an hour (up to 2 hours);
- the pain is burning, tearing, stabbing in nature, usually occurs after physical activity (sometimes immediately after sleep) and does not become less pronounced even after a state of rest;
- the pain is not eliminated (as during an attack of angina) by taking Nitroglycerin and after taking the pill (and even a repeat dose), a person may feel only a slight decrease in pain;
- severe weakness (up to pre-fainting or fainting);
- nausea;
- pain sensations radiate to the left (sometimes to the right) arm, neck area, interscapular area, teeth, scapula, lower jaw;
- severe pallor;
- the appearance of cold and sticky sweat on the skin;
- pronounced anxiety and fear of death.
Approximately half of patients with myocardial infarction experience signs of heart failure: difficulty breathing, shortness of breath, nonproductive cough, arrhythmic pulse, atrial fibrillation, sudden short-term cardiac arrest.
Video: What are the symptoms of myocardial infarction?
In some patients, the heart attack occurs in atypical forms. The following symptoms may indicate the occurrence of such an attack:
- pain in the left hand or little finger of the left hand, in the cervicothoracic spine, lower neck or lower jaw, scapula;
- pain localized in the abdomen and dyspepsia;
- suffocation and shortness of breath;
- shortness of breath with severe weakness and rapid increase in edema;
- dizziness with nausea, darkening of the eyes and a sharp decrease in blood pressure;
- dizziness with confusion, speech disturbances, nausea, vomiting and paresis of the arms and legs;
- discomfort in the chest area (without pain) with increased sweating and severe weakness.
In a number of clinical cases, a heart attack is represented by a combination of symptoms of several atypical forms (for example, cerebral and arrhythmic). Such manifestations of this life-threatening condition significantly complicate the detection of myocardial necrosis and aggravate the prognosis of the outcome of the emergency condition considered in this article.
When is it necessary to start performing first aid?
The answer to this question is always clear – immediately. That is, already when the patient began to show the first signs of myocardial infarction. Its onset is signaled by the following typical symptoms:
- intense chest pain;
- irradiation of pain to the left arm, shoulder blade, teeth or neck area;
- severe weakness;
- fear of death and severe anxiety;
- cold clammy sweat;
- nausea.
With atypical forms of heart attack, the patient may experience other symptoms:
- stomach ache;
- digestive disorders;
- vomit;
- dyspnea;
- suffocation, etc.
First aid in such situations should begin with calling an ambulance. When talking with the dispatcher of this service, you must:
- report the symptoms observed in the patient;
- express your assumption about the possibility of myocardial infarction;
- ask to send a team of cardiologists or resuscitators.
After this, you can begin to carry out those activities that can be performed outside the medical institution.
Emergency care before the ambulance arrives. What to do?
If you suspect a myocardial infarction, you should immediately call an ambulance and provide the dispatcher with the following information:
- about suspected myocardial infarction;
- describe the symptoms observed in the victim;
- ask for a team of cardiologists and resuscitators to arrive.
Before the arrival of specialists, it is necessary to immediately begin carrying out emergency assistance measures:
- Help the patient find a comfortable position: lay him on his back and place a cushion under the back of his head, or give him a semi-sitting position by placing a pillow or folded clothes, a blanket, etc. under his back.
- Unbutton and remove clothing or accessories (scarf, belt, tie, etc.) that interfere with free breathing, and ensure the most comfortable temperature conditions (for example, open a window in hot weather or cover with a blanket in the cold season).
- Explain to the victim that he must remain still and remain emotionally calm. You need to talk to a person in the state of an attack of myocardial infarction in an even, firm and calm tone, and you should not make sudden movements that could frighten him. If the patient has manifestations of motor agitation, then give him a sedative (tincture of valerian, motherwort, Valocardin, etc.).
- Measure blood pressure: if it is not higher than 130 mm Hg. Art., then give the patient a tablet of Nitroglycerin or another drug available under the tongue, the active component of which is organic nitrates (for example, Isoket, Nitrocor, Nitrogranulong, Izodinit in the form of sublingual tablets or spray). Before the doctors arrive, Nitroglycerin should be taken again 1-2 times (that is, 2-3 tablets can be given in total). If after taking the first dose of this drug the victim has a severe throbbing headache, then the subsequent dose should be halved. And if after taking Nitroglycerin there is a sharp decrease in blood pressure, then repeated use of this nitrate-containing drug should be discontinued. When using Nitroglycerin analogues (for example, medicine in the form of Izoket spray), each dose should be 0.4 mg. Before injecting the product, the first dose should be released into the air, as it may not be complete. After this, the patient must take a deep breath and hold his breath, then an injection is performed, the mouth is closed, and breathing for 30 seconds should be carried out only through the nose.
- To prevent blood clots, thin the blood and reduce the load on the heart muscle, give the patient up to 300 mg of crushed Aspirin.
- You can put a mustard plaster on the area where the pain is localized. Constantly monitor it so that the skin does not burn.
- Count the patient's pulse, and if he does not have a history of bronchial asthma, and the heart rate does not exceed 70 beats per minute, then give him 25-50 mg of Anetolol or a dose of any other beta-blocker (for example, Bisopropol, Propranolol, Nebivolol and etc.). This measure will reduce the risk of arrhythmia and sudden death, limit the area of necrosis of cardiac muscle tissue, protect the myocardium from toxic effects and increase its tolerance to stress.
Sometimes during an attack of myocardial infarction the patient faints. The following measures can help him in such situations:
- lay the patient on his back and place a cushion under his shoulders;
- remove dental structures from the mouth (if present);
- tilt the victim's head back or turn him to one side if the patient begins to vomit;
- ensure prevention of aspiration of vomit.
Remember! If a patient with signs of myocardial infarction has stopped his heart and breathing, or his breathing movements have become intermittent (agonal), then he should immediately begin performing cardiopulmonary resuscitation measures - chest compressions and artificial respiration.
Before resuscitation begins, a precordial blow is performed - 2 strong and short blows are applied to the sternum area (at the border of the middle and lower third) from a height of 20 - 30 cm. After their execution, the pulse is immediately felt. If it does not appear, then cardiopulmonary resuscitation (indirect cardiac massage and artificial respiration) is performed:
- pressing on the heart area with a frequency of 75 - 80 per minute;
- 2 breaths into the patient’s mouth after every 15 to 20 chest compressions.
The duration of such actions should be at least 10 minutes.
Pre-hospital emergency room
The standard for the arrival of an EMT team in the city is 10 minutes, outside the city limits - 20 minutes after registering a call with the dispatch service. If we take into account weather conditions, the epidemiological situation and the traffic situation, it is possible that the time may be exceeded (no longer than 10 minutes).
According to the protocol, the algorithm of the team’s actions upon arrival to the patient includes:
- Anamnesis collection (if possible).
- If necessary, perform resuscitation measures (ventilation, chest compressions, defibrillation).
- Conducting an examination and physical examination to assess the condition of the cardiovascular and respiratory systems.
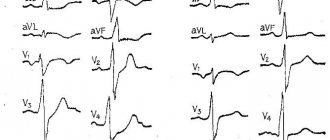
- Registration of 12 leads ECG with repeat after 20 minutes.
Pulse oximetry (if saturation is below 95% - oxygen support by mask or through nasal cannulas 3-5 l/min.).- Determine the level of troponins I, T in the blood (if a portable test is available).
- Providing venous access.
- Actually emergency medical care:
- Nitroglycerin 0.5-1 mg every 10 minutes. In case of severe pain, intravenous drip administration under the control of SBP (not lower than 90 mm Hg);
- relief of an anginal attack with narcotic analgesics. Preferably, Morphine 2-5 mg every 10-15 minutes until the pain stops (total dose not exceeding 20 mg);
- "ASA" 150-325 mg chewed, if the patient did not take it before the ambulance arrived;
- conducting dual antiplatelet therapy - Ticagrelor 180 mg, in its absence, Clopidogrel is prescribed at a dose of 300 mg;
- short-acting beta blockers - Propranolol, Metoprolol;
- reduce the load on the myocardium by lowering blood pressure and correcting hemodynamic disturbances.
If possible, it is recommended to carry out thrombolysis therapy TLT (streptokinase, alteplase, actilyse) at the prehospital stage. If thrombolysis can be carried out within 2 hours from the onset of ischemic changes (optimally within 60 minutes), this can interrupt the development of necrosis during MI, reduce the affected area and significantly reduce mortality. TLT is not effective if more than 12 hours have passed since the onset of the painful attack. Also, the procedure is not performed in the presence of absolute contraindications: intracranial bleeding or hemorrhagic stroke over the past 3 months, malignant brain tumor, abdominal aortic aneurysm with a tendency to dissection, bleeding from the gastrointestinal tract during the last month, disorders of the hemostatic system.
All patients with ACS are hospitalized in the intensive care unit of a specialized cardiology hospital with the ability to perform emergency angiography and reperfusion interventions.
First aid for myocardial infarction. Algorithm of actions
Emergency care for a patient after the ambulance arrives is carried out in the following sequence:
- Relief of acute pain with the help of non-narcotic and narcotic analgesics (solutions of Analgin, Morphine hydrochloride, Omnopon, Promedol) in combination with a solution of Atropine sulfate. The drugs are administered intravenously for faster pain relief.
- Carrying out an ECG.
- If delivery of the patient to the intensive care unit is possible within the next 30 minutes, then the victim is immediately taken to the hospital.
- If such rapid transportation of the patient turns out to be difficult, then drugs to restore coronary circulation (Tenecteplase, Alteplase, etc.) are administered on site.
- The patient is transferred to the ambulance as gently as possible - a stretcher is used for this. During transportation, humidified oxygen is inhaled.
After the patient is delivered to the intensive care unit, neuroleptanalgesia is administered to ensure complete relief of pain. For this purpose, medications such as Talamonal or a combination of Droperidol and Fentanyl are used. If the desired analgesic effect is not achieved, the patient is placed under inhalation anesthesia, which is provided by a mixture of oxygen and nitrous oxide.
Further, to provide first aid to the patient, the following drugs are prescribed:
- organic nitrates: Sodium isosorbide, Nitroglycerin, Isoket or others;
- anticoagulants: Heparin, etc.;
- antiplatelet agents: Acetylsalicylic acid, Cardiomagnyl, etc.;
- beta-blockers: Propranolol, Inderal, Obzidan, Anaprilin;
- ACE inhibitors: Enalapril, Ramipril, etc.;
- sleeping pills and sedatives: Temazepam, Diazepam, Triazolam, etc.;
- antiarrhythmic drugs: Lidocaine, Amiadron, Novocainamide, etc.
The treatment plan is drawn up individually for each patient. If necessary, other medications may be added to it.
To restore coronary circulation to a patient with severe forms of heart attack, the following surgical operations can be performed:
- balloon angioplasty;
- coronary artery bypass grafting.
Hospital treatment
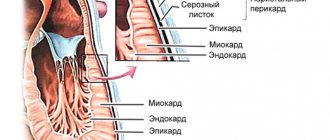
In the acute period, treatment of a heart attack is based on the leading syndromes; the main task of the doctor is to stabilize the patient’s vital functions and limit the spread of the lesion. Maximum possible resumption of coronary circulation. Prevention of complications.
- Pain relief is a simultaneous prevention of cardiogenic shock.
— If the pain persists, droperidol with fetanyl is re-administered after 30–40 minutes. These drugs have a side effect - respiratory depression. - Therefore, you can replace them with a mixture of analgin with Relanium or 0.5% novocaine; a mixture of analgin, diphenhydramine and promedol in 20 ml of physiological solution. These mixtures may have vomiting as a side effect; for prevention, a 0.1% atropine solution is administered subcutaneously. — If there is no effect, anesthesia with nitrous oxide.
- In case of asthmatic variant with pulmonary edema
The patient needs to elevate his upper body as much as possible. Three times with an interval of 2-3 minutes, nitroglycerin (isoket) under the tongue. Inhalation of oxygen with alcohol is effective. While waiting for the doctor, in the absence of oxygen, you can hold a cloth generously moistened with alcohol or vodka near the patient’s face (without closing the airways!). For high or normal blood pressure, Lasix (furosemide) is injected intravenously in large doses. For hypotension, prednisolone is administered intravenously and rheopolyglucin is infused drip-wise.
- For arrhythmias
Tachycardia (fast pulse) is stopped with isoptin solution. In the event of atrial fibrillation and flutter - novocainamide, panangin, unithiol. If there is no effect, electrodefibrillation is used. Bradycardia (rare pulse) - atropine is administered intravenously, izadrin 1 tablet under the tongue. If there is no effect, IV alupent and prednisolone.
- One of the reasons for coronary circulation disorders is their blockage with blood clots.
They are combated with medication using fibrolytic therapy based on streptokinase and its analogues. Contraindications to such therapy are all types of bleeding. Therefore, during this treatment, the patient’s condition is strictly monitored and platelet levels and blood clotting time are monitored.
Actions of a patient during a heart attack
Patients with coronary artery disease who are at risk of developing a heart attack should know not only the first signs of this dangerous condition, but also the algorithm of actions at the onset of such an attack:
- remain calm and take a “reclining” or “sitting” position;
- inform others about the onset of an attack and the need to take medications;
- if possible, call an ambulance yourself, informing the dispatcher about the development of a heart attack;
- try to move as little as possible;
- if you have medications, take 2-3 crushed tablets of Aspirin, Valocardin and Nitroglycerin;
- Describe symptoms to ambulance workers.
Video: First aid for yourself during a heart attack
After admission to the intensive care unit, the patient must follow all the doctor’s recommendations regarding medication, gradual expansion of physical activity and diet.
First aid for complications of myocardial infarction
In the absence of breathing, pulse in the vessels of the neck and graying of the skin, it is necessary to call emergency medical assistance, if this has not been done before, and immediately begin resuscitation measures. According to new recommendations from the American Heart Association, they should be carried out in the following sequence:
- Indirect cardiac massage. Place the patient on a flat and hard surface (floor, asphalt, etc.). Place the base of one of your palms in the place where the ribs meet on the chest, place the second palm on top and apply rhythmic pressure with your body weight. In this case, it is necessary to ensure that the sternum drops sufficiently deep (preferably 5 cm). 100 such movements should be performed per minute. After 30 compressions, you should switch to artificial respiration.
- Artificial respiration. All measures must be done promptly: the patient throws back his head, pushes his jaw forward, opens his mouth and closes his nose, then completely clasps the patient’s lips with his lips and blows air into his mouth (in order to protect against infections, preferably through a handkerchief or mask). In this case, the chest of the person being resuscitated should rise. You need to take 2 such artificial breaths, and then return to cardiac massage.
- Resuscitation should be continued until the doctors arrive, without reducing the rhythm and observing the ratio of pressure on the sternum and inhalations - 30 to 2.
Read also First aid for burns: types of burns and what to do in case of a burn.
The criteria for the effectiveness of the described measures are the improvement of the patient’s skin color, the appearance of spontaneous breaths, and pulse. Resuscitation can be stopped only when the person begins to breathe on his own.
Resuscitators also recommend that if it is impossible to perform artificial respiration (lack of skills and protective equipment - scarves, masks), only perform rhythmic and intense artificial heart massage until the medical team arrives. It is worth noting that first aid for a heart attack, provided correctly and without delay, especially cardiopulmonary resuscitation, can significantly increase the patient’s chances of survival.
Poor nutrition, bad habits and constant habits are the three most important factors that can disrupt the heart function of even the healthiest person. is the disease that kills the most people worldwide every year (7.4 million in 2012), and myocardial infarction is its most severe complication.
What if this happened on the street?
It happens quite often when a person becomes ill outside the home, and in this case it is quite difficult to find the necessary medicine. If trouble occurs, then it is necessary to carefully check the victim’s pockets or bag; as a rule, people suffering from heart disease always carry such medications with them.
How to give medicine to a patient? The use of the above-described drugs occurs according to the following scheme: the first nitroglycerin tablet is placed under the person’s tongue, and after 6 minutes the second is given, provided that the pain has not decreased.
How to distinguish a heart attack from angina pectoris
The problem is relevant even for cardiologists. It is impossible to carry out differential diagnosis on your own. Both processes are determined only approximately.
Specific signs of necrosis of cardiac structures:
- Acute pain. The discomfort is extremely intense. It radiates to the shoulder blade, back in general, neck, jaw, forearm, moves all the way to the hand. The force is so great that the patient may lose consciousness.
There is also a more insidious option. When the discomfort is moderate or mild, but obsessive, lasts more than half an hour. You need to remember: with angina, the pain is always pronounced, but not unbearable, lasting up to 30 minutes maximum.
Read also Sunburn: symptoms, first aid and treatment
In any case, the first action when persistent heart pain is detected should be to call an ambulance. You won’t be able to delimit states on your own.
- There is an effect of Nitroglycerin. But against the background of myocardial infarction it is incomplete, partial. The discomfort subsides, but does not go away. An attack of coronary insufficiency responds better to medications, so stable correction of the patient’s condition is possible. You need to listen carefully to how you feel.
- Severe arrhythmia. It occurs more often with necrosis of the heart muscle. Accompanied by typical disorders: freezing in the chest, turning over, tying a knot, missing blows. These are non-specific moments, so it is impossible to say exactly what caused it.
- Fainting conditions. Against the background of a heart attack, they are also more common.
- Severe shortness of breath. Inability to take in air, problems with the natural process. Panic and a feeling of fear are growing.
- Increased sweating. Almost never occurs during an attack. Against the background of necrosis, much more often. Speaks of a sharp drop in blood pressure and weakening of cardiac activity.
- Rate of progression. A heart attack is more aggressive and leads to health problems faster. In the fairer sex, it develops gradually, which is different from an attack of coronary insufficiency. In female patients, detection of pathology is easier.
In general, it is impossible to distinguish a heart attack from angina without special methods. And such differentiation is not of great importance at the prehospital stage.
In about 15% of emergency cases, there are no symptoms at all. The group at increased risk of developing a “silent” heart attack includes people over 50 years of age, patients with diabetes mellitus and arterial hypertension.
First aid to yourself
Algorithm of action for suspected necrosis of cardiac structures:
- Call an ambulance. Describe your own condition clearly, briefly and to the point. There is no need to embellish, let alone hide anything.
Brigades in Russia and the CIS countries are loaded to capacity, there are not enough doctors and even paramedics, so dispatchers are forced to rank situations by priority. The first to go are heart patients and children.
If you do not make clear the seriousness of the situation, there is a risk that you will have to wait for an ambulance for several hours. A heart attack does not tolerate such delays.
- Open a window or window. Acute necrosis of cardiac structures leads to the impossibility of adequate gas exchange.
The pulmonary artery and pulmonary vessels become stenotic (narrowed), hypoxia of all body tissues occurs due to a decrease in myocardial contractility.
If there is not enough oxygen in the atmospheric air, the situation will worsen. Cerebral ischemia and further progression of infarction are the most likely moments.
- Take a Nitroglycerin tablet, but only with your doctor's approval. The drug and its analogues partially help relieve pain.
It is not recommended to take Validol, Corvalol and phenobarbital-based pharmaceuticals as primary medications. They will not give a pronounced effect. Organic nitrates do not always act as desired.
Extensive heart attack is a contraindication to taking Nitroglycerin. Rapid development of arrhythmic disorders is possible. If there are no doctor’s instructions, then the best decision would be not to take anything until specialists arrive.
- Take a comfortable position. Horizontal orientation is associated with disruption of normal breathing. Asphyxia and other problems may occur. If you lose consciousness, vomit. Therefore, it is better to find a stable sitting position. The possibility of fainting is always taken into account.
- Remove constricting, tight clothing. Especially a collared shirt, T-shirt, etc. Compression of the carotid sinus, located in the neck, will lead to a reflex drop in heart rate. Given the current heart attack, this is almost guaranteed death.
- Calm down. An emergency condition is associated with the development of severe anxiety and fear. This is a so-called panic attack. At such moments, obsessive thoughts, mental and motor agitation arise.
You should call an ambulance if you have any suspicions. Signs of a heart attack in women are described here, and in men - here. False modesty costs lives. Neither heart attack nor angina can be treated at home.
Unconventional method of therapy
For the treatment and prevention of coronary heart disease and myocardial infarction, hirudotherapy - treatment with leeches - is used with great success. Prescribe from 4 to 8 pieces of leeches to the heart area 2 to 4 times with an interval of 2-3 days.
Leech saliva contains a special enzyme that slows down blood clotting and prevents the formation of blood clots.
Infection and suppuration of bite sites are not observed, since hirudia have bactericidal properties. Hirudotherapy is contraindicated for diseases accompanied by increased bleeding. Author:
Selezneva Valentina Anatolyevna general practitioner
3 comments
- Gulya
05/17/2014 at 09:18First, it is necessary to carry out antiparasitic cleansing of the body and only then treat any disease. If doctors approached treatment from this position, there would not be so many diagnoses.
Reply to comment
- Elisha
01/20/2018 at 15:22
After eating there is pressure on the left side, under the rib, what is the reason for this?
Reply to comment
- Klim
02.11.2018 at 17:27
Myocardial infarction is one of the clinical forms of coronary heart disease, occurring with the development of ischemic necrosis of a portion of the myocardium, caused by absolute or relative insufficiency of its blood supply. It occurs only in those who do not cleanse the intestines and do not cleanse the body. It occurs when the intestines are clogged and food without fistal and others digestive tablets are not suitable, since the intestines are full of foreign bodies and cause food rejection, reflux and heartburn and flatulence and the food is not digested, that is, it simply rots in the digestive tract. By the smell of flatulence, you can determine that the food is rotting, that is, by the rotten smell. a person with with such a disease, he is very lazy, cowardly and complex, as a result of which he tries to stay away from doctors and if he catches their eye, he doesn’t say much about himself for fear that the doctors will put an enema into the intestines or somewhere else
Reply to comment
Helping another person
The situation is much more complicated with primary measures for a third-party patient. If the victim complains of severe chest pain, you should immediately call an ambulance. Tell about the condition, suggest the development of necrosis of the heart muscle.
Further:
- Help sit the person down. Laying is not recommended for the reasons already mentioned. Asphyxia due to pulmonary edema and/or vomiting. Possible death before specialists arrive. And beyond cardiac reasons.
- Give Nitroglycerin for mild pain. In general, it is better to refrain from using the drugs unless there is a clear indication from the treating cardiology specialist. The permissible dosage when prescribed by a doctor is 1 tablet. Additional use of aspirin is possible, again according to indications.
- Open the window, window. If the patient is at home or indoors. Move the patient to a warm place when the condition develops in the winter season. In summer there is no need. But place a cloth or clothing under the person so that there is no direct contact with the cold ground or asphalt.
- Calm the person down. Do not allow intense movement. Physical activities affect your heart rate. Excessive stimulation of cardiac structures leads to a greater aggravation of the ischemic process.
- If possible, measure your heart rate.
Differential diagnosis
It is very important to know how to distinguish a heart attack from a regular attack of angina, which also manifests itself as severe chest pain. The most important criteria are the duration of pain and the effect of nitroglycerin, which the patient takes under the tongue.
So, during an attack of angina, the pain lasts no more than five minutes, and is quite easily relieved with one (maximum two) doses of nitrates. In case of a heart attack, even taking nitrates three times does not bring relief to the patient.
The diagnostic tactics here are as follows: sharp pain in the chest - take one dose of nitroglycerin under the tongue > after five minutes the pain persists > another dose of nitroglycerin under the tongue > after five minutes the pain persists > call an ambulance, as a heart attack is likely to develop.
If the patient is unconscious
The algorithm is slightly different:
- Move the person to a safe place. For example, when the patient is close to the road or highway.
- Call out and gently shake your shoulder. Try to get out of syncope in this way.
- Check your pulse. Against the background of the current heart attack, vascular vibrations in the wrists and neck will be minimal.
- Assess the nature of breathing, its presence. You need to lean in and listen.
- Free your tongue. In a faint state, it can lodge in the throat and block the airways.
- The head is carefully turned to the side. In case of vomiting, so that food masses and gastric contents do not provoke aspiration and death from asphyxia.
In case of cardiac arrest
Direct massage is recommended.
Open palms are folded and placed on top of each other. Hands are placed on the chest, in the center, in the hollow area. Press rhythmically at a speed of 100-120 movements per minute.
The force should be sufficient to displace the chest 5 cm in depth.
Clinical first aid guidelines suggest that rib fractures are not a reason to stop massage.
It is better not to do artificial respiration. Without a well-developed skill, the method will be of no use, and valuable time will be lost.
Massage itself is a physically exhausting process. Every 2-3 minutes it is recommended to change with others. You can gain useful experience after completing the relevant courses.
Upon arrival of the team, resuscitation measures are stopped. It is necessary to inform the medical personnel about the condition, also if there have been changes in blood pressure, heart rate - vital indicators.
Primary diagnostic measures - assessment of cardiac activity and breathing - should take no more than 2-3 minutes.
No longer recommended, risks are too high, time is running out. If necessary, it is possible to accompany the person to the emergency department. Especially if it is an elderly relative or a mentally ill person. The issue is resolved on an individual basis.
A little more about terminology
Currently, acute coronary syndrome refers to two conditions that manifest similar symptoms:
Unstable angina
Unstable angina is a condition in which, against the background of physical activity or rest, pain appears behind the sternum, which has a pressing, burning or squeezing nature. This pain radiates to the jaw, left arm, left shoulder blade. It may also manifest itself as abdominal pain and nausea.
Unstable angina is said to occur when these symptoms are either:
- just arose (that is, the person previously performed exercise without heart pain, shortness of breath or discomfort in the abdomen);
- began to occur at less load;
- become stronger or last longer;
- began to appear alone.
Unstable angina is based on a narrowing or spasm of the lumen of a larger or smaller artery that supplies, respectively, a larger or smaller area of the myocardium. Moreover, this narrowing must be more than 50% of the diameter of the artery in this area, or the obstacle in the path of blood (this is almost always an atherosclerotic plaque) is not fixed, but fluctuates with the blood flow, sometimes blocking the artery more or less.
Myocardial infarction
Myocardial infarction - without ST segment elevation or with ST segment elevation (this can only be determined by ECG). It occurs when more than 70% of the diameter of the artery is blocked, as well as in the case when “flying off” plaque, blood clot or drops of fat clog the artery in one place or another.
Acute coronary syndrome without ST segment elevation is either unstable angina or non-ST segment elevation infarction. At the stage before hospitalization in a cardiology hospital, these 2 conditions are not differentiated - there are no necessary conditions and equipment for this. If ST segment elevation is visible on the cardiogram, a diagnosis of “Acute myocardial infarction” can be made.
The treatment of acute coronary syndrome depends on the type of disease - with or without ST elevation.
If the ECG immediately shows the formation of a deep (“infarct”) Q wave, a diagnosis of “Q-myocardial infarction” is made, rather than acute coronary syndrome. This suggests that a large branch of the coronary artery is affected, and the focus of dying myocardium is quite large (large-focal myocardial infarction). This disease occurs when a large branch of the coronary artery is completely blocked by a dense thrombotic mass.
What you should absolutely not do
The following actions are prohibited:
- Engage in physical activity. In some cases, myocardial infarction manifests itself as bradycardia. The heart rate decreases.
Particularly proactive people begin to do squats and push-ups. This is absolutely impossible to do. Heart rate will increase due to reflex stimulation of cardiac activity, but at what cost?
Myocardial contractility decreases, blood flow weakens. The increased frequency of contractions will only make the situation worse. The risk of death will increase dramatically.
- Take medications. The issue of a possible emergency condition and self-care methods is discussed with a cardiologist. If he allows you to take Nitroglycerin, it is permissible to drink it. In other cases, the condition may worsen. The same applies to Aspirin and other medications.
- Wash with cold water. Low temperature exposure to facial tissue will lead to reflex vasoconstriction. Including coronary ones. This is the body's natural response to an intense stimulus. The nutrition of cardiac structures will weaken. Is it worth saying how the hearts will react to such a process? You can’t wash your face with hot or even warm water.
- Panic, nervous. A negative emotional background will lead to the release of large amounts of cortisol, adrenaline and other stress hormones. Including angiotensin, renin. They will lead to stenosis (narrowing) of blood vessels, coronary arteries. The nutrition of the heart and body tissues will weaken. This will increase the likelihood of death or, at a minimum, accelerate the progression of myocardial infarction.
- Eating. You cannot eat because you are likely to develop vomiting. When you lose consciousness, a reflex process occurs. This body response is the result of cerebral ischemia. Aspiration of gastric contents and death from asphyxia are possible.
- Try to cope on your own. It is necessary to call an ambulance. This is an axiom. Provided that the patient still plans to live. Because without hospitalization the chances tend to zero.
- If someone else is hurt, don’t shake the person. Trying to bring him to his senses, hitting him on the cheeks. Such methods are good for cinema, but are strictly contraindicated in real life. Injuries to the cervical spine, vomiting, and other dangerous situations are possible.
Read also First aid for road traffic accidents
If a car is available, the patient is transported to the hospital on their own. This is only advisable if the institution is located nearby or there is a chance of quick transportation.
What do doctors do at first?
Emergency care for myocardial infarction is not a method of treatment, but a path to maintaining the minimum possible vital activity and slowing down the process.
The first thing paramedics or doctors do is assess the objective condition of a person. Sometimes it gets to the point of absurdity, and they try to find out the well-being of unconscious people, but this is rather an exception to the rule.
Blood pressure and heart rate are measured. Auscultation provides information about chest sounds.
The number one task for doctors is to partially stabilize the patient’s condition and take him to the hospital. The person is then placed in intensive care.
Impact measures are conservative. The following drugs are used:
- Epinephrine, Adrenaline. They artificially stimulate cardiac activity. Particularly relevant for critical drops in blood pressure and significant bradycardia of less than 50 beats per minute. In other cases, use is strictly contraindicated. The pathological process may worsen.
- Antispasmodics. Relieves excess muscle stiffness, partially restores blood flow, and eliminates pain.
- Beta blockers. To equalize heart rate. Specific names are determined by specialists. If the patient is accompanied by a relative, it is worth informing about the presence of cardiac or vascular diseases and talking about the prescribed therapy regimen. This will help you get your bearings.
- Calcium antagonists. To ensure normal myocardial contractility.
- Non-narcotic and narcotic, opioid painkillers. Analgesics are used if the patient is conscious to provide relief. Because it is extremely painful for a person to bear.
- Nitroglycerine. Only if there are no contraindications. It is usually prescribed at the pre-hospital stage by the ambulance specialists themselves.
Attention:
It is prohibited to use cardiac glycosides and antiarrhythmic medications. They will cause cardiac arrest and death. The likelihood of complications is high, so considerable experience and qualifications are required.
First aid for myocardial infarction provides a good prognosis for the course and outcome of the pathological process. In the absence of competent support, the chances of survival drop sharply.
Taking specialized courses is a good investment in the future. Including in the event of an emergency condition developing in the person himself or his loved ones.
Further diagnostics in the hospital
After the arrival of medical workers, the patient must undergo an ECG, regardless of complaints and the severity of the condition. Any medical professional must know what signs of ischemia and acute myocardial damage look like on a cardiogram. This is the “back of the cat” that any medical student can recognize.
If an emergency doctor diagnoses a heart attack, he immediately transports the patient to a specialized cardiology or therapeutic hospital, either to the RSC (regional vascular center) or to the PSO (primary vascular department). In the first minutes after diagnosis, the patient receives intensive medical care - this includes adequate pain relief, including the administration of narcotic drugs, this includes the administration of anticoagulants to prevent thrombus formation in a clogged coronary artery, and the administration of thrombolytics to quickly dissolve an existing thrombus in the affected coronary artery. arteries, and symptomatic therapy.
But this treatment is carried out only by doctors, but how can you help a person before the ambulance arrives?
Possible complications of myocardial infarction
Experts divide the complications of a heart attack into early and late:
| Type of complications of myocardial infarction | When do they arise? | Types of complications |
| Early | In the first hours or days (in the first 3-4 days) after an acute attack |
|
| Late | Occurs against the background of increased motor activity of the patient 14–21 days after an acute attack |
|
Depending on the nature of the damage and disorders, complications of a heart attack are classified as follows:
| Type of complications | Nature of damage and violations |
| Mechanical |
|
| Electrical (or arrhythmic) | occur in almost 90% of patients and manifest themselves in different types of arrhythmias. |
| Ischemic |
|
| Thromboembolic |
|
| Inflammatory |
|
The most severe complications of myocardial infarction include:
- recurrent or prolonged course;
- pulmonary edema;
- areactive or true cardiogenic shock;
- clinical death;
- acute right ventricular failure;
- atrioventricular block at any location of the necrosis zone;
- acute cardiac aneurysm;
- thrombosis and thromboembolism in various organs;
- circulatory failure IIB and III degrees;
- ventricular paroxysmal tachycardia;
- gastrointestinal bleeding;
- a combination of two or more complications.
Surgery
After achieving a stable condition, restoration of normal heart rhythm, and other vital signs, surgical treatment is performed according to indications in order to restore the patency of the coronary vessels. The following interventions are currently being carried out:
- Stenting is the introduction of a metal frame (wall) into the narrowed areas of the coronary vessel. During this operation, the chest is not opened; a special probe is inserted into the desired location through the femoral artery under the control of an X-ray machine.
- CABG – coronary artery bypass grafting. The operation is performed on an open heart, its essence is that it creates an additional possibility of blood supply to the affected area by transplanting the patient’s own veins, creating additional paths for blood flow.
Indications for surgical treatment and the choice of type of intervention depend on the results of coronary angiography:
- damage to two arteries out of three, or the degree of narrowing is more than 50%
- presence of post-infarction aneurysm
The patient's motor regimen is of great importance in the treatment of myocardial infarction. In the first period, from 1 to 7 days, strict bed rest is recommended, in which, from the moment a stable condition is achieved, it is recommended to perform passive movements while lying in bed, and breathing exercises under the supervision of medical personnel. Further, as the condition improves, it is recommended to constantly expand physical activity daily by adding active movements (turning, sitting up in bed, eating independently, washing, etc.).
In the second period, when transferred to ward mode, the patient is allowed to get up, walk first near the bed, then along the corridor, gradually increasing the load. In the corridors of cardiology departments there are special markings for therapeutic walking, which indicate the day of illness; the patient must walk this distance daily. The patient switches to complete self-care.
In the third period, the patient is given a free regime, gradually switching to a rehabilitation and training regime in a sanatorium.
Diet
Recommendations for a patient’s nutrition are approached individually, depending on the patient’s condition, laboratory parameters (cholesterol level), and body weight. Patients are recommended 4-5 meals a day. If the cholesterol level exceeds the norm, restrictions are imposed on the consumption of egg yolk, brains, liver, and caviar.
One third of the fats consumed should be vegetable fats. Cholesterol levels are reduced if the menu includes foods rich in pectin (apples, bananas); the content of a large amount of dietary fiber is of great importance, which inhibits the absorption of cholesterol in the intestine and maintains a stable level in the bile. Criteria for discharge of a patient with myocardial infarction from the hospital:
- relief of the main symptoms of the disease
- self-service option
- sufficient resistance to physical activity (the patient can climb one flight of stairs without deterioration and take walks of 0.5 to 3 km in several sessions during the day)
Psychological rehabilitation
In patients after myocardial infarction, a personal reaction to the disease, fears for the outcome of the disease, and future prospects for personal and social life may persist for up to 4 months. If the patient is not provided with timely psychological assistance, the following may occur:
- Neuroses, which are characterized by increased irritability, sudden mood swings, sleep disorders, and obsessive fears.
- Or the hypochondriacal development of the personality - “going into illness”, the patient requires special attention, since he considers himself on the verge of death, while objectively his condition is satisfactory.
Psychological rehabilitation is aimed at returning the patient to work and restoring his status in the family.
Potential Risks
In case of myocardial infarction, experts identify the following potential risks:
| Primary | Secondary |
|
|